Published online Dec 6, 2022. doi: 10.12998/wjcc.v10.i34.12711
Peer-review started: August 18, 2022
First decision: October 12, 2022
Revised: October 25, 2022
Accepted: October 31, 2022
Article in press: October 31, 2022
Published online: December 6, 2022
Processing time: 106 Days and 11.9 Hours
Ureteral-iliac artery fistula is a rare disease resulting from the pathological connection between the ureter and iliac artery, with artificial iliac artery-ureteral fistula being rarer. Iliac artery ureteral fistula is challenging to diagnose, and the misdiagnosis and mortality rates are high.
A case of artificial iliac artery ureteral fistula was reported in this paper. The patient was a 69-year-old male with paroxysmal painless hematuria. The artificial iliac artery ureteral fistula was diagnosed by angiography. The hematuria was stopped after intravascular embolization, and no bleeding occurred after 6 months of follow-up.
Ureteral arterial fistula should be considered when inconspicuous hematuria with previous iliac vessels is encountered in addition to local ureteral surgery history. A rapid endovascular approach is recommended for fistula identification.
Core Tip: Ureteral-iliac artery fistula is a rare disease resulting from the pathological connection between the ureter and iliac artery, with artificial iliac artery-ureteral fistula being rarer. Iliac artery ureteral fistula is challenging to diagnose, and the misdiagnosis and mortality rates are high. A case of artificial iliac artery ureteral fistula was reported in this paper. The patient was a 69-year-old male with paroxysmal painless hematuria. The artificial iliac artery ureteral fistula was diagnosed by angiography. The hematuria was stopped after intravascular stent implantation, and no bleeding occurred after 4 mo of follow-up.
- Citation: Feng T, Zhao X, Zhu L, Chen W, Gao YL, Wei JL. Ureteral- artificial iliac artery fistula: A case report. World J Clin Cases 2022; 10(34): 12711-12716
- URL: https://www.wjgnet.com/2307-8960/full/v10/i34/12711.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i34.12711
Iliac-ureteral fistula is a rare disease resulting from a pathological connection between the ureter and iliac artery. This usually results in hematuria after blood vessels, aneurysms, or artificial blood vessels connect with the urinary collection system. The occurrence of the iliac artery-ureteral fistula is often associated with degenerative iliac artery disease or any previous involvement of artery reconstruction surgery. Additionally, its occurrence is also closely related to pelvic surgery (malignant tumor resection, urinary diversion, radiotherapy, ureteral stent implantation, etc.)[1,2].
Unfortunately, the disease is difficult to diagnose, resulting in a high misdiagnosis rate and a mortality rate as high as 38%[3]. Furthermore, cases of ureteral- artificial iliac artery fistula are exceedingly rare. This report represents the only case encountered in our hospital. In this case report, we describe our angiography observation to improve our understanding of the disease, avoid misdiagnosis, and provide evidence for clinical treatment.
A 69-year-old male presented to our hospital with intermittent painless gross hematuria for 3 d.
Gross haematuria was observed in the urine and presented as bright red, accompanied by blood clots, intermittent attacks, frequent micturition, no urgency, pain and discomfort, no cramping pain, no fever, and chills. On the third day after admission, the patient's haematuria suddenly became worse, and the color was bright red for a total volume of about 500 mL. The bladder was continuously washed.
He had a history of “abdominal aortic stenosis”. Therefore, abdominal aorta and iliac vessel repla
The patients denied any family history of similar diseases.
Upon admission, physical examination demonstrated that vital signs were stable, and no obvious abnormality was found in the cardiopulmonary physical examination.
Hemoglobin was 130 g/L on admission on April 11, platelets and white blood cells were within the normal range, and urine routine showed red blood cell 92/HPF. At 06:55 on April 14, hemoglobin dropped to 98 g/L, and the hemoglobin concentration rose to 104 g/L after interventional therapy.
The results of contrast-enhanced computed tomography of the urinary system, computed tomography urography, and computed tomography angiography (CTA) examination showed that the left renal pelvis and left ureter were dilated, and patchy high-density shadow could be seen inside (Figure 1). However, no enhancement was found in the enhanced scan, except for the possibility of bleeding. At the same time, clots were considered due to the high-density shadow in the bladder. Dilatation and pseudoaneurysm may be seen in the lower abdominal aorta. Cystoscopy showed bright red blood spraying from the left ureteral orifice.
The final diagnosis was the ureteral- artificial iliac artery fistula.
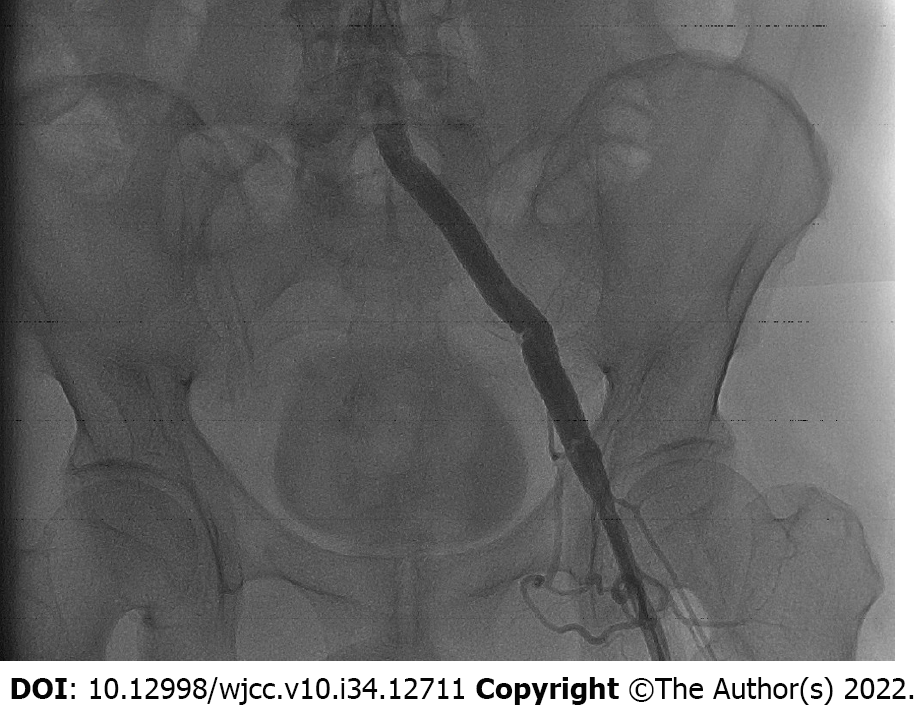
Due to the progressive decrease of hemoglobin concentration in patients, interventional embolization was performed with local anesthesia. There was no obvious abnormality in the left renal artery conventional angiography intraoperative, and the contrast extravasated in the left common iliac artificial blood vessel (Figure 2). An intravascular embolization was given, and no sign of contrast extravasation was found in re-angiography (Figure 3), consistent with the rupture of the left common iliac artificial blood vessel.
The hematuria of the patients was diminished immediately after the operation, and the blood routine test showed no apparent change in hemoglobin concentration compared with before. After being treated for 3 d, the patients were discharged from the hospital and had no recurrence after 6 mo of follow-up.
As early as 1908, Moschcowitz reported the first case of iliac artery-ureteral fistula, which occurred after bilateral ureteral calculi[4]. The pathogenesis of this disease is often due to the pathological changes in iliac vessels and complications related to local radiotherapy and surgery between iliac vessels and ureter, leading to the pathological connection between the ureter and iliac artery. The patient in this report has a history of previous abdominal aortic and iliac vascular replacement, long-term replacement of ureteral stent after the operation, and transureteral holmium laser lithotripsy for left ureteral calculi, having two risk factors mentioned above. Some studies suggest that most iliac arterial ureteral fistulas are caused by the mechanical force of arterial pulsation on the ureter where the stent is placed, which leads to necrosis of the artery and ureteral wall, and finally forms ureteral arterial fistula[3]. For this patient, according to the author's analysis, on the one hand, the direct injury of the local ureter and artificial blood vessels is caused by long-term ureteral stent replacement and holmium laser lithotripsy. In contrast, when an artificial iliac blood vessel is replaced, the dissociation and reconstruction of the ureter and iliac artery junction during operation leads to normal local anatomical changes. However, the friction between the artificial blood vessel and ureter is increased compared with human own blood vessels, thus further increasing the risk of the disease.
The clinical manifestations of the iliac artery ureteral fistula mainly include hematuria, urinary retention, fever, low back pain, and discomfort[3]. Among them, gross hematuria is the most common clinical manifestation of the iliac artery-ureteral fistula, which often occurs intermittently. Additionally, it may be intermittent with local thrombosis at the lesion or occlusion of a ureteral stent. In severe cases, a large amount of gross hematuria may occur, which may result in hemorrhagic shock. The patient's gross hematuria showed intermittent attacks of bright red color, accompanied by blood clots. After admission, a large amount of gross hematuria occurred, accompanied by urinary bladder retention. A blood routine showed that hemoglobin decreased from 130 g/L to 118 g/L within 15 min, suggesting that there was an obvious possibility of massive bleeding in the body. Therefore, the formation of iliac artery-ureter fistula should be highly suspected in patients with sudden unexplained hematuria, especially those with a history of the iliac vessel and ureter-related surgery.
Due to the complex nonspecific and temporary clinical manifestations of ilia-ureteral fistula, diagnosis can often be delayed, leading to disease progression and life-threatening conditions. Therefore, awareness and accurate diagnosis are of utmost importance. Currently, the diagnostic methods are mainly based on computed tomography (CT), CTA, and selective arteriography, and the diagnostic rate of CT is only 42%-50%[5]. The diagnostic rate is further reduced when the arterial and ureteral fistula is small. Simultaneously, blood accumulation above the renal pelvis and fistula may occur if the blood flow pressure of the ureteral fistula is high enough. Consequently, this may result in the illusion of upper urinary tract bleeding, thus misleading clinicians to make an incorrect diagnosis and treatment plan. Due to the CT scan results suggesting dilatation and hematocele of the renal pelvis and ureter, upper urinary tract bleeding was mistakenly advised, and nephrectomy was performed. Therefore, the diagnostic rate of CT alone has substantial limitations. Although angiography is an invasive examination, its diagnostic rate is 72.4% higher than that of CT. On the other hand, when there is a permanent stent or thrombus in the ureter and blockage and leakage, the contrast medium may not enter the ureter[6]. CT of the urinary system of this patient also suggested the possibility of bleeding in the left kidney and middle and upper left ureter. Additionally, CTA found no lesion. Further angiography showed no evident leakage of contrast medium in the left kidney but an apparent overflow of contrast medium in the left iliac common artificial blood vessel. Therefore, angiography is preferred for diagnosing the iliac artery and ureteral fistula, and CT and CTA are needed for auxiliary diagnosis.
Ureteral arterial fistula is endangered, and severe hematuria can cause hemorrhagic shock. Commonly used treatment methods include: suturing fistula, placing arterial patch or ligation for vascular bypass surgery, endovascular stent implantation or embolization, endovascular stent implantation combined with ureteroscopy, and percutaneous nephrostomy combined with ureteral embolization[7]. Although open surgery is the gold standard for treating ureteral arterial fistula, the advantages of open surgery include more intuitive operation and accurate hemostasis effect of suture, the proportion of transvascular interventional treatment of ureteral arterial fistula is gradually increasing with the rapid development of interventional radiology. The benefits of its use are that it can improve diagnostic rates and results in a shorter recovery time since it is a minimally invasive method. In this case, an intravascular stent was grafted through the left femoral artery under local anesthesia. After the operation, the patient's hematuria significantly improved, and he was discharged the third day following the procedure.
In addition to a history of local ureteral surgery and associated radiotherapy radiotherapy history ureteral fistula should be considered when inconspicuous hematuria with previous iliac vessels is detected. Angiography in combination with CTA can be effective in determining diagnosis. A rapid endovascular approach recommended for fistula identification, which requires collaboration among urologists, vascular surgeons and interventionists. Due to the rarity of the ureteral arterial fistula, the type and frequency of complications following endovascular repair are unknown. Therefore, patients' vital signs should be closely monitored after surgery and rigorous follow-up should be considered.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Boopathy Vijayaraghavan KM, India; Syahputra DA, Indonesia S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Luther B, von Lilien-Waldau V, Mamopoulos A, Katoh M, Friedrich M, Weinknecht S, Lent V. [Ureteroarterial fistula - pathogenesis, diagnostics, and therapeutic outcome]. Aktuelle Urol. 2014;45:204-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Bergqvist D, Pärsson H, Sherif A. Arterio-ureteral fistula--a systematic review. Eur J Vasc Endovasc Surg. 2001;22:191-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 117] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 3. | Das A, Lewandoski P, Laganosky D, Walton J, Shenot P. Ureteroarterial fistula: A review of the literature. Vascular. 2016;24:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Moschcowitz AV. IX. Simultaneous Ligation of Both External Iliac Arteries for Secondary Hemorrhage. Ann Surg. 1908;48:872-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | van den Bergh RC, Moll FL, de Vries JP, Lock TM. Arterioureteral fistulas: unusual suspects-systematic review of 139 cases. Urology. 2009;74:251-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 78] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Pillai AK, Anderson ME, Reddick MA, Sutphin PD, Kalva SP. Ureteroarterial fistula: diagnosis and management. AJR Am J Roentgenol. 2015;204:W592-W598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Fernandopulle CL, Jeyaraj R, Alchanan R, Huang DY. Ureteroarterial fistula: imaging diagnosis and endovascular management. BMJ Case Rep. 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |