Published online Dec 6, 2022. doi: 10.12998/wjcc.v10.i34.12696
Peer-review started: July 28, 2022
First decision: September 27, 2022
Revised: October 11, 2022
Accepted: November 2, 2022
Article in press: November 2, 2022
Published online: December 6, 2022
Processing time: 127 Days and 3.3 Hours
The treatment of large pelvic masses in postmenopausal women is a challenge in clinical practice. Although ultrasound or magnetic resonance imaging can be used to determine the size and location of the mass, it is still difficult to achieve a preoperative diagnosis. The majority of cellular leiomyomas are diagnosed by histopathology after surgery. We report the differential diagnosis and surgical management of a rare case of cellular leiomyoma in the broad ligament of the uterus.
A 52-year-old Chinese woman without sexual history was admitted to the First Affiliated Hospital of Guangzhou University of Chinese Medicine for the first time. The patient had a 1-year history of progressive abdominal enlargement as well as a 2-year history of menopause, and complained of frequent abdominal pain and low-grade fever. Computed tomography of the abdomen showed a solid cystic mass (29.4 cm × 18.8 cm × 37.7 cm) in the pelvis and abdomen. Moreover, routine blood test results indicated a baseline cancer antigen 125 (CA-125) level of 187.7 U/mL and C-reactive protein of 109.58 mg/L. Subsequently, retrograde hysterectomy and bilateral adnexectomy were performed in this patient. On histopathologic examination of the surgical specimen, a rare cellular leiomyoma in the broad ligament was diagnosed.
Clinicians need to constantly improve diagnosis and treatment for the challenges posed during clinical assessment, differential diagnosis, and surgical management.
Core Tip: Initially, a gynecological malignancy was suspected due to an elevated tumor blood index and large abdominal mass of unknown nature in this unmarried, childless middle-aged woman. The importance of differential diagnosis in this case was crucial and removal of the mass was also challenging. We performed an unconventional hysterectomy to ensure a smooth operation, which indicates the importance of surgical choice.
- Citation: Yan J, Li Y, Long XY, Li DC, Li SJ. Giant cellular leiomyoma in the broad ligament of the uterus: A case report. World J Clin Cases 2022; 10(34): 12696-12702
- URL: https://www.wjgnet.com/2307-8960/full/v10/i34/12696.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i34.12696
Cellular leiomyoma arising in the broad ligament of the uterus is extremely rare, with only five cases reported to date. Furthermore, the preoperative diagnosis of cellular leiomyoma poses a great challenge for clinicians. On the one hand, its clinical presentation is similar to that of ovarian cancer, such as enlargement of abdominal masses and increased tumor markers (CA-125) after the menopause[1]. On the other hand, all cellular leiomyomas in the broad ligament were diagnosed by intraoperative observation and postoperative pathology. In our study, the sixth case of giant cellular leiomyoma in the broad ligament with cystic and mucinous lesions is reported.
The patient had recurrent abdominal distension for 1 year, accompanied by left upper abdominal pain for 4 d.
Due to low-grade fever and abdominal pain for 4 d, the woman was admitted to the emergency department of the First Affiliated Hospital of Guangzhou University of Chinese Medicine.
Except for congenital neurofibroma accompanied by local pigmentation throughout the body and prominent skin with scattered small masses, she had no specific previous medical history.
The patient was a 52-year-old Chinese postmenopausal woman who was unmarried and childless, without a sexual history. She had no drug history or family history. In addition, the patient had no history of smoking or drinking.
Abdominal examination revealed an abdominal mass corresponding to the abdominal size at 37 wk gestation (located below the xiphoid process). Anal examination revealed a large solid cystic mass with well-defined borders in the pelvic abdomen.
An elevated baseline CA-125 level of 187.7 U/mL was observed.
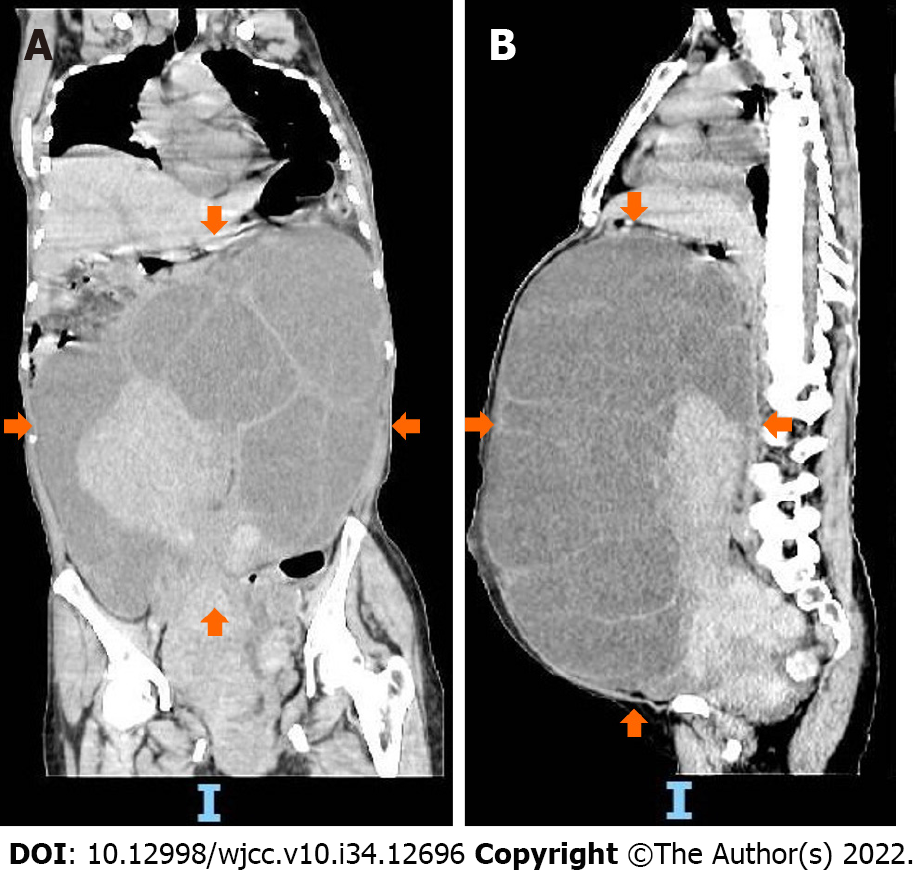
As shown by computed tomography (Figure 1), a solid cystic mass (29.4 cm × 18.8 cm × 37.7 cm) was found in the pelvis and abdomen (Figure 2).
Right broad ligament uterine leiomyoma.
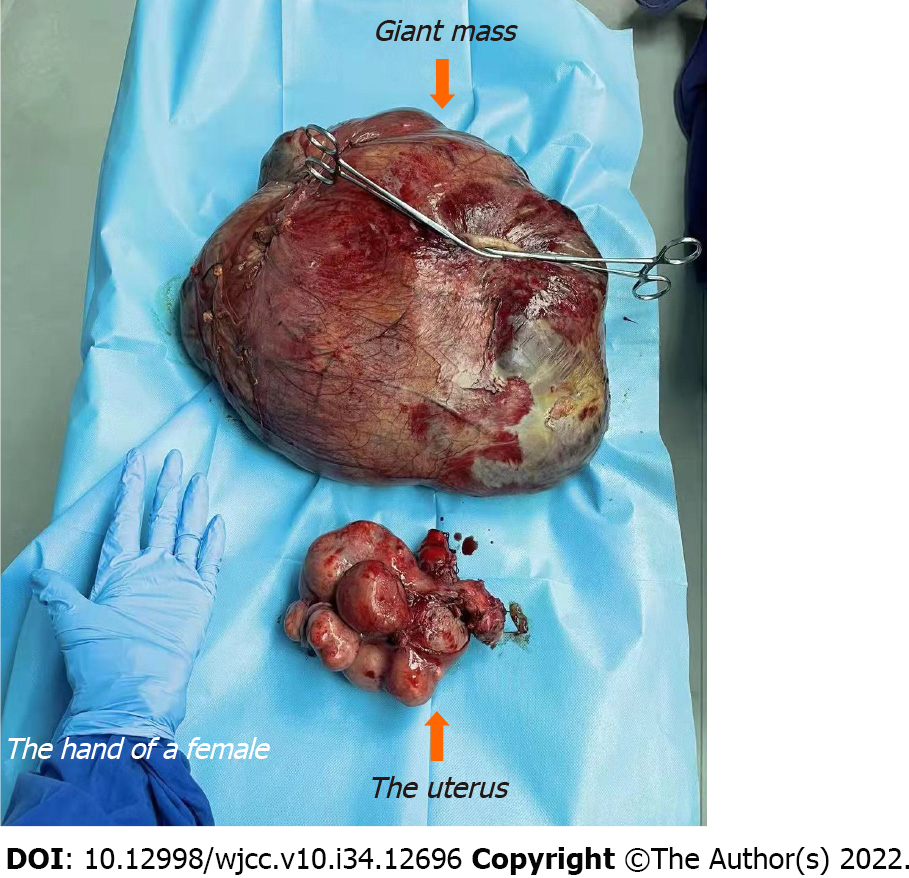
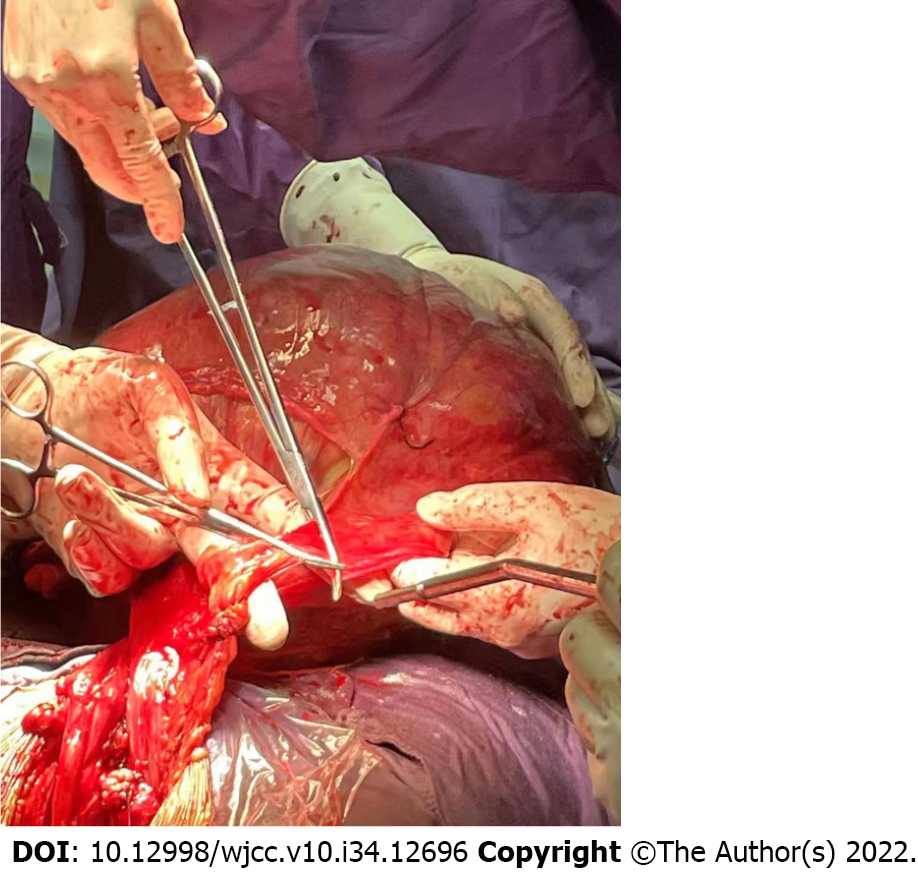
The patient successfully underwent retrograde abdominal hysterectomy and bilateral adnexectomy (Figure 3 and Video).
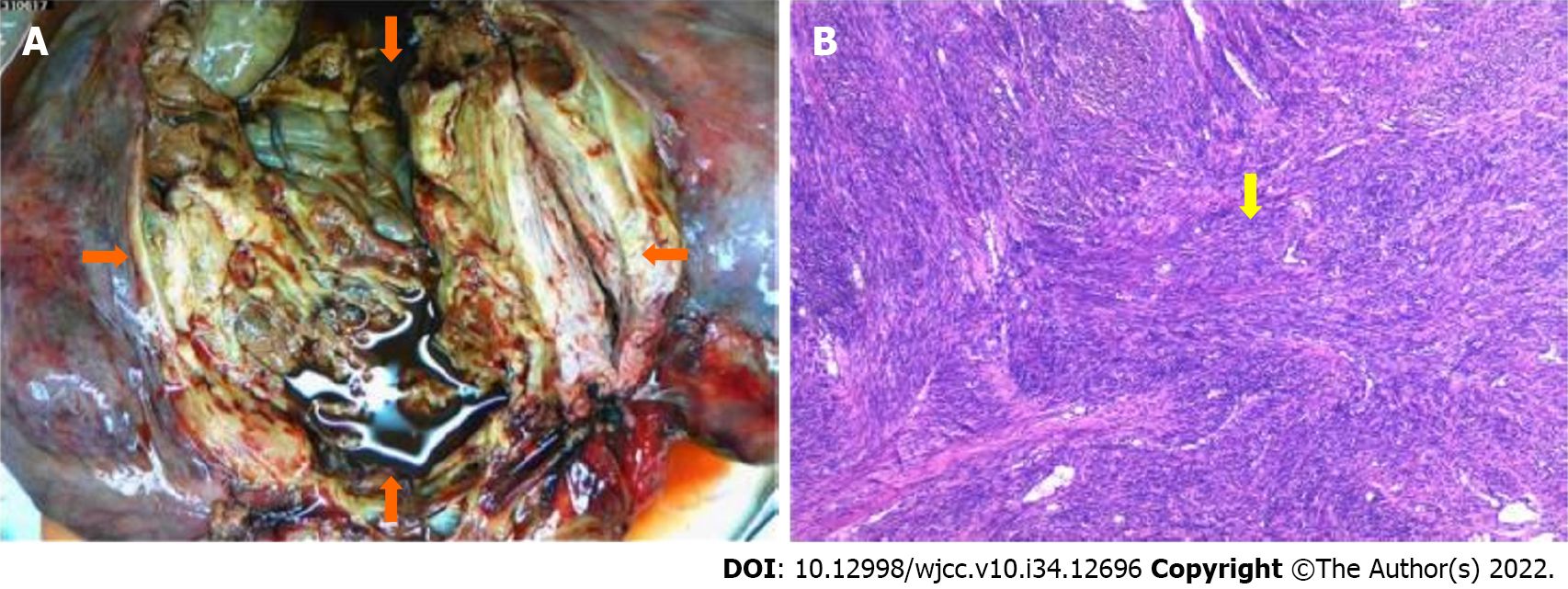
The surgical samples were sent for histopathological examination, and the results showed that the uterine mass was composed of proliferating smooth muscle cells and arranged in a braided shape; the cell morphology was slightly changed and no abnormalities were observed (Figure 4).
Leiomyoma, the most common benign uterine tumor[2], presents no obvious symptoms in many women with fibromas. Only patients who have symptoms affecting the function of the tumor-adjacent organ, such as urinary frequency and urgency, constipation, pain, or cancer-related anemia will opt to visit the clinic. Given the complex pathogenesis of uterine leiomyoma, its etiology is unclear at present. As revealed by clinical observations and laboratory tests, both estrogen and progesterone are involved in regulating the growth of uterine fibroids[3]. In addition, sex hormone level is an essential contributor to uterine fibroids. Several studies have shown that the incidence of hormone-dependent uterine leiomyoma is approximately 70% in women of childbearing age[4] and 80% in 50-year-old women[5]. Uterine fibroids form inside the uterus and are rarely found outside the uterus. In terms of their histomorphological features, uterine fibroids are mainly classified into intramural fibroids, submembranous fibroids, and submucosal fibroids[6]. Of these histopathological forms, cellular leiomyoma in the broad ligament is the least common type of uterine fibroid (< 5%)[7,8]. The broad ligament contains embryonic remnants formed by mesonephric (Wolffian) ducts. Notably, Wolffian ducts give rise to the genital ducts in males, but contract to generate embryonic remnants. These remnants including epithelial and paracellular cells, may spread and form abnormal cysts, or produce some myofibers that can lead to leiomyomas within the broad ligament[9]. To date, only five cases of cellular leiomyoma in the broad ligament have been reported in the literature[7,10-12]. The comprehensive assessment and diagnosis in these studies were mainly conducted with the aid of tumor markers, ultrasonography and histopathological examination. Nevertheless, little information on cellular leiomyoma in the broad ligament is available due to its rare occurrence. It is easily confused with the diagnosis of ovarian malignancies; therefore, posing a great challenge for clinicians and pathologists to increase the accuracy of preoperative diagnosis of cellular leiomyoma in the broad ligament.
Patients with cellular leiomyoma in the broad ligament are diagnosed at an advanced stage, with the main clinical manifestations of an abdominal mass, abdominal distension, and ascites. In line with the findings of previously reported cases, our patient presented with elevated CA-125 levels. However, CA-125 is not a specific marker for cellular leiomyoma in the broad ligament, and is increasingly expressed in endometriosis and serous ovarian tumors, which therefore increases the difficulty of preoperative diagnosis[1]. These findings also imply that all cellular leiomyomas in the broad ligament are currently diagnosed by intraoperative observation and postoperative pathology. Accordingly, it is worth mentioning that exploratory laparotomy is the most effective method for making a diagnosis.
In this case, ring ligation was performed by an attending physician with more than 30 years of clinical surgical experience. Attention should be paid to protecting vital tissues and organs such as the bladder, ureter and major blood vessels during the operation. The tumor was distinctly different from the ovary (Figure 5). Given its complete and clear capsule, the tumor can be preliminarily distinguished from ovarian tumors. Nonetheless, histopathology is the gold standard and should be performed. Postoperative pathological examination of the myometrial wall and bilateral ovaries revealed acute suppurative inflammation, and recurrent low-grade fever in patients may be associated with endogenous fever factors such as tumor growth. In the present case, successful surgical intervention was critical to the patient’s prognosis.
The mass in this patient was so huge that the bladder was moved upward and the boundaries of the interstitial space were unclear. Thus, choosing a conventional hysterectomy had higher risks, such as poor hemostasis and excessive intraoperative bleeding. Collectively, we finally chose retrograde total hysterectomy through the Douglas pouch to inhibit bleeding and effectively dissect the uterovesical space. Specifically, the cervix and vagina were exposed in the posterior fornix; blood flow was blocked in each branch; and the uterus was finally removed after blunt dissection of the uterine space from below to above the level of the bladder triangle.
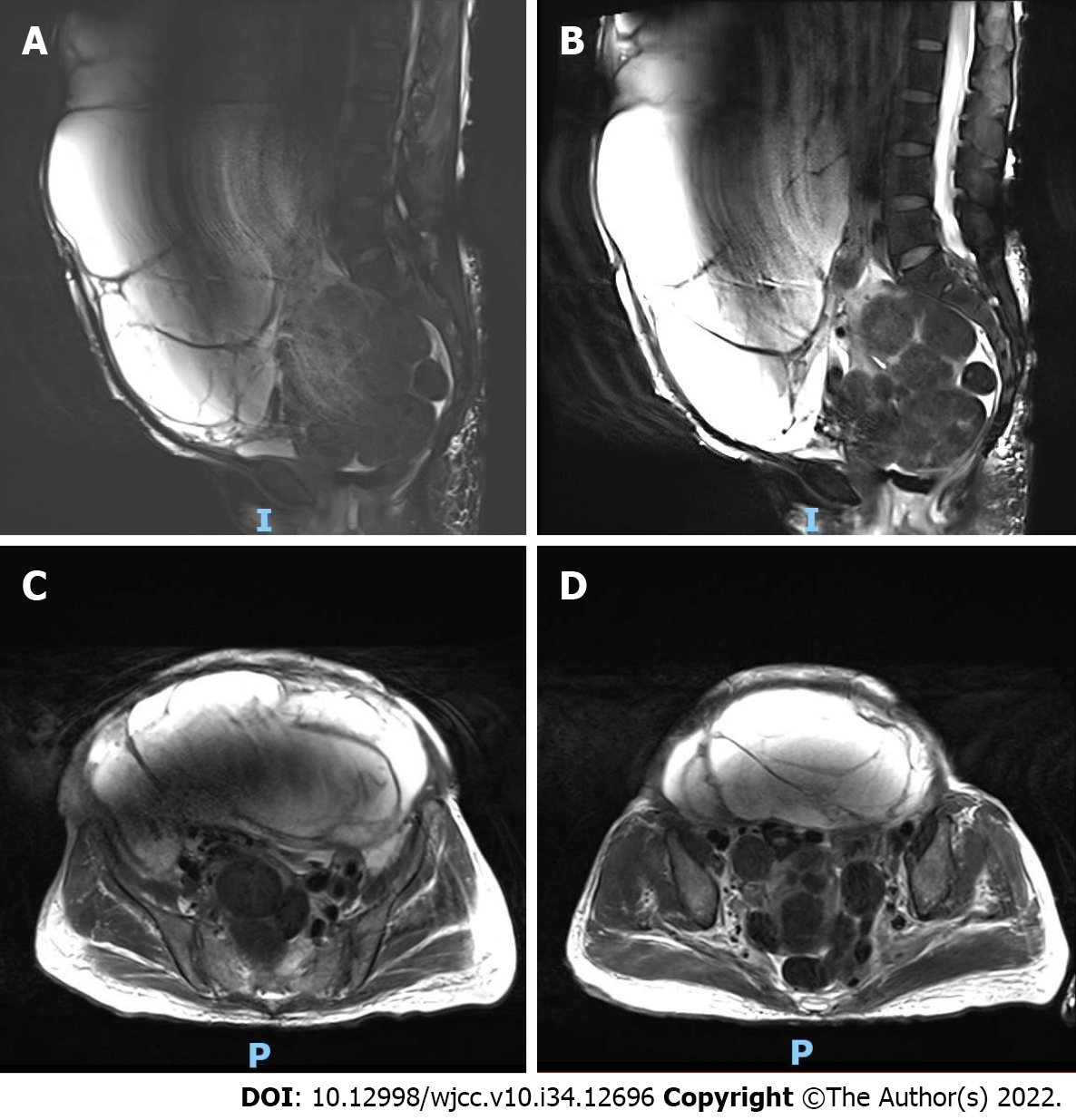
In addition, hyalinization is the most common secondary phenomenon. With the development of hyaline fibroids, cysts of various sizes are generated after liquefaction and necrosis of muscle cells. This was concluded by reviewing the cases from 2016 and 2020. Thus, large masses were associated with cystic and myxoid lesions. Cystic leiomyomas displayed decreased T1 signal intensity and increased T2 signal intensity (no increase observed in the cystic lesion area) on MRI, while common leiomyomas exhibited lower T2 signal intensity. This provided a method for the clinical differentiation of common leiomyomas and cystic leiomyomas[12].
Cellular leiomyoma, a variant of leiomyoma, is one of the most special types of uterine leiomyoma. In the study conducted by Naz et al[13] of 964 female genital leiomyomas, cellular leiomyomas were discovered to be the most common variant of leiomyomas, but they were easily confused with malignancy due to their specificity. Therefore, the application of bioinformatics to predict relevant specific tumor biomarkers is particularly important for preoperative diagnosis and prognosis. In light of the rarity of this disease, it is crucial to address this issue with additional research using animal models in future studies.
Giant cellular leiomyoma in the broad ligament is a rare clinical neoplasm. The probability of it being confused with ovarian malignancy is increased by elevated CA-125 levels, as well as cystic and mucinous lesions. Timely and successful surgical intervention is critical for patients indicated for surgery.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gislinge JIP, Denmark; Hegazy AA, Egypt S-Editor: Liu JH L-Editor: Webster JR P-Editor: Liu JH
| 1. | Mallick D, Saha M, Chakrabarti S, Chakraborty J. Leiomyoma of broad ligament mimicking ovarian malignancy- report of a unique case. Kathmandu Univ Med J (KUMJ). 2014;12:219-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Jagtap SV, Khatib WGM, Jagtap SS, Kshirsagar NS. Large leiomyoma of the broad ligament. Journal of Medical and Allied Sciences. 2013;3. [DOI] [Full Text] |
| 3. | The North American Menopause Society (NAMS). NAMS 2018 Utian Translational Science Symposium, October 2018, San Diego, California New therapies for leiomyomas: when surgery may not be the best option. Menopause. 2019;26:947-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 4. | Machado-Lopez A, Simón C, Mas A. Molecular and Cellular Insights into the Development of Uterine Fibroids. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 5. | Lewis TD, Malik M, Britten J, San Pablo AM, Catherino WH. A Comprehensive Review of the Pharmacologic Management of Uterine Leiomyoma. Biomed Res Int. 2018;2018:2414609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 6. | Bajis R, Eloundou G. Unusual Case of a Torted Mesenteric Fibroid. Case Rep Obstet Gynecol. 2018;2018:8342127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Chmaj-Wierzchowska K, Buks J, Wierzchowski M, Szymanowski K, Opala T. Leiomyoma cellulare in the broad ligament of the uterus--case report and review of literature. Ginekol Pol. 2012;83:301-304. [PubMed] |
| 8. | Lodhia J, Gaffur R, Sadiq A, Amsi P, Tsandiraki J, Maro E. Unusual case of broad ligament leiomyoma: A diagnostic and surgical challenge. Clin Case Rep. 2022;10:e6350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Kagan II. Traditions and peculiarities of clinical anatomy education in Russia. Clin Anat. 2002;15:152-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Sharma P, Zaheer S, Yadav AK, Mandal AK. Massive Broad Ligament Cellular Leiomyoma with Cystic Change: A Diagnostic Dilemma. J Clin Diagn Res. 2016;10:ED01-ED02. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Sikora-Szczęśniak DL. Leiomyoma cellulare in the broad ligament of the uterus. Prz Menopauzalny. 2018;17:49-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Jha S, Singh A, Singh S, Murmu S. Huge broad ligament leiomyoma with cystic degeneration: A diagnostic and surgical challenge. J Obstet Gynaecol Res. 2020;46:791-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Naz S, Rehman A, Riyaz A, Jehangir F, Naeem S, Iqbal T. Leiomyoma: Its Variants And Secondary Changes A Five-Year Study. J Ayub Med Coll Abbottabad. 2019;31:192-195. [PubMed] |