Published online Dec 6, 2022. doi: 10.12998/wjcc.v10.i34.12690
Peer-review started: July 21, 2022
First decision: October 12, 2022
Revised: October 22, 2022
Accepted: November 4, 2022
Article in press: November 4, 2022
Published online: December 6, 2022
Processing time: 134 Days and 1.6 Hours
Most case reports on laryngeal granuloma formation have described patients after tracheotomy and single-lumen endotracheal intubation. Few studies have investigated vocal cord granuloma formation after double-lumen endotracheal (DLT) intubation.
We report granulation tissue formation on the bilateral vocal cords after DLT intubation in a 45-year-old, 153-cm-tall female patient. Previous imaging reports showed no formation of vocal cord granuloma before DLT intubation. Therefore, we inferred that DLT intubation may have been the main reason for the postoperative granulation tissue formation on her bilateral vocal cords, based on the patient’s history of DLT intubation, persistent hoarseness after thoracic surgery, and fibrolaryngoscopic and pathological reports during 12 mo follow-up.
Thirty-two Fr DLT tubes should be utilized for thoracic surgery on female patients who are shorter than 153 cm in height.
Core Tip: Most case reports on laryngeal granuloma formation have been reported on patients after tracheotomy and single-lumen endotracheal intubation. Few studies have investigated vocal cord granuloma formation after double-lumen endotracheal (DLT) intubation. We reported a case of a 45-year-old woman with granulation tissue formation of the bilateral vocal cords after lobectomy with DLT. We found that a 32 Fr DLT tube should be selected for thoracic surgery for female patients below 153 cm in height. This study is intended to act as a reference for those seeking to identify people at a high risk of developing airway granulomas and lower the frequency of such complications.
- Citation: Xiong XJ, Wang L, Li T. Formation of granulation tissue on bilateral vocal cords after double-lumen endotracheal intubation: A case report. World J Clin Cases 2022; 10(34): 12690-12695
- URL: https://www.wjgnet.com/2307-8960/full/v10/i34/12690.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i34.12690
Double-lumen endotracheal (DLT) intubation is now widely applied in thoracic surgery for most cases of lung isolation and perioperative one-lung ventilation. However, compared with single-lumen endotracheal (SLT) intubation, the DLT tube is stiffer. It has a larger external diameter and is more likely to cause postoperative complications[1], such as airway granuloma formation. Previous studies suggested that incidences of granuloma after SLT intubation are rare[2]. Most case reports on laryngeal granuloma formation have been reported on patients after tracheotomy and SLT intubation. There are few case reports on vocal cord granuloma formation after DLT intubation. We report a case of a 45-year-old woman with granulation tissue formation on the bilateral vocal cords after lobectomy with DLT intubation.
A 45-year-old woman of a height of 153 cm and weighing 49 kg, who was an employee of the sales industry, was admitted to our department. She complained of nodules in the right upper lobe that had been observed during a routine physical examination 1 mo previously.
During anesthesia induction, midazolam (2 mg), etomidate (20 mg), sufentanil (25 µg), and cisatracurium (10 mg) were administered intravenously. A left 35 Fr DLT tube (PVC; Wellhead, China) was inserted orally and smoothly with an ordinary laryngoscope. Then, endotracheal intubation was performed by an anesthesiologist with 1 year of experience, and the position of the DLT tube was examined carefully by fiberoptic bronchoscopy. The patient underwent thoracoscopic wedge resection of the right lower lobe without re-positioning the DLT tube.
After surgery, her respiratory signs, muscle strength, and consciousness recovered well, and after 80 min intubation, the DLT tube was removed. The patient experienced hoarseness for 1 mo after discharge but did not seek any medical remediation.
She denied having a history of hypertension, diabetes, surgery, drug or food allergies, drug use, smoking, alcohol consumption, or a family history of vocal granuloma formation. The patient had no preoperative complaints of sore throat, hoarseness, cough, or gastroesophageal reflux.
She denied having a history or a family history of vocal granuloma formation.
According to the Classification System of the American Society of Anesthesiologists, Mallampti II, her physical status included a normal thyromental distance and a low risk of airway difficulty.
According to preoperative laboratory examinations, she had no history of syphilis, acquired immune deficiency syndrome, or other infectious diseases.
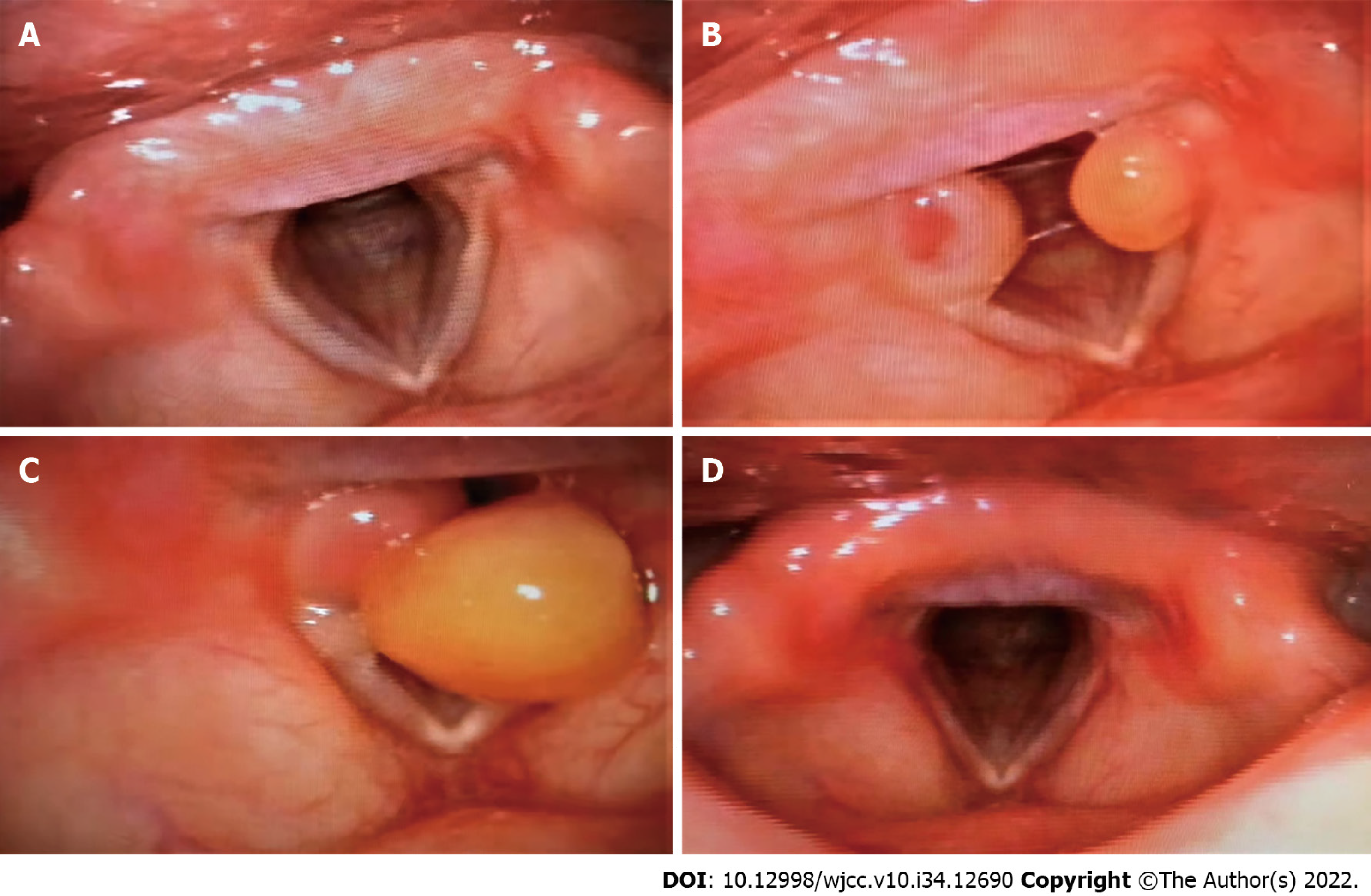
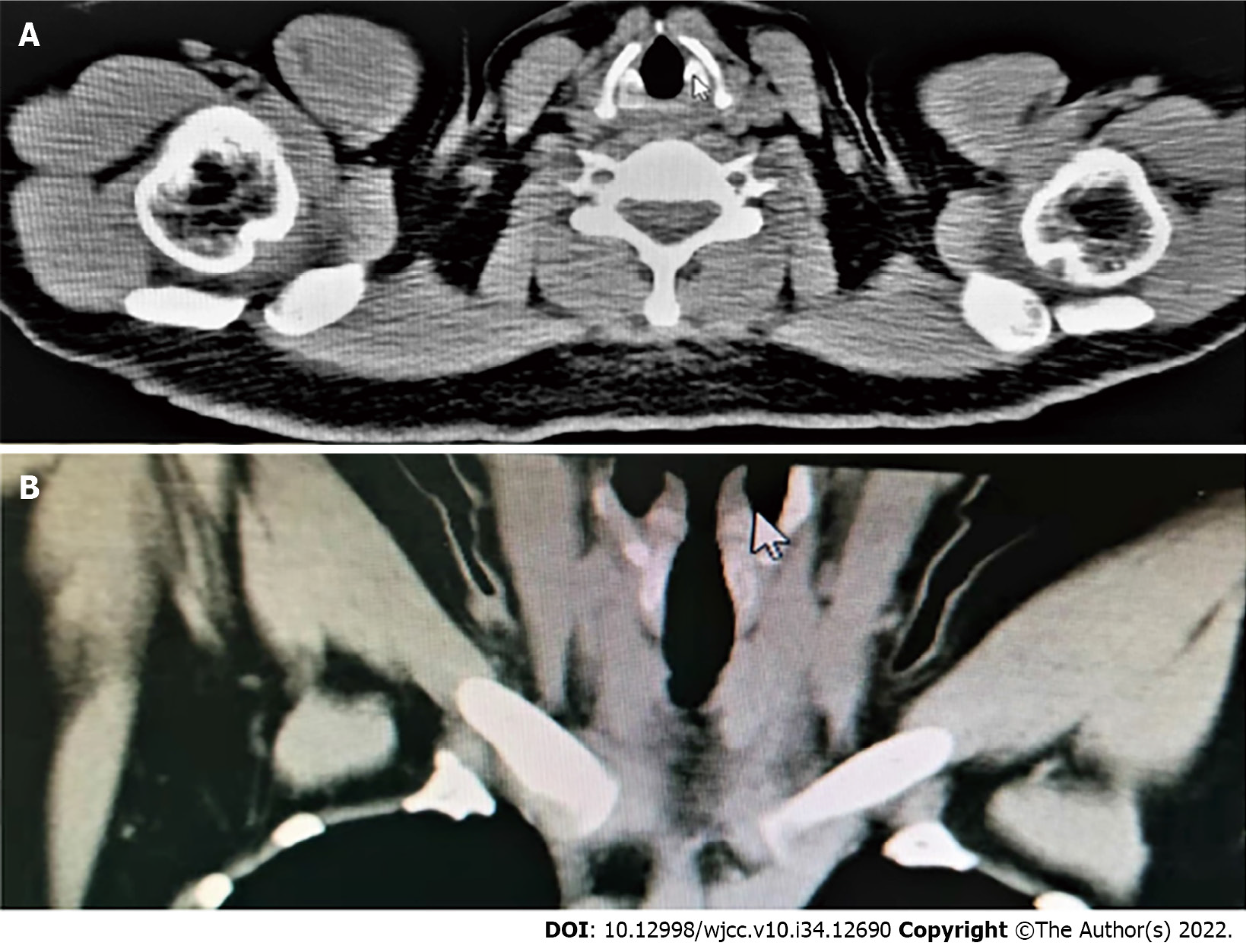
She underwent fibrolaryngoscopy due to "snoring and dry mouth" 7 mo before the thoracic surgery, and no significant abnormalities were observed (Figure 1A). There was no neoplasm of the glottis on preoperative chest computed tomography (Figure 2). A repeat fibrolaryngoscopy revealed her bilateral vocal cords to be slightly swollen, with a smooth surface, normal motility, poor closure, and granulation tissue protrusions in the bilateral arytenoid region (Figure 1B). Later, her bilateral vocal cords became more swollen under fibrolaryngoscopy. Granulation was observed in the bilateral arytenoid area, and the area of granulation of the right vocal cords (Figure 1C) was larger than that in the previous examination (Figure 1B) and virtually blocked the glottis. On day 105 after thoracic surgery, during follow-up, a fibrolaryngoscopy showed no granulation tissue formation at the glottis (Figure 1D).
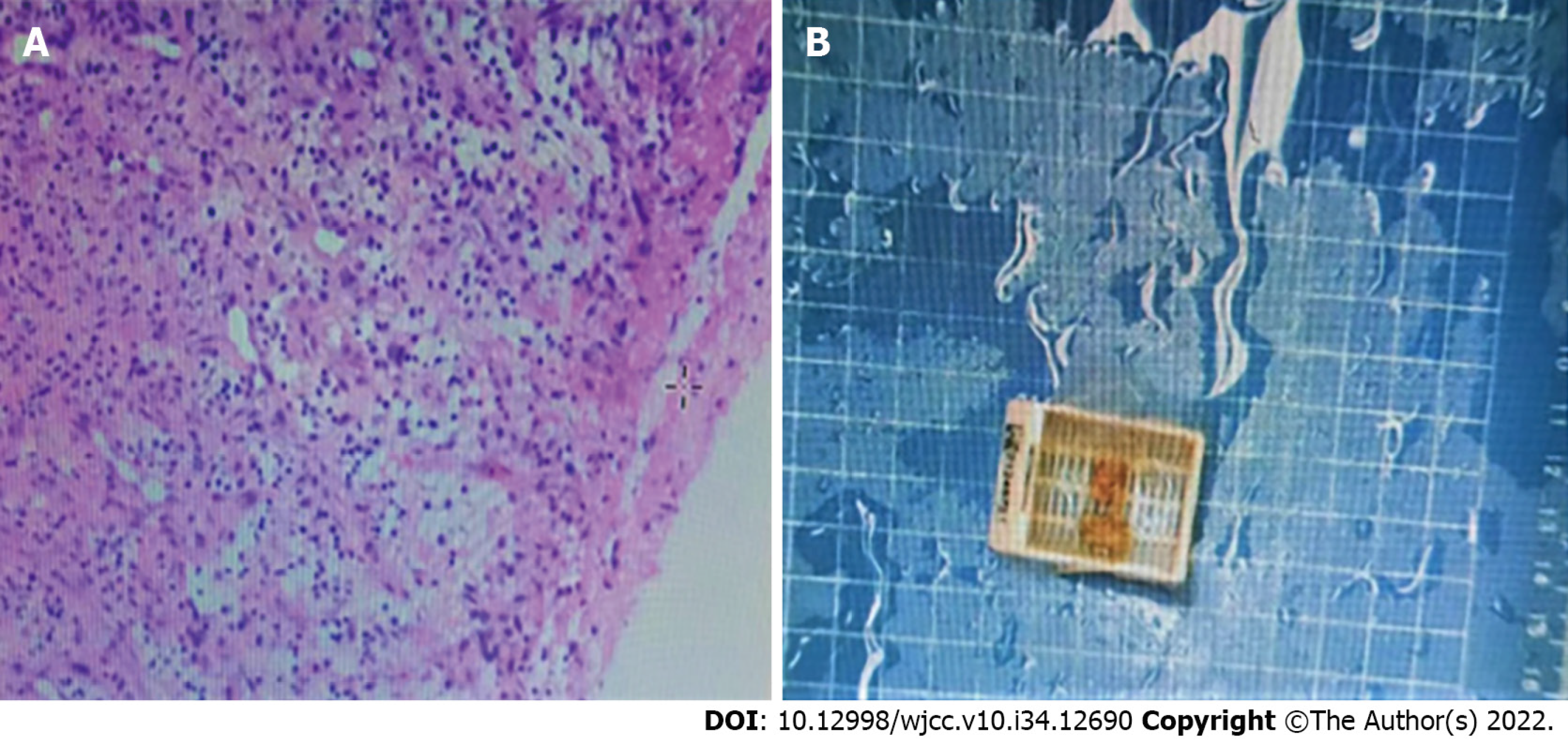
Pathological investigation of the resected lesion revealed neoplasms and polyps on both vocal cords and a large amount of granulation tissue (Figure 3).
On day 51 after thoracic surgery, she experienced intermittent and recurrent episodes of hoarseness, especially after excessive talking, accompanied by laboured speech and mild dyspnea. However, the symptoms failed to diminish after the patient received medicine for 10 d (montelukast, 10 mg, qd and methoxyphenamine, 25 mg, po tid). She noted worsening hoarseness and dyspnea on postoperative day 73. Therefore, she received resection of the bilateral vocal cord lesion with supporting laryngoscopy on day 75 after thoracic surgery.
On day 105 after thoracic surgery, during follow-up, a fibrolaryngoscopy showed no granulation tissue formation at the glottis (Figure 1D).
Laryngeal granulomas are benign and nontumorous, and unilateral/bilateral lesions are more likely to develop in the posterior third of the vocal cords, specifically the vocal processes of the arytenoid cartilage, but also occur in the posterior and lateral parts of the cricoid cartilage in the subglottic larynx[3]. According to Poiseuille’s law, minor changes to the diameter of the laryngotracheal stem and the length of the narrowed segment result in significant variations in airflow. Hoarseness occurs when the airway size reduces by 30%; dyspnea occurs when the airway shrinks by 80%, and severe airway size reduction can lead to difficulty breathing and swallowing and voice alterations[4]. Treatment of vocal cord granuloma is primarily conservative, either through the amelioration of irritation or the use of medication[3,5]. Surgical excision is rare and only adopted in severe cases[5].
This is the first paper on the granulation tissue formation of vocal cords after DLT intubation, supported by imaging and pathological reports during follow-up. In this case, the causes of pos
The DLT tube is a curved endobronchial tube that has the potential to cause harm to the patient[5]. DLT tubes are often made of PVC materials with an oblique cut at the end, which increases the risk of touching the vocal cords during intubation and extubation. Laryngeal injury caused by direct pressure from the endotracheal tube can result in mucosal ulceration and inflammation, leading to granuloma formation[5]. In addition, the high pressure applied by balloon cuffs or tubes surpasses the capillary pressure, posing the risk of loss of local blood flow and the inducement of local ischemia or necrosis[6]. The fibrinolytic pathway is thus stimulated, generating a proliferative phase, characterized by angiogenesis, collagen deposition, and granulation tissue formation, followed by a phase of maturation and remodeling with membranous web-like stenosis[6].
One previous study suggested that 32 Fr DLT intubation might only be appropriate for women shorter than 153 cm[7]. However, we selected a 35 Fr left DLT tube for our female patient, who was 153 cm tall. The distance between the trachea and the bronchial cuff was 10.1 cm vs 10.3 cm between the glottis and carina. D’Anza et al[8] found that, in both men and women, the tracheal cross-sectional area increased with height. Gelbard et al[9] concluded that the passage of oversized endotracheal tubes through the commonly smaller female trachea might contribute to tracheal injury and subsequent stenosis. At a given depth, the cuff fitted more tightly in the trachea, closer to the vocal cords, and was associated with mucosal tracheal compression over a longer segment[10]. Therefore, the DLT main tracheal cuff was probably positioned at the vocal cords. Once inflated, the cuff could have easily compressed the vocal cords.
Female patients are prone to developing intubation-related granulomas and account for 75%-90% of all cases[11]. This is because of their narrower and lower glottis and thinner arytenoid cartilage[12] compared to men.
Excessive use of the vocal cords and chronic cough are predisposing factors for forming granulomas after intubation[3]. Traumatic collisions of the vocal cords occur during absurd pronunciation, and a chronic cough can cause stress to the vocal cords after intubation. Therefore, the cricoidal cartilage epithelium may be injured, and tissue healing delayed[3,13]. Our patient, a sales woman, might have overused her vocal cords during work after surgery. Unfortunately, she did not receive proper or prompt treatment after experiencing hoarseness.
In this case, fibrolaryngoscopy showed that the polyp on the right vocal cord, which almost blocked the glottis, was larger than the polyp on the left. The right vocal cord was at risk of granulation tissue formation when the tube tip injured it. This can be explained by the fact that most endotracheal intubation operators carry the laryngoscope handle in their left hand while using their right hand to perform the intubation procedure[14]. Furthermore, we also suggest that DLT should perform by an anesthesiologist experienced in endotracheal intubation.
During follow-up, the patient admitted that she should have sought medical advice when she experienced persistent hoarseness 1 wk after her thoracic surgery. She was also reminded of her elevated risk of airway granulomas. We noted that a smaller and softer DLT tube should be used in further potential thoracic surgery.
According to our observations and assessment, female patients of a short stature (less than 153 cm) are considered high-risk for the formation of vocal cord granulomas after DLT intubation. Therefore, for female patients shorter than 153 cm, a 32 Fr DLT tube should be selected.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jha P, United States; Thongon N, Thailand S-Editor: Wei ZH L-Editor: A P-Editor: Wei ZH
| 1. | Seo JH, Cho CW, Hong DM, Jeon Y, Bahk JH. The effects of thermal softening of double-lumen endobronchial tubes on postoperative sore throat, hoarseness and vocal cord injuries: a prospective double-blind randomized trial. Br J Anaesth. 2016;116:282-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 2. | Naito K, Iwata S, Nishimura T, Takasu A, Kuwauchi T, Yaida M. Nine cases with postintubation granuloma of the larynx. Auris Nasus Larynx. 1982;9:111-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 3. | Rimoli CF, Martins RHG, Catâneo DC, Imamura R, Catâneo AJM. Treatment of post-intubation laryngeal granulomas: systematic review and proportional meta-analysis. Braz J Otorhinolaryngol. 2018;84:781-789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Hast MH. The developmental anatomy of the larynx. Otolaryngol Clin North Am. 1970;3:413-438. [PubMed] |
| 5. | Knoll H, Ziegeler S, Schreiber JU, Buchinger H, Bialas P, Semyonov K, Graeter T, Mencke T. Airway injuries after one-lung ventilation: a comparison between double-lumen tube and endobronchial blocker: a randomized, prospective, controlled trial. Anesthesiology. 2006;105:471-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 171] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 6. | Nikolovski N, Kopacheva-Barsova G, Pejkovska A. Laryngotracheal Stenosis: A Retrospective Analysis of Their Aetiology, Diagnose and Treatment. Open Access Maced J Med Sci. 2019;7:1649-1656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Seo JH, Kwon TK, Jeon Y, Hong DM, Kim HJ, Bahk JH. Comparison of techniques for double-lumen endobronchial intubation: 90° or 180° rotation during advancement through the glottis. Br J Anaesth. 2013;111:812-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | D'Anza B, Knight J, Greene JS. Does body mass index predict tracheal airway size? Laryngoscope. 2015;125:1093-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Gelbard A, Francis DO, Sandulache VC, Simmons JC, Donovan DT, Ongkasuwan J. Causes and consequences of adult laryngotracheal stenosis. Laryngoscope. 2015;125:1137-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 233] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 10. | Karmali S, Rose P. Tracheal tube size in adults undergoing elective surgery - a narrative review. Anaesthesia. 2020;75:1529-1539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Drosnes DL, Zwillenberg DA. Laryngeal granulomatous polyp after short-term intubation of a child. Ann Otol Rhinol Laryngol. 1990;99:183-186. [PubMed] |
| 12. | Park SY, Choi HS, Yoon JY, Kim EJ, Yoon JU, Kim HY, Ahn JH. Fatal vocal cord granuloma after orthognathic surgery. J Dent Anesth Pain Med. 2018;18:375-378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Ogawa M, Hosokawa K, Iwahashi T, Inohara H. The results of Kaplan-Meier and multivariate analyses of etiological factors related to the outcome of combined pharmacological therapy against laryngeal granuloma. Acta Otolaryngol. 2016;136:1141-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |