Published online Dec 6, 2022. doi: 10.12998/wjcc.v10.i34.12462
Peer-review started: August 27, 2022
First decision: September 5, 2022
Revised: September 17, 2022
Accepted: November 7, 2022
Article in press: November 7, 2022
Published online: December 6, 2022
Processing time: 96 Days and 20.4 Hours
The novel coronavirus disease 2019 (COVID-19) is an ongoing disease caused by severe acute respiratory syndrome coronavirus-2 that still poses an important and urgent threat to global health. In Slovenia, the epidemic was declared on March 12th, 2020, and since then COVID-19 has had a great impact on our health system. The field of neurosurgery in particular has been experiencing difficulties in both elective and emergency service. In this article, we described epidemiologic protocols and the effect that the COVID-19 pandemic had on the surgical practice and workflow of the Department of Neurosurgery at the University Medical Centre Ljubljana. We analyzed and compared the number of elective and emer
Core Tip: The novel coronavirus disease 2019 (COVID-19) is an ongoing disease caused by severe acute respiratory syndrome coronavirus-2 that poses an important and urgent threat to global health and has had a great impact on the health system in Slovenia. In this article, we described epidemiologic protocols and the effect that the COVID-19 pandemic had on the surgical practice and workflow of the Department of Neurosurgery at University Medical Centre Ljubljana.
- Citation: Munda M, Bosnjak R, Velnar T. Problematics of neurosurgical service during the COVID-19 pandemic in Slovenia. World J Clin Cases 2022; 10(34): 12462-12469
- URL: https://www.wjgnet.com/2307-8960/full/v10/i34/12462.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i34.12462
Coronavirus disease 2019 (COVID-19) is a novel coronavirus disease that primarily affects the respiratory system but may also infect multiple organs, including the brain. It was first reported as 4 cases of pneumonia of unknown etiology on December 29, 2019 in Wuhan, Hubei Province, China and is responsible for an ongoing pandemic. The disease presented with unique and severe biological characteristics, specific blood test results, particular clinical symptoms and imaging characteristics[1-3]. The virus genome analysis showed high sequence similarity to a bat coronavirus, which was detected in the Rhinolophus affinis species, therefore framing the hypothesis that the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) originated from bats and was then transmitted to humans through unknown intermediary animals[4]. It was swiftly recognized as a major threat to global health and on March 11, 2020, COVID-19 was declared a pandemic by the World Health Organization. At the time of writing in August 2022, the disease is present in almost every country around the world, and the number of infected patients exceeds 550 million. The real number of infected people is in all likelihood much higher. Furthermore, the number of deaths caused by COVID-19 is predicted to be more than 6.4 million[5].
Slovenia is a central European country and a member of the European Union with a population of approximately two million inhabitants. There are two neurosurgical centers, both organized as departments within the Division of Surgery. They are both located at university hospitals, one in the capital city of Ljubljana and the other in Maribor, which is the second largest city in Slovenia. The Department of Neurosurgery at University Medical Centre Ljubljana consists of 50 beds and an intensive care unit; the department in Maribor is half this size. In accordance with the regional division of Slovenia, the Department of Neurosurgery in Ljubljana covers approximately two-thirds of the population with Maribor covering the rest.
Being a neighboring country of Italy, where the province of Bergamo suffered one of the first major COVID-19 outbreaks in Europe, Slovenia faced a great risk of a very early epidemic onset. It was virtually impossible to adapt and prepare the health system for the impending threat on time. Our first reported case emerged on March 4, 2020, shortly after outbreaks occurred in other central European countries. A few days later, the official epidemiological safety measures at the state level were put into action, and on March 12, 2020, an epidemic was declared[6,7].
In addition to the general epidemic measures that took place at the state level (mandatory masks, state lockdown, strict border crossing rules, etc.) a series of hospital and departmental protocols were put into practice to prevent the virus spreading inside the hospitals and health centers. Some of the measures included adjustments of outpatient services, postponement of elective surgeries, strict regulations upon patient admission, additional departmental and surgical premises for high-risk or COVID-19-positive patients, quantitative reduction of the surgical program, reallocation of staff to COVID-19-related posts, constant use of protective equipment, expansion of telephone consultation service and many more. The purpose of this article was to outline the effect that COVID-19 had on the management of patients at the Department of Neurosurgery in Ljubljana and assess the number of our surgical cases in comparison to pre-COVID-19 times.
Under normal circumstances prior to the COVID-19 epidemic, the Department of Neurosurgery in Ljubljana consisted of 50 patient beds and one intensive care unit that could hold 10 patients. The elective neurosurgical patients were admitted from home or transferred from another department. Emergency cases were admitted directly via the emergency center. Upon admittance, the patients underwent routine clinical evaluation, laboratory results and neuroimaging examinations that were needed for the surgery. The operations took place in two elective operating theatres, and a third operating theatre was reserved for emergency surgeries.
In the early phases of the COVID-19 epidemic, the performance of our health system was in jeopardy, as the established clinical pathways did not meet the needs of the demanding epidemiological situation. The swift outbreak of the epidemic resulted in unpreparedness on the local, state and global levels. The circumstances were constantly changing and with the lack of knowledge about the disease, it was nearly impossible to set up a new, sustainable and stable system with optimal guidelines that would prove useful in the long run. Over time, experience and knowledge accumulated, and more stable protocols were implemented and put into clinical practice. However, they still varied on a monthly or weekly level in accordance with the number of infected people in the population, staff availability and occupancy of COVID-19 hospital beds.
All patients in need of a neurosurgical treatment or assessment were screened and evaluated as a first step. In the emergency setting, they were managed immediately in accordance with the underlying pathology and at the same time tested for COVID-19 infection using a nasopharyngeal swab for the reverse transcription polymerase chain reaction (PCR) test. If the patient needed immediate surgery and no time could be wasted waiting for the result, the patient was treated as a COVID-19-positive until proven otherwise. In the beginning, due to the limited capacities and equipment of the microbiological laboratories, it could take hours or even until the next morning until the test result was available. This meant that all preoperative preparation, imaging and surgical care was carried out with the required protective measures. Therefore, the hospital needed to provide a separate area, special anesthesiological and surgical management, additional teams and extra safety measures, including personal protective equipment and specialized cleaning and ventilation. All these challenges, in the beginning, took great effort and extra time, hence compromising patient care and treatment outcome. In time, the situation gradually started to normalize, and the fast PCR tests and rapid antigenic tests came into everyday clinical routine. They were regularly utilized as a first screening test, thus drastically reducing the time delay until the test result. In non-emergency or elective cases, a standard PCR test was still needed before the admittance or transfer to the department.
With the higher number of COVID-19 cases in the population, the chance of virus invasion and departmental outbreaks increased. Therefore, in the later phase of the epidemic, the hospital safety measures and admittance algorithm had to change, adapt and become stricter. All the neurosurgical patients and premises associated with their treatment were divided into three groups: Red (danger zone), grey (transitional zone) and green (safe zone).
The red zone was a high-risk zone with confirmed COVID-19-positive patients. In practice, this meant that in the event of a COVID-19 outbreak, some rooms at the department became isolation rooms, and entry was allowed only while wearing special personal protective equipment. Departmental outbreaks also resulted in the spread of the virus among medical and other personnel. Altogether, this reduced the possibility of a normal workflow in the department and the operating theatres.
The grey zone included all patients admitted to the department who required non-urgent elective treatment. Upon admission, they were denied any contact with green zone patients or staff and were temporarily stationed in transitional grey zone hospital rooms until a negative reverse transcription PCR SARS-CoV-2 test was confirmed. Personal protective equipment was provided both for patients and for the grey zone staff. After the test results became available, they were transferred to a green zone regular ward. In the event of a positive SARS-CoV-2 test and in the absence of reasons for hospitalization or emergency surgery, they were sent back home, and the procedures were rescheduled in accordance with the patient’s contagion period.
The green zone consisted of all COVID-19 negative patients, who were routinely tested every 3 or more days following admission. The protocols for routine testing were constantly changing in accordance with the latest guidelines. In the event of risky contact with a SARS-CoV-2-positive patient or personnel, the green zone patients were transferred to the transitional zone, where they remained until the quarantine period expired.
After the SARS-CoV-2 vaccine became widely available, the management of the zone system became easier. To be treated as a green zone patient, an individual was required to fulfil one of three conditions: That they be vaccinated; previously recovered from COVID-19; or have a negative PCR test. It was called the RVT rule: R for recovered, V for vaccinated and T for tested. With more and more individuals being vaccinated or recovering from the disease, less pressure was put on transitional zones, and the health system was one step closer to a more fluid workflow.
The performance and the dynamics of the COVID-19 management improved even more in November 2020 when the entire new premises of the hospital were adapted into a COVID-19 treatment center named Diagnostical and Technical Service (DTS), which could hold more than 200 COVID-19-positive patients. It also included the intensive and critical care unit. Compared to earlier COVID-19 departments that were scattered among different buildings and clinics, the capacity of the new premises was relatively large and centralized. All SARS-CoV-2-positive patients, including every neurosurgical patient after emergency surgery, were transferred to DTS, where they continued with their treatment. The core of the DTS medical staff consisted of infectious disease specialists with specialists and residents from other medical fields who were rotated there on a monthly basis. The system was optimized so that in cooperation with the neurosurgical consultant service the patients were treated in a multidisciplinary manner and simultaneously for COVID-19 and their primary underlying pathology. During the times when the number of SARS-CoV-2-positive patients was relatively manageable, this new solution relieved the epidemiological pressure on non-infectious clinical departments and allowed them to function and operate on an almost pre-pandemic level. The main weakness, however, was that these new premises required a large number of new staff that the hospital did not have, so numerous personnel, including doctors and nurses, were relocated from their home departments. Due to the lack of staff, the work in the department and operating theatres was once again limited.
During the winter of 2021/2022, due to a high number of COVID-19-related hospitalizations, even the capacities of DTS were almost completely occupied. Thus, the red zones in the department were reactivated. Only the patients with severe respiratory symptoms or those in need of the intensive care unit were transferred to DTS, while everyone else was treated in the department with the help of an extended infectious disease consultation service. With the introduction of new, less aggressive variants of the virus at the beginning of 2022, the situation gradually improved as fewer and fewer COVID-19 patients developed pneumonia and had a need for oxygen and hospitalization. In May 2022, the DTS was closed down, and the zone system currently remains in use in the department.
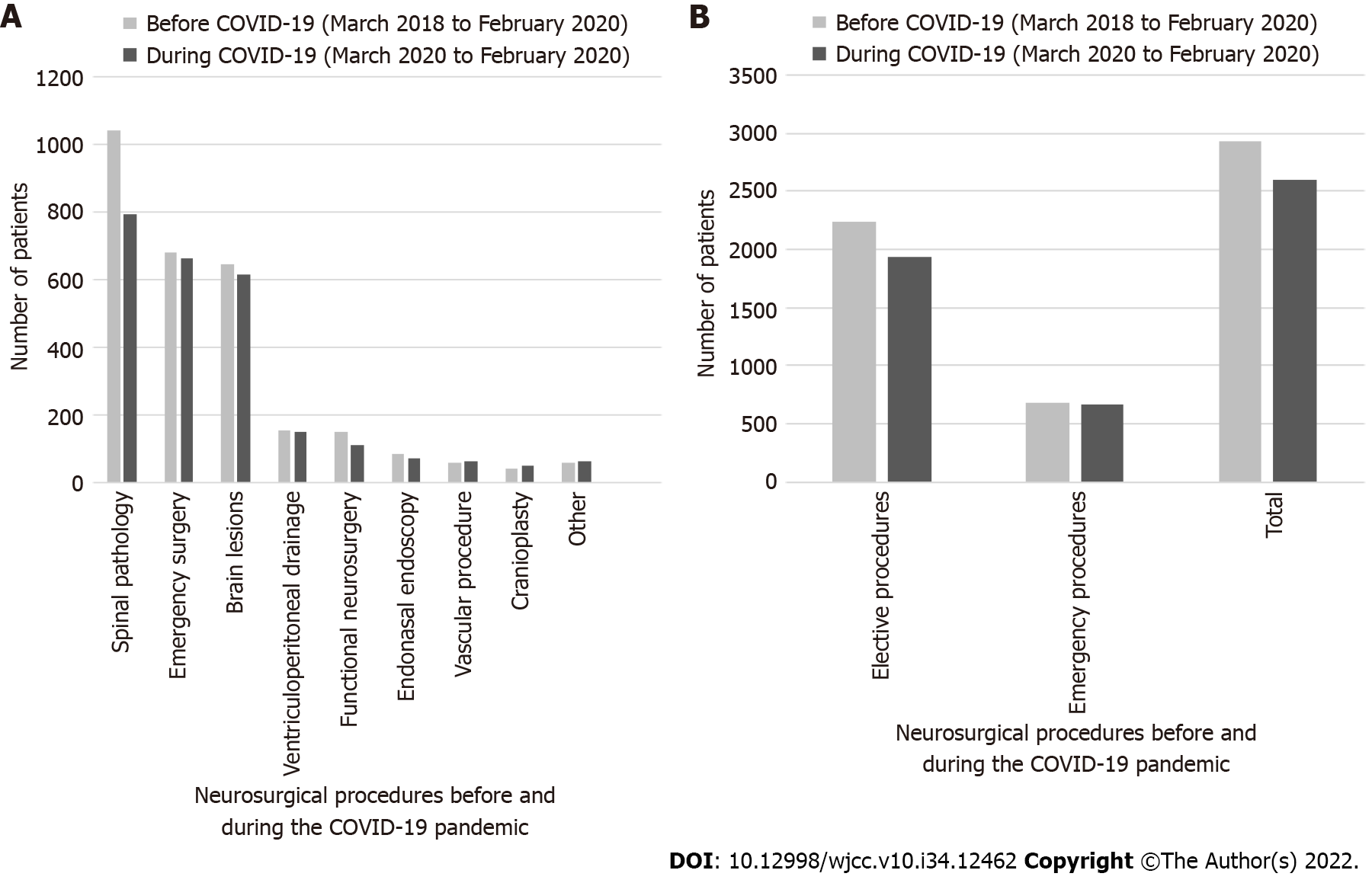
We analyzed and compared the number of elective and emergency surgeries before and during the pandemic (Figure 1). In this article, we address an emergency case as any case that needed immediate surgery in a matter of hours due to a life-threatening situation and an elective case as any case that was scheduled in advance and operated on during working hours. For the analysis, we divided the procedures into subgroups. These were related to underlying pathology as follows: (1) Spinal pathology (spinal degenerative disorders, spinal lesions, etc.); (2) Brain lesions (any supra- or infratentorial brain tumors, cysts, abscesses or similar pathology); (3) Ventriculoperitoneal drainage; (4) Cranioplasty; (5) Functional neurosurgical procedure (deep brain stimulation, spinal cord stimulation, vagus nerve stimulation, replacement of the batteries, etc.); (6) Vascular pathology (aneurysms, arteriovenous malformations, etc.); (7) Endonasal endoscopy (pituitary adenoma, Rathke cyst, clivus chordoma, craniopharyngioma, etc.); and (8) Other. Emergency surgery was any procedure that needed immediate intervention, and it included any form of an acute brain hemorrhage (epidural, subdural or intracerebral), decompressive craniectomy, insertion of external ventricular drainage or intracranial pressure monitoring and evacuation of chronic subdural hematoma.
Two years before the COVID-19 pandemic was declared (from March 2018 to February 2020), a total of 2924 patients were treated surgically at the Department of Neurosurgery in Ljubljana. There were 2413 elective cases. Altogether, 1042 surgeries addressed spinal pathology, 646 brain lesions, 154 elective ventriculoperitoneal drainages for hydrocephalus treatment, 41 cranioplasties, 150 functional, 62 vascular, 86 endonasal endoscopic and 62 other procedures. There were 681 emergency surgeries.
During a 2-year period after the COVID-19 pandemic was declared (from March 2020 to February 2022), a total of 2597 patients were treated surgically. There were 1932 elective procedures. There were 797 spinal pathology surgeries, 665 brain lesions, 153 ventriculoperitoneal drainages, 50 cranioplasties, 113 functional, 65 vascular, 75 endoscopic endonasal and 64 other procedures. There were 665 emergency surgeries (Tables 1 and 2).
| Type of neurosurgical procedure | Number of cases | Decrease in number of cases | |
| March 2018 to February 2020 | March 2020 to February 2022 | ||
| Spinal pathology | 1042 | 797 | 245 (23.5) |
| Emergency surgery | 681 | 665 | 16 (2.4) |
| Brain lesions | 646 | 615 | 31 (4.8) |
| Ventriculoperitoneal drainage | 154 | 153 | 1 (0.7) |
| Functional neurosurgery | 150 | 113 | 37 (24.7) |
| Endonasal endoscopy | 86 | 75 | 11 (12.8) |
| Vascular procedure | 62 | 65 | / |
| Cranioplasty | 41 | 50 | / |
| Other | 62 | 64 | / |
| Total | 2924 | 2597 | 327 (11.2) |
| Type of surgery | Number of cases | Decrease in number of cases | |
| March 2018 to February 2020 | March 2020 to February 2022 | ||
| Elective surgery | 2243 | 1932 | 311 (13.9) |
| Emergency surgery | 681 | 665 | 16 (2.4) |
Overall, we recorded an 11.2% (n = 327) decrease in all neurosurgical procedures in the 2 years during which COVID-19 was declared compared to the 2-year period before. A decrease of 13.9% (n = 311) in elective procedures was observed, mostly on account of spinal pathology procedures (23.5% decrease or 245 cases), functional neurosurgical procedures (24.7% decrease or 37 cases), endonasal endoscopy procedures (12.8% decrease or 11 cases) and brain lesions (4.8% decrease or 31 cases). The decrease in emergency procedures was insignificant and amounted to a 2.4% drop (n = 16).
The COVID-19 pandemic has affected our health system to a great extent and highlighted its well-known weaknesses. Compared to other specialties, neurosurgery suffered for the most part with one of the main reasons being a centralization of the neurosurgical service into two clinical centers with a lack of peripherally distributed services, as seen in other surgical subdivisions[6-8]. With the shortage of staff due to illness or reallocation to a COVID-19-related post, the working capacities of the department were limited, and no compensation through other medical institutions was possible. Due to the COVID-19 pandemic, it became necessary to reorganize and adapt the neurosurgical practice. Adjustments were required in surgical scheduling, patient admission, outpatient clinic management, emergency treatment and general protective measures. Several clinical guidelines have been announced internationally[8-10]. Overall, the hospital protocols were constantly changing, improving and rapidly adapting to the flow of the pandemic[8-11]. When the number of new COVID-19 cases per day decreased and the pressure on the hospital was lessened, there was a larger capacity for elective surgical programs. Once the COVID-19 numbers rose again, the restrictions and limitations were used again. Within these fluid circumstances, it was important to try to maintain a workflow that was as close to normal as possible[11].
We experienced numerous difficulties in both elective and emergency services. In neurosurgery, it is difficult to assess whether pathology is urgent or elective. Life-threatening emergency cases must always be addressed immediately, and even so-called elective pathologies, such as various brain tumors, hydrocephalus, spinal lesions, etc., are urgent and cannot be delayed for a long period. The lesions rapidly progress and cause further irreversible damage to the nervous system and neurological deterioration. The inflow of patients during the pandemic did not change drastically, yet a new variable of COVID-19 infection was introduced, and it altered the neurosurgical management of the patients[10].
We analyzed and compared the number of neurosurgical operations in a 2-year period before and after the COVID-19 pandemic was officially declared in our country. We recorded a relatively small decrease of 13.9% or 311 cases of elective surgery for 2 years after the pandemic started. The decrease in cases was mostly in the fields of spinal pathology and functional neurosurgery as these types of procedures were the least urgent because of the non-malignant nature of the pathology and the low risk of neurological deterioration. Regarding spinal pathology, the reduction was mostly because of degenerative spinal disorders with pain syndromes. Cases with accompanying neurological deficits or spinal lesions were addressed and operated on accordingly and as soon as possible. The number of procedures in other areas of neurosurgical fields was quite comparable. Overall, we did not record any missed cases or cases with irreversible neurological damage due to the pandemic measures and restrictions. There was a small decrease in the number of brain and sellar lesions, which might be coincidental. Another explanation may be that patients without acute clinical presentation did not receive adequate health services and appropriate diagnostics in a sufficient time. during the height of the pandemic. After the diagnosis and indication for neurosurgical treatment were confirmed, the patients were presented to our service by the established and uncompromised clinical pathways.
The decrease in the number of elective surgeries during the pandemic was not as drastic as we predicted it would be. One of the reasons for that was the effective COVID-19 screening protocol. Very few surgeries were cancelled due to a SARS-CoV-2-positive patient because if the patient presented with a positive test, he or she was rescheduled, returned home and a substitute patient was called in for the procedure. Another contributing factor might also be that during the quieter periods of the pandemic when medical staff returned to their original posts, more surgeries were performed to reduce the backlog.
Throughout the world, the COVID-19 pandemic had a significant effect on emergency services and the transportation system. It decreased the number of patients transported by ambulance and redesigned the triage algorithm and emergency protocols[12-14]. In neurosurgery, promptness of transport is of great importance and influences the optimal surgical outcome. Neurosurgical emergency patients who experience a delay of 4 h or more before the surgery have a higher mortality rate compared to those who receive treatment on time. The usual transportation time to the neurosurgical centers in Slovenia varies from 1-4 h, depending on the location of the patient and the primary admission location. It also depends on the type of transport (via road or by helicopter). Therefore, all admitted patients were categorized based on the degree of emergency and screened for SARS-CoV-2.
The inclusion criteria for rapid surgery regardless of SARS-CoV-2 status included: (1) Pediatric and adult patients presenting with symptoms of raised intracranial pressure due to stroke, abscess, tumor, brain edema, hematoma or deteriorating hydrocephalus; (2) Traumatic cases in need of emergency intervention such as acute subdural, epidural or intracerebral hematoma evacuation, decompressive craniectomy, external ventricular drainage; (3) Spinal compressive myelopathies (traumatic or non-traumatic) with neurological deficits or an observable deterioration of symptoms; and (4) Vascular emergencies, such as a ruptured intracranial aneurysm or ruptured arteriovenous malformations.
With other SARS-CoV-2-positive patients, conservative treatment was applied if possible or the patient was rescheduled for surgery following the expiration of the contagious period. With these measures in place, the clinical flow of neurosurgical emergencies was optimized so that the patients were not deprived of immediate neurosurgical intervention. We confirmed this with the number of emergency operations 2 years before and after the COVID-19 pandemic was declared. In comparison, from March 2018 to February 2020, we performed 681 emergency procedures and from March 2020 to February 2022, the number of surgeries was 665. Despite the limitations and epidemiological situation, we did not record a significant quantitative decrease in neurosurgical emergency service. Although COVID-19 was an important factor in the treatment of urgent neurosurgical patients, with the measures in place we did not notice any direct impact on surgical outcome and postoperative virulence. The postoperative course relied on the severity of the cardiorespiratory impairment due to COVID-19 before neurological damage. Patients with mild respiratory symptoms were extubated after the procedure mostly without inconvenience, and those with severe respiratory failure and pulmonary damage were transferred to an intensive care unit where the extubation was postponed until adequate cardiorespiratory stability.
With new triage systems on the level of the outpatient clinic, we minimized and optimized patient admission. With a nonregulated inflow of patients, the risk of the transmission of COVID-19 to other patients and hospital staff is high. In general, SARS-CoV-2-positive patients who undergo surgical intervention have a higher complication and mortality rate in some studies than SARS-CoV-2-negative patients[15,16]. It is also implied that in subclinical SARS-CoV-2 patients, the surgery impairs the immune system and increases the likelihood of the emergence of fully symptomatic COVID-19[15-17].
The COVID-19 pandemic also presented a great impact on hospital and departmental staff. The main causes for the shortage of healthcare personnel were recurring sick leaves, transfer to a COVID-related post and general lockdown, due to which healthcare students and volunteers were unable to participate in hospital work. Younger workers in particular, such as residents, nurses, physiotherapists and administrative and other workers, were transferred for an indefinite period to COVID-19 departments. Depending on the size of the department, the quotas were set, in accordance with which it was necess
COVID-19 is not only associated with a high mortality rate but also puts an enormous strain on the healthcare system[14]. Severe forms of COVID-19 with respiratory failure lead to a high rate of intubation, thus creating a shortage of beds in the intensive care units[15,16]. Therefore, the treatment of other critical diseases becomes even more difficult and limited. From a neurosurgical perspective, the COVID-19 pandemic forced us to keep in mind that regular neurosurgery needed to continue in parallel with the treatment of COVID-19 and that it was necessary to balance these two aspects of our everyday work as ideally as possible.
COVID-19 had a vast impact on our healthcare system. The circumstances and management protocols were constantly changing and adapting to the flow of the pandemic. Nonetheless, we managed to provide almost uninterrupted neurosurgical care in the years following the global outbreak, especially regarding life-saving procedures. In the long run, new and enhanced strategies will be needed for the neurosurgical service and healthcare system in general, to return it to its uncompromised and optimal performance.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Slovenia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Carlan SJ, United States; Leowattana W, Thailand S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ
| 1. | Haidar MA, Shakkour Z, Reslan MA, Al-Haj N, Chamoun P, Habashy K, Kaafarani H, Shahjouei S, Farran SH, Shaito A, Saba ES, Badran B, Sabra M, Kobeissy F, Bizri M. SARS-CoV-2 involvement in central nervous system tissue damage. Neural Regen Res. 2022;17:1228-1239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 2. | Peacock WF, Soto-Ruiz KM, House SL, Cannon CM, Headden G, Tiffany B, Motov S, Merchant-Borna K, Chang AM, Pearson C, Patterson BW, Jones AE, Miller J, Varon J, Bastani A, Clark C, Rafique Z, Kea B, Eppensteiner J, Williams JM, Mahler SA, Driver BE, Hendry P, Quackenbush E, Robinson D, Schrock JW, D'Etienne JP, Hogan CJ, Osborne A, Riviello R, Young S. Utility of COVID-19 antigen testing in the emergency department. J Am Coll Emerg Physicians Open. 2022;3:e12605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Chams N, Chams S, Badran R, Shams A, Araji A, Raad M, Mukhopadhyay S, Stroberg E, Duval EJ, Barton LM, Hajj Hussein I. COVID-19: A Multidisciplinary Review. Front Public Health. 2020;8:383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 171] [Cited by in RCA: 182] [Article Influence: 36.4] [Reference Citation Analysis (0)] |
| 4. | Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15248] [Cited by in RCA: 14090] [Article Influence: 2818.0] [Reference Citation Analysis (1)] |
| 5. | World Health Organization. WHO Coronavirus (COVID-19) Dashboard. [cited 24 August 2022]. Available from: https://covid19.who.int/. |
| 6. | Perico N, Fagiuoli S, Di Marco F, Laghi A, Cosentini R, Rizzi M, Gianatti A, Rambaldi A, Ruggenenti P, La Vecchia C, Bertolini G, Paglia S, Lorini FL, Remuzzi G. Bergamo and Covid-19: How the Dark Can Turn to Light. Front Med (Lausanne). 2021;8:609440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Vlada Republike Slovenije. Slovenija razglasila epidemijo novega koronavirusa. [cited 24 August 2022]. Available from: https://www.gov.si/novice/2020-03-12-slovenija-razglasila-epidemijo-novega-koronavirusa/. |
| 8. | Liu Z, Zhang Y, Wang X, Zhang D, Diao D, Chandramohan K, Booth CM. Recommendations for Surgery During the Novel Coronavirus (COVID-19) Epidemic. Indian J Surg. 2020;82:124-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 9. | Burke JF, Chan AK, Mummaneni V, Chou D, Lobo EP, Berger MS, Theodosopoulos PV, Mummaneni PV. Letter: The Coronavirus Disease 2019 Global Pandemic: A Neurosurgical Treatment Algorithm. Neurosurgery. 2020;87:E50-E56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 10. | American College of Surgeons. COVID-19: Recommendations for Management of Elective Surgical Procedures. [cited 24 August 2022]. Available from: https://www.facs.org/for-medical-professionals/covid-19/clinical-guidance/elective-surgery/. |
| 11. | Olson S, Honeybul S, Rosenfeld JV. Considering Futility of Care Decisions in Neurosurgical Practice. World Neurosurg. 2021;156:120-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Katayama Y, Kiyohara K, Kitamura T, Hayashida S, Shimazu T. Influence of the COVID-19 pandemic on an emergency medical service system: a population-based, descriptive study in Osaka, Japan. Acute Med Surg. 2020;7:e534. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 13. | Gulen M, Satar S, Acehan S, Bozkurt M, Aslanturkiyeli EF, Sevdimbas S, Esen CI, Balcik M, Uzucek MD, Sahin GK, Firat BT. Have the Diagnoses of Patients Transported by Ambulances Changed in the Early Stage of the COVID-19 Pandemic? Prehosp Disaster Med. 2022;37:4-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 14. | Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 577] [Cited by in RCA: 830] [Article Influence: 166.0] [Reference Citation Analysis (0)] |
| 15. | Ozoner B, Gungor A, Hasanov T, Toktas ZO, Kilic T. Neurosurgical Practice During Coronavirus Disease 2019 (COVID-19) Pandemic. World Neurosurg. 2020;140:198-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 16. | Panciani PP, Saraceno G, Zanin L, Renisi G, Signorini L, Fontanella MM. Letter: COVID-19 Infection Affects Surgical Outcome of Chronic Subdural Hematoma. Neurosurgery. 2020;87:E167-E171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | O'Dwyer MJ, Owen HC, Torrance HD. The perioperative immune response. Curr Opin Crit Care. 2015;21:336-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |