Published online Nov 26, 2022. doi: 10.12998/wjcc.v10.i33.12422
Peer-review started: September 5, 2022
First decision: September 26, 2022
Revised: October 5, 2022
Accepted: October 31, 2022
Article in press: October 31, 2022
Published online: November 26, 2022
Processing time: 78 Days and 21.5 Hours
Allergic cutaneous vasculitis (ACV) is a difficult disease to treat. At present, there is no effective treatment for this condition. Traditionally, immunosuppressants and hormones have been primarily used in its management, but the treatment effect is suboptimal, and it has several side effects.
We present the case of a 19-year-old woman who presented at our hospital with a four-year history of symmetric skin lesions mainly affecting her lower extremities. She had previously undergone treatment with prednisolone acetate, cetirizine hydrochloride, and loratadine tablets but had not experienced any relief in her condition. Thereafter, she was treated with oral traditional Chinese medicine. Her skin damage gradually improved within two months of treatment initiation. After six months, the skin ulcers had completely subsided. No evidence of skin ulcer recurrence was observed during the subsequent follow-up. This report presents the first case of a female patient who received oral Danggui Sini decoction for the treatment of ACV.
Danggui Sini decoction may be a promising oral treatment for ACV patients.
Core Tip: This is the first report of the recovery of skin ulcers in a patient with allergic cutaneous vasculitis (ACV) treated with Danggui Sini decoction. This finding indicates that Traditional Chinese Medicine is particularly effective in the treatment of ACV.
- Citation: Chen XY, Wu ZM, Wang R, Cao YH, Tao YL. Danggui Sini decoction treatment of refractory allergic cutaneous vasculitis: A case report. World J Clin Cases 2022; 10(33): 12422-12429
- URL: https://www.wjgnet.com/2307-8960/full/v10/i33/12422.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i33.12422
Allergic cutaneous vasculitis (ACV), also known as cutaneous small vessel vasculitis, allergic small arteritis, or leukocytoclastic vasculitis[1], mainly affects the capillaries, venules and arterioles of the skin. It is a common vasculitis in dermatology and mostly involves children and women in their early adulthood[2]. In a study on cutaneous vasculitis patients in the United Kingdom, Watts et al[3] reported the overall annual incidence of cutaneous vasculitis as 38.6/million, and that of cutaneous leukocytoclastic angiitis as 15.4/million between the years 1990 and 1994[3]. The annual incidence of biopsy-proven leukocytoclastic vasculitis has been reported to be approximately 45 per million individuals[2,4]. Although the exact global prevalence of this pathology is uncertain due to the variability of its definition, it ranges from 2.7 to 29.7 per million people[1-5]. The disease is characterized by pleomorphic skin lesions, such as purpura, maculopapular rash, blood filled blisters, pustules, necrosis, ulcers and nodules in the lower leg and ankle. The aforementioned skin lesions usually manifest in a symmetrical and repetitive pattern, often accompanied by arthritis and myositis, as well as visceral damage in severe cases. The disease follows a prolonged course, spanning months to years, and often leaves pigmentation and scars after the skin lesions subside[2]. It severely damages the skin texture, causing immense psychological and mental stress to the patient as the symptoms worsen. Anticoagulants, hormones, and other drugs that are occasionally used in the clinical treatment of this condition, generally lead to various adverse effects, including increased appetite, weight gain, sleep disturbances, excessive irritability, hypertension, gastrointestinal complications (vomiting, gastritis, and abdominal pain), glycosuria, and infections. Moreover, even after treatment, the disease shows a tendency for recurrence[6]. As such, the therapeutic efficacy of medication for ACV is limited[7]. Traditional Chinese Medicine (TCM) with its focus on overall regulation of the body, can play a multi-target role in modulating the different body systems[8]. TCM is considered a supplementary treatment to achieve a healthy qi and improve immunity in weak individuals. It has been shown to alleviate clinical symptoms and improve cure rates of several diseases[9].
With the increasingly extensive application of TCM in healthcare, it has gained gradual popularity in the treatment of ACV. Moreover, to date, there exists no treatment with proven efficacy for ACV; this has led to the adoption of TCM in its treatment. In this report, we present the case of a patient with ACV, who was successfully treated with a TCM decoction. The Danggui Sini decoction, an aqueous extract of Angelica sinensis, Ramulus Cinnamomi, and Radix Puerariae, has been used vastly in China to treat inflammatory and ischemic diseases[10].
ACV is a very complex vascular disorder. To our knowledge, Danggui Sini decoction is the first effective treatment for this disease, which is why we report this case. We hoped to identify a safer and more effective alternative treatment.
A 19-year-old girl presenting with ACV was treated at Sheng Ai Hospital of TCM on October 18, 2020. Upon history evaluation, the patient conveyed that at 15 years of age she had developed a rash on both lower limbs and ankles that was red, itchy, painless on touch, not raised above the skin surface, and non-patchy. She further reported that since the rashes originally looked like mosquito bites, she did not pay much attention to them.
However, after two weeks, her condition began to worsen, with the rashes turning from the initial red to purpuric, while her lower limbs, ankles, and feet began to swell and fester. She was subsequently hospitalized and was advised to undergo hormone therapy. Considering the patient's youthful age, her family refused the hormonal treatment. Therefore, she was administered intravenous injections of Xuesaitong for half a month, but her condition did not show significant improvement. After discharge from the hospital, in order to speed up recovery, she finally agreed to take oral corticosteroid treatment. Corticosteroid therapy led to symptomatic relief, but it was short lived, and the same condition developed in another part of the ankle after one month.
Over the next two years, she received medical treatment at both the Wuhan First People's Hospital and the Dermatology Hospital Affiliated to the Shandong First Medical University. She was treated with prednisolone acetate, cetirizine hydrochloride, and loratadine tablets. After taking the medications prescribed by both institutions, her symptoms neither dissipated nor aggravated, and the patient exhibited no meaningful improvement.
There is no genetic disease in her family.
No special physical examination of heart, lung and abdomen.
The patient went to the dermatology department of Pu'er People's Hospital, where she underwent routine examinations (complete blood count, urinalysis, erythrocyte sedimentation rate, and immunology examinations). The laboratory urinalysis revealed a red blood cell count of 95.9/mL, red blood cell (high-power field of vision) count of 17.26/HPF, and a positive result for occult blood in the urine.
The patient did not show any imaging examination.
When she visited our hospital for the first time, the patient had the following chief symptoms: Ulceration of both lower limbs and ankles; red, swollen, and painful skin; white exudate and fishy smell of the sores; blood scabs; pale skin of the foot soles and toes, which was cold on touching; and a pale complexion. Her diet and bowel movements were unaltered. Furthermore, the patient’s tongue was light-colored with a thin white coating, and her pulse was deep and thready. According to the symptoms and laboratory test results, the patient was diagnosed with ACV.
On October 18, 2020, we advised the prescription indicated in Table 1 to the patient according to her symptoms, condition of the tongue, and pulse characteristics. The skin lesions are shown in Figure 1A. During the period of treatment at our facility, the patient did not receive any other treatment. Therefore, TCM decoction played the solitary role in clearing heat, promoting dampness and detoxification, warming and invigorating blood vessels, and nourishing Yingyin. After 20 d of treatment (on November 8, 2020), the white exudates on both the lower limbs were significantly reduced, some ulcers had formed scabs, and the pain had also reduced. The condition of the skin ulcers after 20 d of treatment is shown in Figure 1B. At the patient’s second visit, the redness and swelling of the lower extremities and ankles were considerably relieved and residual blood scabs were still present. During the fourth follow-up visit, the patient’s symptoms had almost resolved, the blood scabs had fallen off, the skin color of the feet was pale, and the skin felt lukewarm on touching; the patient’s diet was as usual, her tongue was red, the coating on the tongue was white, and her pulse was thready. The condition of the skin at the fourth visit is shown in Figure 1C. Considering that the disease is caused by compromised blood circulation, cold coagulation of meridians and unfavorable blood circulation, Danggui Sini decoction was used in the present case as it increases the temperature of meridians, disperses cold, and nourishes the blood and dredge meridians. The compatibility is characterized by the combination of warming Yang and dispersing cold, nourishing blood and dredging pulse, warming without dryness, and tonifying without stagnation. The skin condition on April 14, 2021, is shown in Figure 1D. The complete process of change in the skin condition with treatment progression is shown in Figure 1.
| Medication | Phase 1 (October 18, 2020) | Phase 2 (November 8, 2020) | Phase 3 (December 6, 2020) | Phase 4 (March 3, 2021) |
| Honeysuckle | 15 g | 15 g | — | — |
| Oldenlandia | 20 g | 20 g | 20 g | — |
| Dandelion | 20 g | 20 g | 20 g | — |
| Paris polyphylla | 20 g | 20 g | 20 g | — |
| Rehmannia glutinosa | 15 g | — | — | — |
| Cyathulae Radix | 15 g | 15 g | 15 g | 10 g |
| Cassia Twig | 15 g | 15 g | 15 g | 30 g |
| Glycyrrhiza uralensis Fisch | 6 g | 6 g | 6 g | 6 g |
| Pulsatilla chinensis | 30 g | — | — | — |
| Phellodendron amurense Rupr | 15 g | 15 g | — | — |
| Atractylodes lancea | 15 g | — | — | — |
| Talcum | 15 g | 15 g | 15 g | — |
| Tetrapanax papyrifer | — | 10 g | 10 g | 10 g |
| Arnebiae Radix | — | 30 g | 30 g | — |
| Sophora flavescens Alt | — | 10 g | — | — |
| Sanguisorba officinalis L | — | 15 g | — | — |
| Aconitum carmichaeli Debx | — | 15 g | 15 g | 15 g |
| Thlaspi arvense Linn | — | — | 15 g | — |
| Leonurus artemisia | — | — | 15 g | — |
| Tribulus terrestris Linnaeus | — | — | 15 g | — |
| Angelicae sinensis Radix | — | — | 15 g | 15 g |
| Asarum sieboldii Miq | — | — | — | 6 g |
| Paeonia lactiflora Pall | — | — | — | 15 g |
| Zingiber officinale Rosc | — | — | — | 15 g |
| Codonopsis pilosula | — | — | — | 30 g |
| Poria | — | — | — | 15 g |
| Atractylodes macrocephala Koidz | — | — | — | 15 g |
From the initiation to completion of TCM treatment, we adjusted the prescription three times, according to the patient's symptoms, tongue coating, pulse, and other physical examination results. The specific formula administered to the patient is described in Table 1.
The decoction method of TCM followed in the present case was as follows: (1) Soak all medicinal materials in 500 mL cold water for half an hour, boil for half an hour and then turn to low heat and take 400 mL of the resulting juice; (2) Add 500 mL of hot water for the second time, decoct for half an hour, and take 400 mL of the resulting juice; (3) Repeat a second time to achieve the final decoction; (4) 200 mL of this preparation was to be taken orally, three times a day, one dose over two days; and (5) Note that Aconitum carmichaeli Debx contains aconitine, so it should be boiled in water for 3 h, prior to the addition of the other drugs for the combined decoction.
After the completion of TCM treatment, the patient was followed-up twice, on April 14, 2021, and October 8, 2021. At the first follow-up, her symptoms had disappeared. The skin temperature of the hands and feet was normal, skin ulcers of both lower limbs had healed, pain had disappeared, no redness and swelling were observed, and only the scars of the blood scabs had persisted. The second follow-up on October 8, 2021, mainly focused on ruling out disease recurrence, skin rash regression, skin ulceration and to note the skin temperature of the hands and feet post-TCM treatment. There was no relapse or worsening of the patient’s condition after treatment withdrawal, nor did she report any additional symptoms of discomfort.
Herein, we have described the case of a 19-year-old woman with refractory ACV, who experienced an improvement in skin ulcers and complete remission of ACV after six months of treatment using TCM. There is a variety of causes of ACV. From the perspective of western medicine, the pathogenesis of ACV remains unclear. Certain bacteria, viruses, drugs, or chemicals can increase the sensitization of the body, leading to the production of antibodies against these stimulants and ultimately the emergence of allergic reactions. Subsequently, the allergic reaction induces formation of immune complex deposits in the skin capillaries and small vascular endothelium, resulting in the skin lesions of ACV[11]. The treatment choice depends on the severity of the patient's condition and can range from antihistamines to corticosteroids to immunosuppressive drugs[12,13]. However, glucocorticoids are conventionally the first choice of drugs used in clinical practice.
In TCM, the term “blood stasis” is used to describe ACV, which falls within the categories of diseases and syndromes in TCM, such as "melon and rattan entanglement," "plum core fire Dan," and "dampness flow." Such diseases are mostly caused by internal heat in the viscera, cold and dampness invading from the outside, heat, combined cold and humidity, obstruction of veins or stagnation of muscles and veins, loss of nourishment of pulse, failure of yang, and stagnation of qi and blood. In the syndrome differentiation of TCM, the development of ACV has been divided into three stages, namely the acute stage, delayed stage and stable stage.
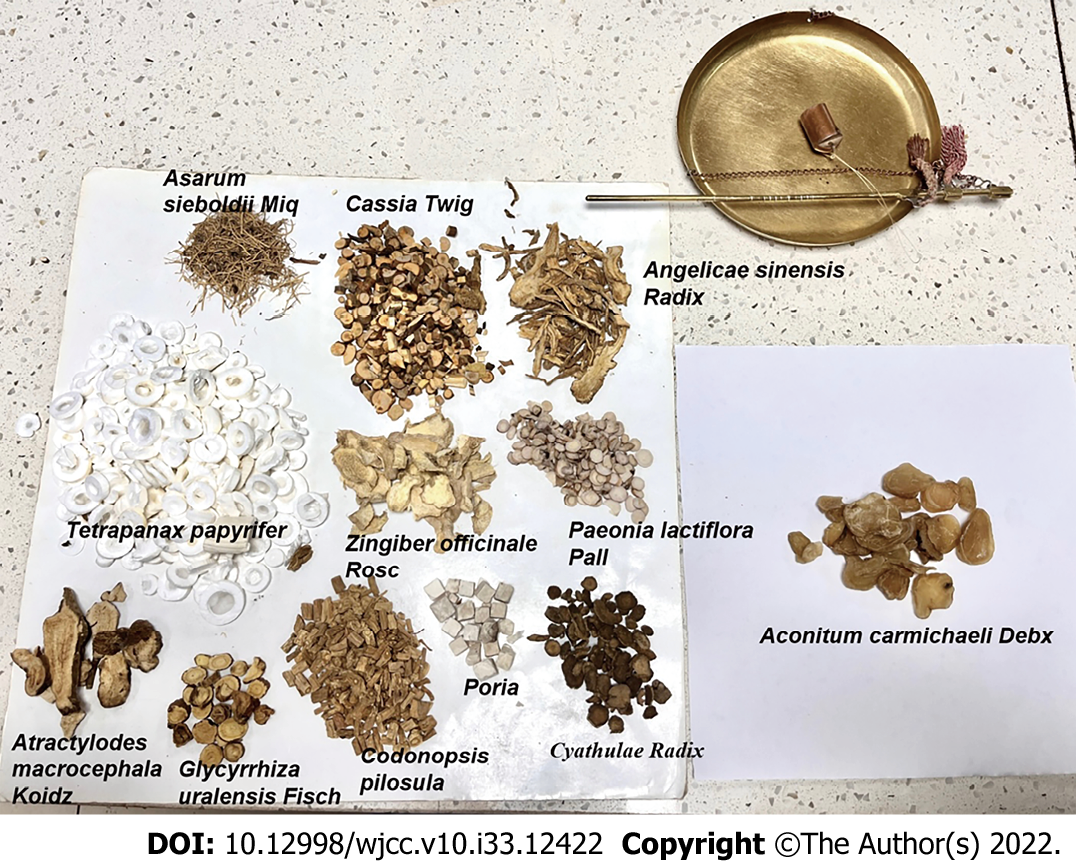
As described in this case, the patient's purpura, skin lesions, and ulcers improved dramatically after oral administration of TCM decoction for six months. In this case, based on the patient’s symptoms and signs at the initial presentation, Professor Zhi-Ming Wu primarily focused on clearing heat, promoting dampness and detoxification, warming blood circulation, and nourishing Yingyin. He used drugs such as honeysuckle, dandelion, Chong Lou, Atractylodes, talc, Phellodendron Phellodendri, and others for clearing heat and detoxification while Achyranthes bidentata was utilized to strengthen the effect of the aforementioned drugs in promoting blood circulation and dredging collaterals. At the second visit of the patient on November 8, 2020, considering that November 7, 2020, is "The Beginning of Winter" in the 24 solar terms, Fuzi was added to the TCM regimen after this visit. Aconite acts by dispelling cold and dehumidification, as well as warming and relieving pain and when coupled with cassia twig, this effect becomes more significant. Additionally, "the Beginning of Winter" makes it necessary to maintain Yang during this period and the heat of aconite can help improve treatment of diseases and enhancement of physique. The diterpene alkaloids contained in aconite have obvious cardiotonic, analgesic, anti-inflammatory, and other effects[14]. Even after the localized symptoms of our patient had improved, the hands and feet were still cold and pale, so adjustment was made to the Danggui Sini decoction accordingly, as the patient showed symptoms of blood deficiency and pulse obstruction, which made the meridians cold. The limbs of the patient had lost Yang temperature and were cold (The medicinal materials in the Danggui Sini Decoction are shown in Figure 2). Danggui Sini decoction can regulate pulse, benefit qi and blood, regulate the sum of operation and defense, and have a significant effect on vascular diseases. Recently, studies have shown that some major compounds in Danggui Sini formula have anti-inflammatory and antioxidant effects, thus inhibiting apoptosis and senescence. Quercetin and kaempferol are common ingredients in licorice[15], and Lu et al[16] reported that quercetin could inhibit the expression and release of various inflammatory factors, such as tumor necrosis factor-α, interleukin (IL)-1β, and IL-6, by suppressing the activation of the nuclear factor kappa light chain enhancer of activated B cells pathway[16]. Furthermore, beta-sitosterol, which is the common component in Angelicae sinensis Radix, Cinnamomi, Ramulus, Paeoniae Radix Alba, and Fructus jujubae, has anti-inflammatory and antioxidant effects[17].
To our knowledge, the present case is the first report of recovery of skin ulcers in a patient with ACV treated with Danggui Sini decoction. It is evident from this case that TCM is particularly effective in the treatment of ACV. No existing reports document the use of this prescription to treat ACV. Thus, the present case provides a reference for the treatment of ACV using TCM. A limitation of our case report is that during treatment, the patient refused to undergo pathological examination, so the relevant pathological examination report was not available to us to explain the disease. The treatment regimen was also tested on only one patient in this case, so the conclusion is not representative. Moreover, the follow-up period was short. We will strive to include more cases and run randomized controlled trials as well as other research projects in the future to confirm the feasibility of this treatment plan and provide new treatment ideas for reducing pain and improving the quality of life of ACV patients. Furthermore, this is a case report outlining the treatment of ACV with Danggui Sini decoction, and we did not determine the molecular mechanism of action of TCM decoction in the treatment of ACV. We hope to draw a clear conclusion in this regard through further relevant studies.
This case suggests that Danggui Sini decoction may be considered an effective therapy for ACV, especially in individuals who are unwilling to receive injections or are unresponsive to hormones and other drugs. However, it is necessary to conduct clinical research studies with larger sample sizes to confirm the efficacy of the proposed prescription. We look forward to treating more ACV cases successfully with Danggui Sini decoction to support our conclusions and lay a foundation for subsequent clinical trials in this area.
Throughout the writing of this dissertation, I have received a great deal of support and assistance. I would first like to thank my supervisor, Professor Zhi-Ming Wu, whose expertise was invaluable in formulating the research questions and methodology. I would particularly like to acknowledge my team members, Rui Wang, Yu-Hong Cao, and Yong-Lian Tao for their wonderful collaboration and patient support. Finally, I could not have completed this dissertation without the support of my friends.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oley MH, Indonesia; Primadhi RA, Indonesia; Tajiri K, Japan S-Editor: Wei ZH L-Editor: A P-Editor: Wei ZH
| 1. | Fraticelli P, Benfaremo D, Gabrielli A. Diagnosis and management of leukocytoclastic vasculitis. Intern Emerg Med. 2021;16:831-841. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 80] [Article Influence: 20.0] [Reference Citation Analysis (1)] |
| 2. | Baigrie D, Goyal A, Crane JS. Leukocytoclastic Vasculitis. 2022 May 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. [PubMed] |
| 3. | Watts RA, Jolliffe VA, Grattan CE, Elliott J, Lockwood M, Scott DG. Cutaneous vasculitis in a defined population--clinical and epidemiological associations. J Rheumatol. 1998;25:920-924. [PubMed] |
| 4. | Arora A, Wetter DA, Gonzalez-Santiago TM, Davis MD, Lohse CM. Incidence of leukocytoclastic vasculitis, 1996 to 2010: a population-based study in Olmsted County, Minnesota. Mayo Clin Proc. 2014;89:1515-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | García-Porrúa C, González-Gay MA. Comparative clinical and epidemiological study of hypersensitivity vasculitis vs Henoch-Schönlein purpura in adults. Semin Arthritis Rheum. 1999;28:404-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 77] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Kapoor D, Sharma S, Garg D, Samaddar S, Panda I, Patra B, Mukherjee SB, Pemde HK. Intravenous Methylprednisolone Versus Oral Prednisolone for West Syndrome: A Randomized Open-Label Trial. Indian J Pediatr. 2021;88:778-784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Zhu KJ, Yang PD, Xu Q. Tofacitinib Treatment of Refractory Cutaneous Leukocytoclastic Vasculitis: A Case Report. Front Immunol. 2021;12:695768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Zhao Z, Li Y, Zhou L, Zhou X, Xie B, Zhang W, Sun J. Prevention and treatment of COVID-19 using Traditional Chinese Medicine: A review. Phytomedicine. 2021;85:153308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 178] [Cited by in RCA: 148] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 9. | Guo X, Zhou D, Sun L, Wang P, Qu J, Zhang C, Wang Y, Chen Z, Li B, Hu J, Lin Z, Shi F, Bai Y, Li Y, Duan X, Bao S, Lan H, Sun X, Wang X, Liu X, Li L, Zhang L, Feng F, Meng Y, Liu Q, Guo X, Guo J, Liu Y, Qi C, Chen J, Feng S, Li P. Traditional Chinese medicine for psoriasis vulgaris: A Protocol of a prospective, multicenter cohort study. Medicine (Baltimore). 2020;99:e21913. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Liu M, Qiang QH, Ling Q, Yu CX, Li X, Liu S, Yang S. Effects of Danggui Sini decoction on neuropathic pain: experimental studies and clinical pharmacological significance of inhibiting glial activation and proinflammatory cytokines in the spinal cord . Int J Clin Pharmacol Ther. 2017;55:453-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Ronkainen J, Koskimies O, Ala-Houhala M, Antikainen M, Merenmies J, Rajantie J, Ormälä T, Turtinen J, Nuutinen M. Early prednisone therapy in Henoch-Schönlein purpura: a randomized, double-blind, placebo-controlled trial. J Pediatr. 2006;149:241-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 184] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 12. | Koutkia P, Mylonakis E, Rounds S, Erickson A. Leucocytoclastic vasculitis: an update for the clinician. Scand J Rheumatol. 2001;30:315-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Runowska M, Majewski D, Puszczewicz M. Life-threatening manifestation of cutaneous leukocytoclastic vasculitis. Postepy Dermatol Alergol. 2021;38:335-337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Zhou G, Tang L, Zhou X, Wang T, Kou Z, Wang Z. A review on phytochemistry and pharmacological activities of the processed lateral root of Aconitum carmichaelii Debeaux. J Ethnopharmacol. 2015;160:173-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 227] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 15. | Wang L, Lin J, Li W. Pharmacological Mechanism of Danggui-Sini Formula for Intervertebral Disc Degeneration: A Network Pharmacology Study. Biomed Res Int. 2021;2021:5165075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Lu J, Wu DM, Zheng YL, Hu B, Zhang ZF, Shan Q, Zheng ZH, Liu CM, Wang YJ. Quercetin activates AMP-activated protein kinase by reducing PP2C expression protecting old mouse brain against high cholesterol-induced neurotoxicity. J Pathol. 2010;222:199-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 150] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 17. | Zhang F, Liu Z, He X, Li Z, Shi B, Cai F. β-Sitosterol-loaded solid lipid nanoparticles ameliorate complete Freund's adjuvant-induced arthritis in rats: involvement of NF-кB and HO-1/Nrf-2 pathway. Drug Deliv. 2020;27:1329-1341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 57] [Article Influence: 14.3] [Reference Citation Analysis (0)] |