Published online Nov 26, 2022. doi: 10.12998/wjcc.v10.i33.12404
Peer-review started: August 31, 2022
First decision: September 26, 2022
Revised: September 30, 2022
Accepted: October 24, 2022
Article in press: October 24, 2022
Published online: November 26, 2022
Processing time: 82 Days and 5 Hours
There are a few cases of lateral lymph node (LLN) metastasis (LLNM) of T1 rectal cancer. Moreover, LLNM is easily missed, especially in patients with early-stage rectal cancer. To our knowledge, the possibility of bilateral LLNM before surgery has not been reported in previous studies.
A 36-year-old woman underwent endoscopic submucosal dissection at a local hospital owing to a clinical diagnosis of a rectal polyp. The pathology report showed a diagnosis of T1 rectal mucinous adenocarcinoma. She was considered to have bilateral LLNM after the examination at our hospital. Laparoscopic total mesorectal excision plus bilateral LLN dissection was performed and the pathological outcomes indicated unilateral LLNM. The patient received long-course adjuvant chemoradiotherapy with no recurrence or metastasis observed during the 1-year follow-up period.
T1 rectal cancer could lead to LLNM and possibly, bilateral LLNM. Therefore, adequate clinical evaluation is essential for these patients.
Core Tip: T1 rectal cancer is rarely accompanied by lymph node metastases, and even fewer lateral lymph node (LLN) metastases (LLNM). To our knowledge, the published case reports to date have mainly reported cases of heterochronous LLNM, only two cases with simultaneous metastases, and only one case of missed LLNM after endoscopic submucosal dissection (ESD). For patients with no residual tumor after ESD, in whom LLNM is suspected, it is also inconclusive whether only LLN dissection could be performed.
- Citation: Liu XW, Zhou B, Wu XY, Yu WB, Zhu RF. T1 rectal mucinous adenocarcinoma with bilateral enlarged lateral lymph nodes and unilateral metastasis: A case report. World J Clin Cases 2022; 10(33): 12404-12409
- URL: https://www.wjgnet.com/2307-8960/full/v10/i33/12404.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i33.12404
The probability of lateral lymph node (LLN) metastasis (LLNM) in locally advanced rectal cancer is 10%-25%[1-3], whereas the corresponding probability of bilateral LLNM is only 2.8%-3.5%[1]. It has been reported that the rate of pelvic extra-regional LNM of T1 rectal cancer is 5.4%[4]. Previous studies have reported that the incidence of LLNM in patients with T1 rectal cancer ranges from 0.5% to 0.9%[5]. However, there have been limited studies in this field, therefore, and more studies are needed. Among the five case reports published to date[6-10], three had focused on heterochronous metastasis and two had reported on simultaneous metastasis. Moreover, four cases had unilateral solitary LLNM (only one LLN had cancer metastasis), and one case had unilateral multiple LLNM (several LLNs at one side had cancer metastasis). In one patient, LLNM was suspected to have been missed before total mesorectal excision (TME) and was found 6 mo postoperatively. In another patient, LLNM was missed before endoscopic submucosal dissection (ESD). The detailed information of the five cases is presented in Table 1. To our knowledge, we report the second case, in which LLNM was missed before ESD, and the first case, where bilateral LLNM was suspected.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | |
| Ref. | Hara et al[6], 2008 | Sueda et al[7], 2013 | Ogawa et al[8], 2016 | Tanishima et al[9], 2017 | Zhang et al[10], 2020 | Ours, 2022 |
| Sex | Male | Female | Female | Male | Male | Female |
| Age (yr) | 61 | 41 | 35 | 56 | 45 | 36 |
| Risk factors of LNM | ||||||
| Depth of invasion (μm) | - | - | 3000 | Head invasion | - | - |
| Histological type | Well | Moderately | Moderately | Moderately | Well | Moderately |
| Budding | - | - | - | 1 | - | - |
| Time after 1st surgery (mo) | 22 | 6 | Simultaneous | 6 | Simultaneous | Simultaneous |
| Treatment | Extended, LLND | Extended, LLND | TME + LLND | LLND | TME + LLND | TME + LLND |
| Bilateral or unilateral LLND | Unilateral | Unilateral | Unilateral | Unilateral | Unilateral | Bilateral |
| Isolated or multiple LLNM | Isolated | Isolated | Isolated | Multiple | Isolated | Multiple |
| Adjuvant therapy after LLND | None | None | Tegafururacil + leucovorin | FOLFOX | XELOX + radiotherapy | XELOX + radiotherapy |
| Follow-up period (mo) | 44 | 12 | 48 | 30 | 10 | 12 |
| Prognosis | Alive | Alive | Alive | Alive | Alive | Alive |
A 36-year-old woman underwent a routine physical examination at a local hospital.
Colonoscopy revealed a polypoid lesion with a diameter of 1.5 cm, and the lower edge was located 3 cm from the anal verge. Because the lesion was more likely to be a polyp, ESD was performed at that time. Pathology revealed a mucinous adenocarcinoma, with moderate differentiation and submucosal invasion. There was no residual tumor at the basal edge or in the resection mucosa. The patient visited our hospital immediately for consultation on whether further treatment was needed.
The woman was previously in good health.
The patient’s family history was unremarkable.
Physical examination revealed no abnormalities except several metal clips that could be palpated on digital rectal examination.
We evaluated the carcinoembryonic antigen and carbohydrate antigen-199 levels, which were found to be 2.54 ng/mL and 12.73 ku/L, respectively. Our pathologists also confirmed the pathologic finding of the local hospital.
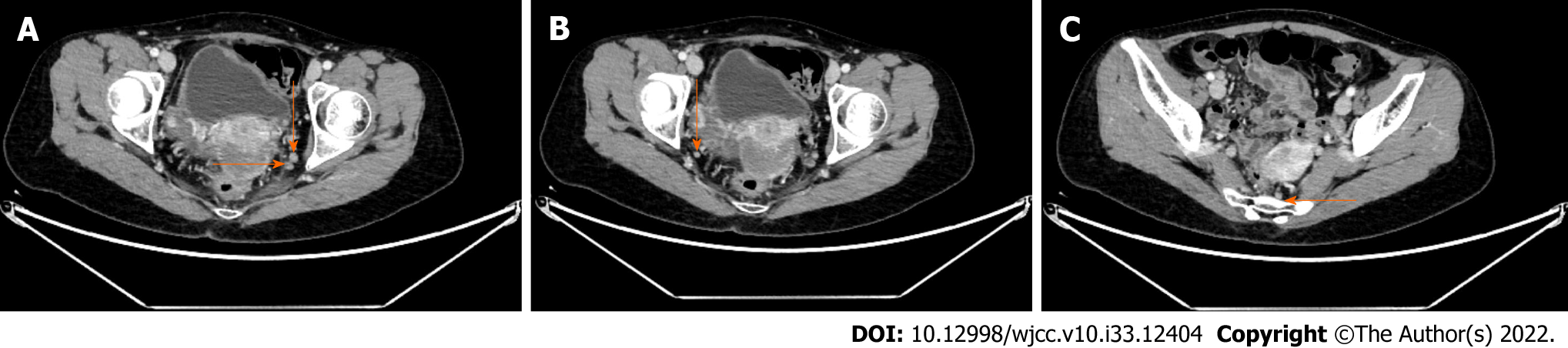
We performed abdominal contrast-enhanced computed tomography (CT) and chest CT for this patient, in addition to a pathological consultation. Magnetic resonance imaging of the pelvis was not performed because there was no residual tumor. The chest CT scan revealed no sign of distant metastasis. However, the abdominal contrast-enhanced CT showed suspected enlarged bilateral LLNs and some enlarged mesorectal LNs (MLN) (Figure 1). Among these, there were two enlarged LLNs in the left lateral area, both located in the distal internal iliac region (263D)[11], with short-axis diameters of 7.1 mm and 6.2 mm, respectively. An enlarged LLN was noted in the right lateral area (distal internal iliac region), with a short-axis diameter of 5.3 mm. These three LLNs had at least two of three malignant features, including a round, irregular border and shape, and heterogeneous density, consistent with a positive LN diagnosis[12]. The maximum short-axis diameter of the enlarged MLN was 4.8 mm, which was insufficient for a diagnosis of LNM.
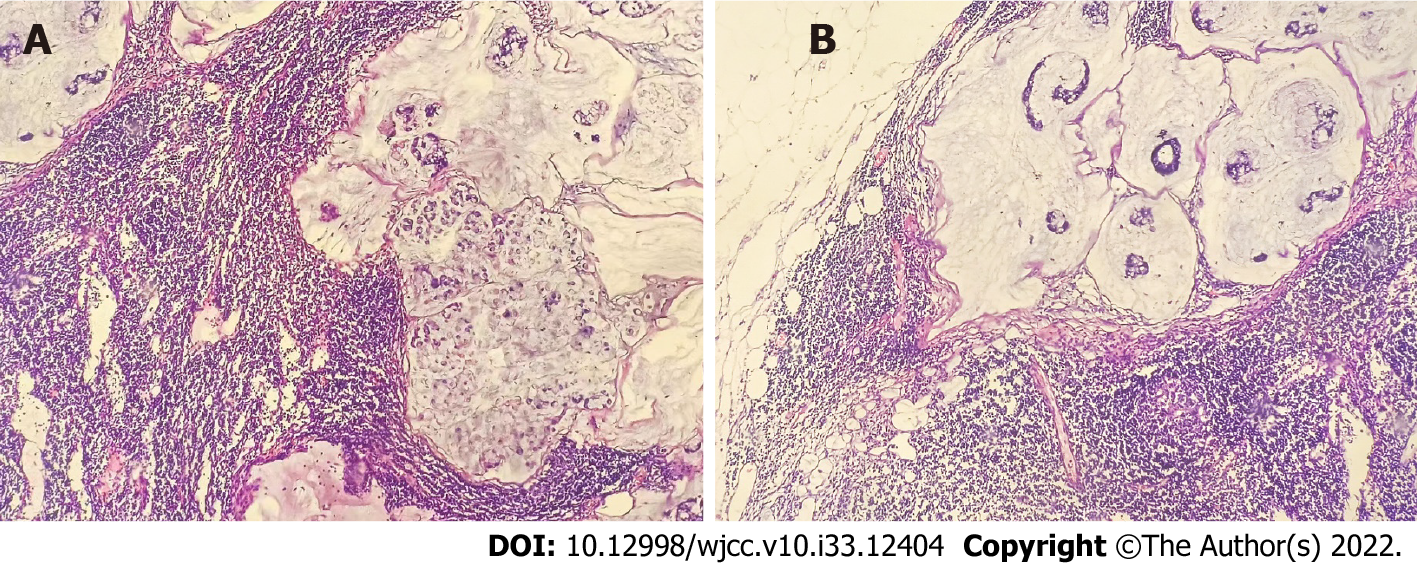
After discussions with the multidisciplinary team and after obtaining the consent of the patient and her family, laparoscopic TME with bilateral lateral lymph node dissection (LLND) was performed. The patient recovered uneventfully and was hospitalized for 10 d with no complications. There was no residual tumor in the rectal specimen and the distal and proximal margins were both negative; only partial mucosal hemorrhage with scattered acute and chronic inflammatory cell infiltration was noted. A total of 31 LNs were harvested, including nine MLNs, 13 left LLNs, and nine right LLNs. The MLNs and right LLNs were confirmed to have no metastasis, but the two enlarged left LLNs were confirmed to have metastasis (Figure 2).
T1 rectal mucinous adenocarcinoma with simultaneous LLNM.
The patient received chemotherapy involving six cycles of XELOX (oxaliplatin plus capecitabine) and radiotherapy (50.4 Gy; 28 fractions).
There was no sign of recurrence or metastasis, and the patient’s urinary and sexual functions were normal during the 1-year follow-up.
A meta-analysis suggested that there is only a 1.9% risk of LNM in T1 rectal cancers with low-risk criteria[13], which was defined as submucosal invasion of ≤ 1000 µm without poor differentiation, lymphovascular invasion, or budding[14]. Thus, the probability of LLNM is even lower in this type of cancer. Most patients with T1 rectal cancer with a diameter of ≤ 2 mm can be cured with ESD[15]. However, the main problem is that it is often difficult to assess the low-risk criteria prior to ESD[16]. Moreover, LLNM is easily missed, especially in patients with early-stage rectal cancer[9].
In our case, the patient achieved the standard clinical cure because she had no risk factors. If the patient did not take the initiative to come to our hospital for a consultation, the LLNM would most likely have been missed. Moreover, she was even suspected to have bilateral LLNM, although it was finally confirmed that she had only unilateral LLNM. Patients with T1 rectal cancer are at the risk of LLNM and may even have bilateral LLNM. ESD may guarantee a clinical cure for the majority of patients with T1 rectal cancer. However, a few patients may need more in-depth clinical examinations to ensure that there is no missed diagnosis, not only for LLNM, but also for liver or lung metastasis[17,18]. Therefore, we suggest that if the relevant examinations cannot be completed before ESD for evaluating the patient’s condition, these examinations should be completed after ESD and according to the standard management for advanced rectal cancer, even if the patients are pathologically diagnosed with T1 stage and have no risk factors. Such an approach would avoid the possibility of missing LLNM or distant metastases.
At present, for advanced rectal cancer with suspected LLNM, although the National Comprehensive Cancer Network guidelines recommend neoadjuvant chemoradiotherapy (nCRT) combined with TME[19], and Japanese guidelines recommend preventive LLND combined with TME[11], neither method can effectively control the lateral local recurrence[20]. Therefore, more and more scholars recommend nCRT combined with TME and selective LLND with the in-depth clinical research[21]. However, there is no guideline or consensus for the treatment of T1 rectal cancer with suspected LLNM. Moreover, the prognosis of advanced rectal cancer with LLNM is significantly worse than that without LLNM, therefore, LLND is necessary[22]. However, no prognostic data have been reported in T1 rectal cancer with LLNM because not enough cases have been reported. Furthermore, we believe that LLND is important in T1 rectal cancer with suspected LLNM according to the prognostic data of advanced rectal cancer.
In addition, in view of the report of Zhang et al[10] and the present study, although simultaneous LLNM was considered after ESD, no residual tumor or mesorectal LNM was observed after TME and LLND. Therefore, LLND may only be possible in such patients (without considering residual tumor and mesorectal LNM) after adequate assessment of the patient’s status. Instead, the “watch and wait” strategy can be implemented for the primary tumor and MLN. However, we have no clinical practice experience regarding this, and our theory needs to be confirmed by more cases or multicenter studies.
T1 rectal cancer could lead to LLNM and possibly, bilateral LLNM. Therefore, adequate clinical evaluation is essential in patients with this type of cancer.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Obando A, Nicaragua; Yap RVC, Philippines S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Kim DJ, Chung JJ, Yu JS, Cho ES, Kim JH. Evaluation of lateral pelvic nodes in patients with advanced rectal cancer. AJR Am J Roentgenol. 2014;202:1245-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Laparoscopic Surgery Committee of the Endoscopist Branch in the Chinese Medical Doctor Association (CMDA); Laparoscopic Surgery Committee of Colorectal Cancer Committee of Chinese Medical Doctor Association (CMDA); Colorectal Surgery Group of the Surgery Branch in the Chinese Medical Association (CMA). [Chinese expert consensus on the diagnosis and treatment for lateral lymph node metastasis of rectal cancer (2019 edition)]. Zhonghua Wei Chang Wai Ke Za Zhi. 2019;22:901-912. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Moriya Y. Treatment of lateral pelvic nodes metastases from rectal cancer: the future prospective. G Chir. 2013;34:245-248. [PubMed] |
| 4. | Kobayashi H, Mochizuki H, Kato T, Mori T, Kameoka S, Shirouzu K, Sugihara K. Outcomes of surgery alone for lower rectal cancer with and without pelvic sidewall dissection. Dis Colon Rectum. 2009;52:567-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 132] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 5. | Sugihara K, Kobayashi H, Kato T, Mori T, Mochizuki H, Kameoka S, Shirouzu K, Muto T. Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum. 2006;49:1663-1672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 338] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 6. | Hara J, Yamamoto S, Fujita S, Akasu T, Moriya Y. A case of lateral pelvic lymph node recurrence after TME for submucosal rectal carcinoma successfully treated by lymph node dissection with en bloc resection of the internal iliac vessels. Jpn J Clin Oncol. 2008;38:305-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Sueda T, Noura S, Ohue M, Shingai T, Imada S, Fujiwara Y, Ohigashi H, Yano M, Tomita Y, Ishikawa O. Case of isolated lateral lymph node recurrence occurring after TME for T1 lower rectal cancer treated with lateral lymph node dissection: report of a case. Surg Today. 2013;43:809-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Ogawa S, Itabashi M, Hirosawa T, Hashimoto T, Bamba Y, Okamoto T. Diagnosis of lateral pelvic lymph node metastasis of T1 lower rectal cancer using diffusion-weighted magnetic resonance imaging: A case report with lateral pelvic lymph node dissection of lower rectal cancer. Mol Clin Oncol. 2016;4:817-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Tanishima H, Kimura M, Tominaga T, Iwakura S, Hoshida Y, Horiuchi T. Lateral lymph node metastasis in a patient with T1 upper rectal cancer treated by lateral lymph node dissection: a case report and brief literature review. Surg Case Rep. 2017;3:93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Zhang X, He D, Ding Y, Liu S, Wang Z. Lateral lymph node dissection after endoscopic submucosal dissection for T1 rectal cancer: a case report. ANZ J Surg. 2020;90:2369-2370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kinugasa Y, Murofushi K, Nakajima TE, Oka S, Tanaka T, Taniguchi H, Tsuji A, Uehara K, Ueno H, Yamanaka T, Yamazaki K, Yoshida M, Yoshino T, Itabashi M, Sakamaki K, Sano K, Shimada Y, Tanaka S, Uetake H, Yamaguchi S, Yamaguchi N, Kobayashi H, Matsuda K, Kotake K, Sugihara K; Japanese Society for Cancer of the Colon and Rectum. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1024] [Cited by in RCA: 1312] [Article Influence: 262.4] [Reference Citation Analysis (1)] |
| 12. | Beets-Tan RGH, Lambregts DMJ, Maas M, Bipat S, Barbaro B, Curvo-Semedo L, Fenlon HM, Gollub MJ, Gourtsoyianni S, Halligan S, Hoeffel C, Kim SH, Laghi A, Maier A, Rafaelsen SR, Stoker J, Taylor SA, Torkzad MR, Blomqvist L. Magnetic resonance imaging for clinical management of rectal cancer: Updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol. 2018;28:1465-1475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 331] [Cited by in RCA: 606] [Article Influence: 75.8] [Reference Citation Analysis (0)] |
| 13. | Mou S, Soetikno R, Shimoda T, Rouse R, Kaltenbach T. Pathologic predictive factors for lymph node metastasis in submucosal invasive (T1) colorectal cancer: a systematic review and meta-analysis. Surg Endosc. 2013;27:2692-2703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 14. | Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 817] [Cited by in RCA: 929] [Article Influence: 92.9] [Reference Citation Analysis (0)] |
| 15. | Tanaka S, Toyonaga T, Morita Y, Hoshi N, Ishida T, Ohara Y, Yoshizaki T, Kawara F, Umegaki E, Azuma T. Feasibility and safety of endoscopic submucosal dissection for lower rectal tumors with hemorrhoids. World J Gastroenterol. 2016;22:6268-6275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Probst A, Ebigbo A, Märkl B, Schaller T, Anthuber M, Fleischmann C, Messmann H. Endoscopic submucosal dissection for early rectal neoplasia: experience from a European center. Endoscopy. 2017;49:222-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 17. | Shigoka M, Koganezawa I, Yokozuka K, Miyoshi K, Tomita K, Tabuchi S, Chiba N, Katayanagi S, Nagakawa Y, Katsumata K, Tsuchida A, Kawachi S. [A Case of Early Rectal Cancer Recurring as Liver Metastasis Nine Months after ESD]. Gan To Kagaku Ryoho. 2019;46:2285-2287. [PubMed] |
| 18. | Li A, Wang H, Zuo Q, Fu C. [Analysis of the factors in the disease-free interval of metachronous pulmonary metastasis from rectal cancer]. Zhonghua Wei Chang Wai Ke Za Zhi. 2016;19:562-565. [PubMed] |
| 19. | Ahmadi N, Brown KGM, Lee P, Quinn M, Austin KKS, Solomon MJ. Is neoadjuvant chemoradiotherapy sufficient in patients with advanced rectal malignancy and positive extra-mesorectal lateral lymph nodes? Colorectal Dis. 2020;22:689-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Malakorn S, Yang Y, Bednarski BK, Kaur H, You YN, Holliday EB, Dasari A, Skibber JM, Rodriguez-Bigas MA, Chang GJ. Who Should Get Lateral Pelvic Lymph Node Dissection After Neoadjuvant Chemoradiation? Dis Colon Rectum. 2019;62:1158-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 21. | Agger E, Åkerlund V, Ekberg O, Jörgren F, Lydrup ML, Buchwald P. Management, treatment and prognostic significance of lateral lymph node metastases in rectal cancer-a regional cohort study. Int J Colorectal Dis. 2021;36:2707-2714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Williamson JS, Quyn AJ, Sagar PM. Rectal cancer lateral pelvic sidewall lymph nodes: a review of controversies and management. Br J Surg. 2020;107:1562-1569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |