Published online Nov 26, 2022. doi: 10.12998/wjcc.v10.i33.12352
Peer-review started: July 19, 2022
First decision: September 25, 2022
Revised: October 4, 2022
Accepted: October 19, 2022
Article in press: October 19, 2022
Published online: November 26, 2022
Processing time: 126 Days and 19.3 Hours
Currently, the implantation of permanent cardiac pacemakers entails mostly subclavian vein puncture, which is relatively simpler and easier to master. However, due to individual differences, some patients carry a narrow space between the clavicle and the first rib. If the range of activity of the upper limb is increased, the friction between the electrode wire and the bone gap leads to the breakage of the electrode wire, which is manifested by poor pacemaker perception and pacing.
A 68-year-old woman underwent permanent pacemaker implantation in our hospital because of third-degree atrioventricular block 6 years ago. At that time, the patient was recommended to have a dual-chamber permanent pacemaker implantation, and finally chose a single-chamber permanent pacemaker because she could not afford the cost. The patient has repeatedly lost consciousness for no obvious reason in the past 3 d, and went to our hospital for treatment. The chest X-ray showed that the pacemaker electrode was broken. After the patient was given a pacemaker electrode replacement, the patient did not continue to lose consciousness.
Because the electrodes implanted in the subclavian approach are close to the clavicle and the first rib, the pacemaker electrodes may wear out. If the patient loses consciousness again after the pacemaker is implanted, we should consider whether there is a pacemaker. The possibility of electrode breakage, and timely help the patient to replace the new pacemaker electrodes.
Core Tip: We treated a patient who was implanted with a single-chamber pacemaker 6 years ago. The patient experienced repeated loss of consciousness 3 d ago without obvious incentives. The patient did not continue to lose consciousness after the pacemaker electrodes were replaced.
- Citation: Zhu XY, Tang XH, Huang WY. Pacemaker electrode rupture causes recurrent syncope: A case report. World J Clin Cases 2022; 10(33): 12352-12357
- URL: https://www.wjgnet.com/2307-8960/full/v10/i33/12352.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i33.12352
Permanent pacemaker implantation is an effective treatment for bradyarrhythmia. This treatment method involves relatively simple surgery and is associated with minimal trauma. However, complications can still occur, including mainly hematoma, infection, hemopneumothorax, pacemaker syndrome, and electrode breakage and dislocation. The proportion of electrode fractures is about 1.2%[1]. Early fracture is mostly caused by operator inefficiency, while the late fracture is mostly attributed to small subclavian space and long-term friction between the electrode and the clavicle or rib. We describe a case of abnormal perception and pacing triggered by the rupture of permanent pacemaker electrode, resulting in recurrent syncope. Ultimately, the patient did not experience any loss of consciousness after the pacemaker and electrodes were replaced.
A 68-year-old female, who suffered from repeated loss of consciousness for 3 d went to the Jiujiang University Affiliated Hospital on June 9, 2022.
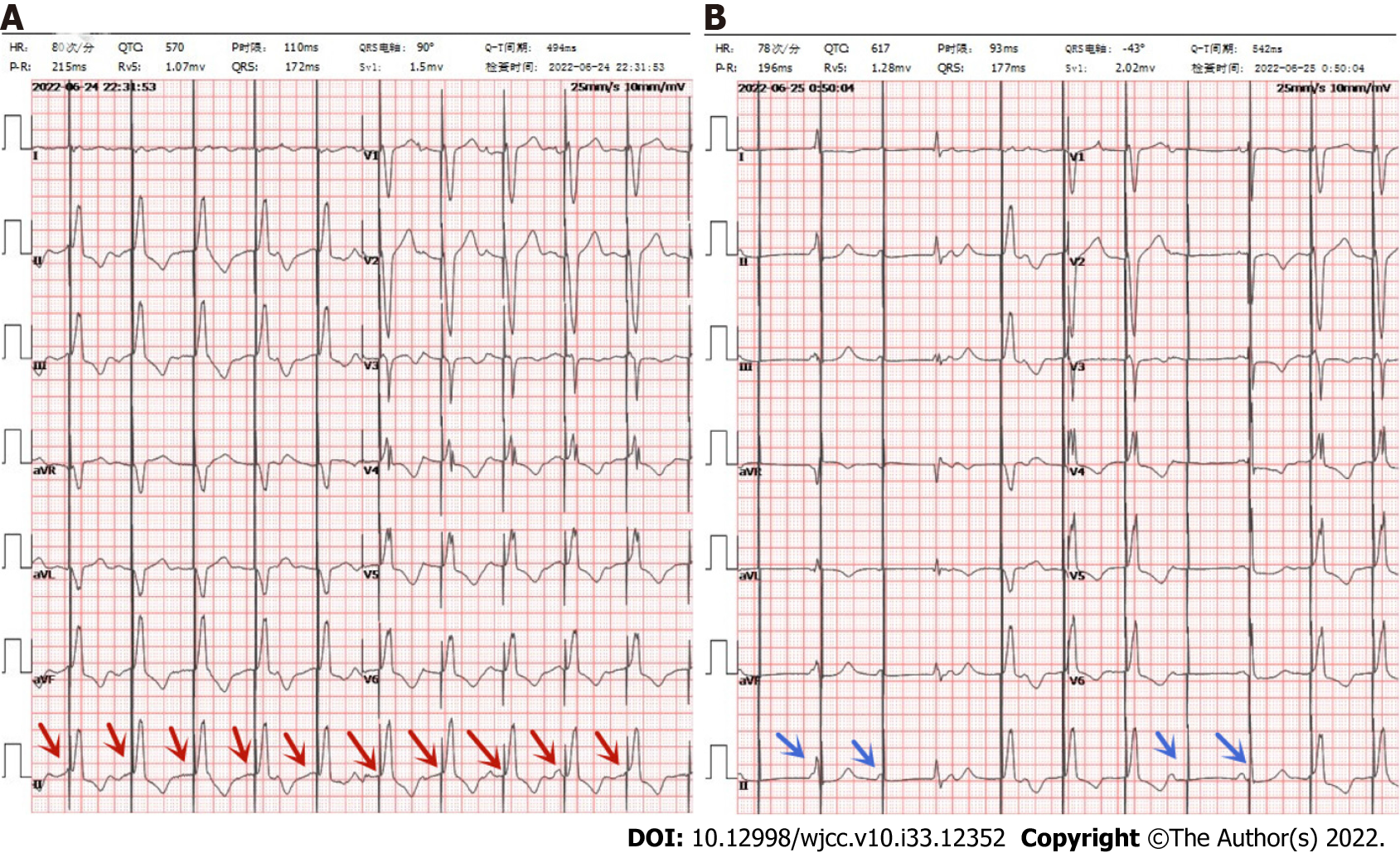
The patient complained that there was no obvious cause for loss of consciousness 3 d ago, and the family members complained that the patient's consciousness recovered 10 s later, but he did not pay attention to it at that time and did not diagnose and treat it. The patient complained of repeated episodes of loss of consciousness, especially when turning sideways. He went to the emergency department of our hospital for treatment, and the electrocardiogram showed a pacemaker electrocardiogram (Figure 1A). Interestingly, when the patient was sitting on the bed and describing his medical history, she suddenly said that she had amaurosis symptoms, and the bedside electrocardiogram (ECG) monitor showed intermittent poor pacing, which was recorded in time by the ECG (Figure 1B). When the heart resumed full pacing, the patient complained of dizziness and amaurosis symptoms relieved, and the pacemaker programming indicated that the electrode impedance was 323 ohms, and the pacing threshold was 5v.
The patient had a history of hypertension for 10 years. She took amlodipine besylate 5 mg QD regularly to control her blood pressure, noting that the blood pressure level was controlled well. She did not take any other medications. The patient denied history of coronary heart disease, cerebral infarction, diabetes.
The patient denied smoking, drinking history, and family disease history.
Body temperature, 36.3 ℃; breathing, 20 breaths/min; blood pressure, 114/70 mmHg; heart rate, 80 beats/min. Nerve examination and physical examination showed no abnormality
No abnormality is found in blood routine test, liver function, kidney function, electrolyte, thyroid function, blood coagulation function and stool routine test.
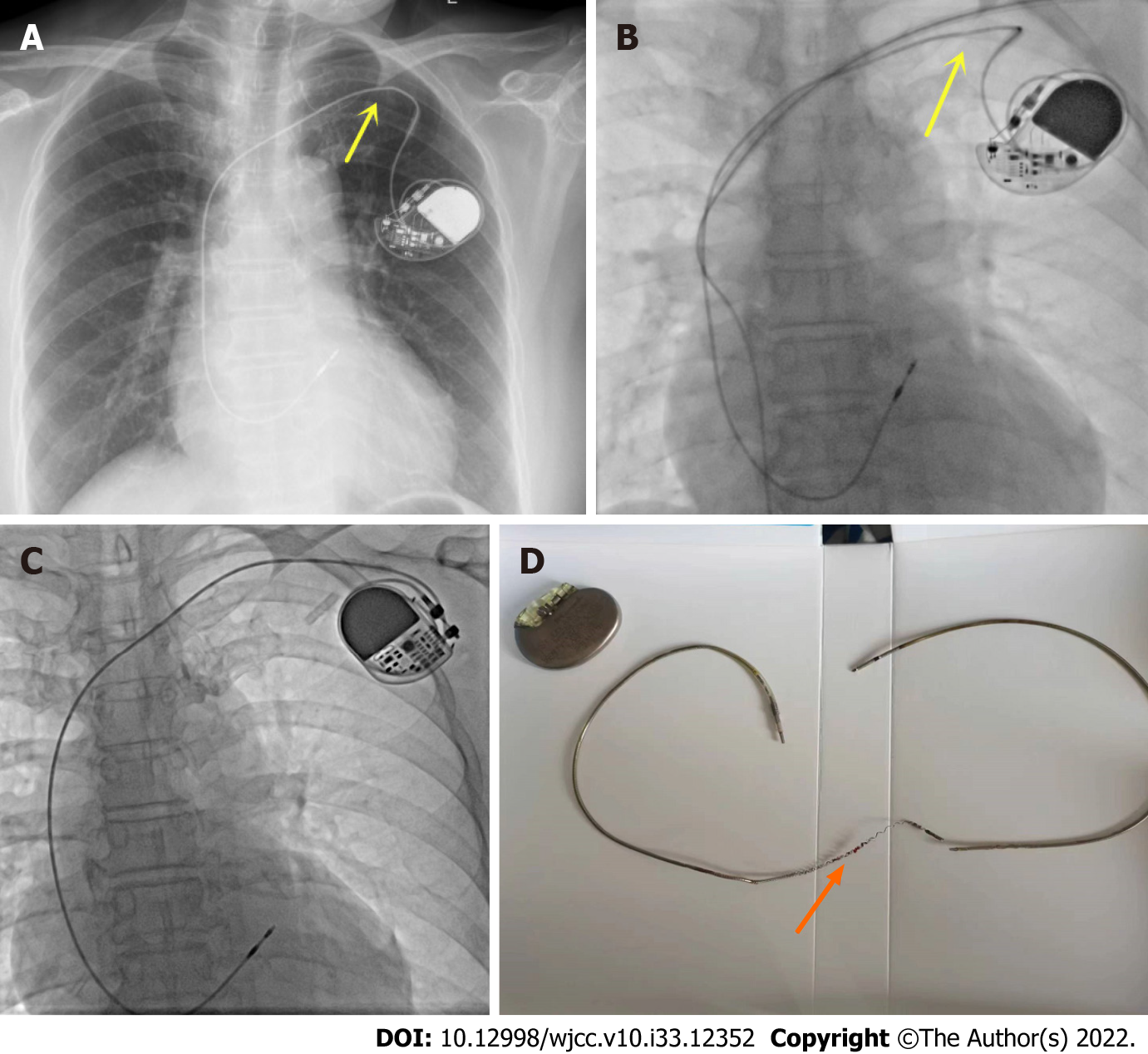
Brain computed tomography showed no abnormality, Chest X-ray showed a broken electrode line at the junction of the left clavicle and the first rib (Figure 2A and B).
Fractured pacemaker electrodes resulted in poor pacing, and the patient experienced repeated loss of consciousness.
Because the patient's pacemaker was implanted 6 years ago, the pacemaker and electrode replacement surgery were considered after full communication with the patient's family. The vascular puncture site was also adjusted from the subclavian vein to the axillary vein puncture, and the original electrodes were removed. And implanted new electrodes and pacemaker (Figure 2C and D).
The patient had good pacing after surgery, no further loss of consciousness, and was discharged from the hospital on July 7, 2022.
Permanent pacemaker plays an important role in the treatment of symptomatic bradyarrhythmia, Syncope can be induced by multiple factors. However, syncope triggered by cardiac causes often indicates poor prognosis and high mortality[2]. The causes of syncope in patients with permanent cardiac pacemakers are mostly neurogenic, hemodynamic instability caused by ventricular tachycardia, pacemaker sensing and pacing dysfunction due to abnormalities associated with pacemaker and lead. Syncope caused by broken pacemaker leads accounts for the least proportion of these cases. Subclavian vein puncture is the preferred method for pacemaker electrode implantation, because of its high success rate, fewer complications, and relative simplicity and user-friendly features. The implantation of electrodes from the subclavian vein route is usually done through a narrow space consisting of the clavicle, ribs, muscles and ligaments[3]. The sternoclavicular joint in this area is the joint between the sternal ribs and the scapula, which is involved in the movement of the thoracolumbar region[3]. Because of the relative structural complexity, the pacemaker lead may be clamped, which leads to wear and tear of the pacemaker electrode during hand and shoulder movements, and breakage of the electrode. In some patients, this position can lead to subclavian crush syndrome, resulting in damaged wire. Magney et al[4] reported anatomical studies involving cadavers that lead entrapment in the clavicle and first rib rather than friction resulted in lead damage.
In this case, subclavian vein puncture was used. Imaging revealed a medial puncture site and sub-clavicular electrode fracture site. Considering that the electrode fracture was related to the selection of puncture site, the reduced impedance suggested that the electrode insulation layer was damaged. The subsequent electrode fracture was related to pacemaker extrusion, traction and wear under the clavicle, which was also a disadvantage of subclavian puncture and electrode implantation. Axillary vein or cephalic vein pathway prevents electrode damage induced by subclavian puncture. Compared with the strong medial subclavian vein access, the cephalic or axillary vein puncture significantly reduced this complication[3,5]. Implantation of pacemaker electrodes via axillary or cephalic vein incision can significantly reduce the risk of electrode wear[3]. A meta-analysis showed that compared with subcla
Electrode breakage after permanent pacemaker implantation can be prevented by the following precautions: (1) The puncture point in subclavian vein puncture should be as close to the outside as possible to reduce the angle between the puncture needle and the skin, and avoid compression and friction of the locking rib triangle on the electrode line, or axillary vein or cephalic vein puncture may be used instead; (2) The range of motion of the upper limb on the operated side should be appropriate to avoid repeated twisting of electrode wires and prevent metal fatigue leading to fracture; and (3) The electrode wire should not be clamped with vascular forceps during the operation to prevent the risk of breakage of the electrode wire caused by human intervention.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Ghannam WM, Egypt; M.D. HA, Italy; Moussa BS; Salman I, Czech Republic S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Alt E, Völker R, Blömer H. Lead fracture in pacemaker patients. Thorac Cardiovasc Surg. 1987;35:101-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Yasa E, Ricci F, Holm H, Persson T, Melander O, Sutton R, Hamrefors V, Fedorowski A. Pacing therapy in the management of unexplained syncope: a tertiary care centre prospective study. Open Heart. 2019;6:e001015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 3. | Chan NY, Kwong NP, Cheong AP. Venous access and long-term pacemaker lead failure: comparing contrast-guided axillary vein puncture with subclavian puncture and cephalic cutdown. Europace. 2017;19:1193-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Magney JE, Flynn DM, Parsons JA, Staplin DH, Chin-Purcell MV, Milstein S, Hunter DW. Anatomical mechanisms explaining damage to pacemaker leads, defibrillator leads, and failure of central venous catheters adjacent to the sternoclavicular joint. Pacing Clin Electrophysiol. 1993;16:445-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 119] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Atti V, Turagam MK, Garg J, Koerber S, Angirekula A, Gopinathannair R, Natale A, Lakkireddy D. Subclavian and Axillary Vein Access Versus Cephalic Vein Cutdown for Cardiac Implantable Electronic Device Implantation: A Meta-Analysis. JACC Clin Electrophysiol. 2020;6:661-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Benz AP, Vamos M, Erath JW, Hohnloser SH. Cephalic vs. subclavian lead implantation in cardiac implantable electronic devices: a systematic review and meta-analysis. Europace. 2019;21:121-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Morrison TB, Rea RF, Hodge DO, Crusan D, Koestler C, Asirvatham SJ, Bradley D, Shen WK, Munger TM, Hammill SC, Friedman PA. Risk factors for implantable defibrillator lead fracture in a recalled and a nonrecalled lead. J Cardiovasc Electrophysiol. 2010;21:671-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Udo EO, Zuithoff NP, van Hemel NM, de Cock CC, Hendriks T, Doevendans PA, Moons KG. Incidence and predictors of short- and long-term complications in pacemaker therapy: the FOLLOWPACE study. Heart Rhythm. 2012;9:728-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 421] [Article Influence: 32.4] [Reference Citation Analysis (0)] |