Published online Nov 26, 2022. doi: 10.12998/wjcc.v10.i33.12240
Peer-review started: March 23, 2022
First decision: May 30, 2022
Revised: June 12, 2022
Accepted: October 17, 2022
Article in press: October 17, 2022
Published online: November 26, 2022
Processing time: 244 Days and 15 Hours
The presence of dens invaginatus (DI) complicates treatment of any tooth, from diagnosis to access cavity and biomechanical preparation and obturation. Reports of successful non-surgical management of DI type IIIB in maxillary lateral incisor are rare. Here, we report such a case, with three root canals and a long follow-up.
A 13-year-old female patient presented with mild pain in the maxillary right lateral incisor (#7) for 10-15 d. On examination, the tooth was slightly rotated, with slight tenderness on percussion and grade I mobility but with no caries, pockets or restorations and non-vital pulp (via vitality tests). Radiographic examination revealed unusual configuration of the tooth’s root canals, with an enamel-lined invagination extending to the apex, suggesting the possibility of DI Oehler’s type IIIB and a periapical radiolucency. Widening the access cavity lingually revealed one distinct buccal orifice and two distinct palatal orifices; under higher magnification of a dental operating microscope (DOM), the mesio-palatal and disto-palatal orifices were observed as connected by a C-shaped groove. The root canals were prepared with hand K-files following a step-back technique, and obturated using a combination technique of lateral condensation and vertical compaction. At the 6-year follow-up, the patient was asymptomatic, and the periapical radiography displayed significant healing around the apical end of the root.
Proper knowledge of unusual root canal anatomy is required in treating DI. Conventional methods of root canal treatment can successfully resolve such complex cases, facilitated by DOM and cone-beam computed tomography.
Core Tip: This case report describes the successful non-surgical management of dens invaginatus type IIIB in a maxillary lateral incisor with three root canals. Access cavity preparation revealed one distinct buccal orifice and two palatal orifices (mesio-palatal and disto-palatal) connected by a C-shaped groove, observed under a dental operating microscope. The root canals were prepared with hand K-files following the step-back technique and obturated using a combination technique of lateral condensation and vertical compaction. At the 6-year follow-up, the patient was asymptomatic and the periapical radiography displayed excellent healing around the apical end of the root.
- Citation: Arora S, Gill GS, Saquib SA, Saluja P, Baba SM, Khateeb SU, Abdulla AM, Bavabeedu SS, Ali ABM, Elagib MFA. Non-surgical management of dens invaginatus type IIIB in maxillary lateral incisor with three root canals and 6-year follow-up: A case report and review of literature. World J Clin Cases 2022; 10(33): 12240-12246
- URL: https://www.wjgnet.com/2307-8960/full/v10/i33/12240.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i33.12240
Success of endodontic treatment relies on myriad features of the clinical process, including accurate diagnosis, proper access cavity preparation, biomechanical preparation, obturation and post-endodontic restoration, as well as the physician’s knowledge of root canal anatomy. The majority of maxillary lateral incisors are one-rooted with single canal[1], but anatomical variations such as the presence of multiple canals[2-4], radicular palatal grooves[5], dens invaginatus (DI)[6], talon cusps with DI[7], enamel projections at cemento-enamel junction, etc[8] can complicate their endodontic management.
DI, a dental anomaly resulting from invagination of the enamel organ and dental papilla before the mineralization phase[9], has been reported to occur in 0.04%-12% of cases[10-12], and is bilateral in almost 43% of cases[13]. It is also referred to as dens in dente, dilated composite odontome, dents telescopes, and gestant anomaly in the literature[12]. The exact cause of DI formation is unknown, although trauma, genetics, infection of the tooth bud during development, and pressure from adjacent developing tooth germ have been suggested as causes. The clinical appearance of DI varies from normal morphology to conical-, peg- or barrel-shaped, large bucco-lingual dimensions, or association with talon cusp[3,5,7]. Based on Oehlers’s classification[14], according to depth of penetration and communication with the periodontal ligament or periapical tissue (determined radiographically), it is classified into the following three types/four subtypes: type I, an enamel-lined minor invagination that does not extend beyond the cementoenamel junction; type II, an invagination extending apically beyond the cementoenamel junction as a blind sac and which may or may not communicate with the dental pulp but has no communication with the periodontal ligament; type IIIA, an invagination penetrating through the root and laterally communicating with the periodontal space by a pseudo foramen without any direct communication with the pulp; and type IIIB, an invagination penetrating the root to communicate with the periodontal ligament at the apical foramen without any direct communication with the pulp. The presence of DI complicates the treatment of any maxillary lateral incisor, from diagnosis to access cavity and biomechanical preparation and obturation. This case report describes the comprehensive non-surgical endodontic management of a case of DI type IIIB in a lateral incisor with three root canals and 6-year follow-up. The aim of this case report is to highlight the importance of accurate diagnosis, treatment planning and use of the latest techniques and materials to achieve successful management of the rare type III DI.
A 13-year-old female patient presented to the Department of Endodontics with complaint of mild pain in the maxillary right anterior tooth that had persisted for 10 d.
The pain in the upper right anterior tooth started 10 d before presentation. During that time, the patient had taken anti-inflammatory drugs whenever she felt the pain. Since the drugs had only provided temporary pain relief, she wanted to get it checked.
The patient’s history of past illness was irrelevant.
The patient’s personal and family histories were unremarkable.
On physical examination, the maxillary right lateral incisor (tooth #7 by the universal numbering system) was found to be slightly rotated, without caries, restorations or fractures; it appeared identical to the maxillary left lateral incisor, without any coronal morphological variation. The tooth was slightly tender on percussion and had grade I mobility, but no pockets were detected. The tooth was considered non-vital as it did not respond to electric and thermal pulp vitality tests.
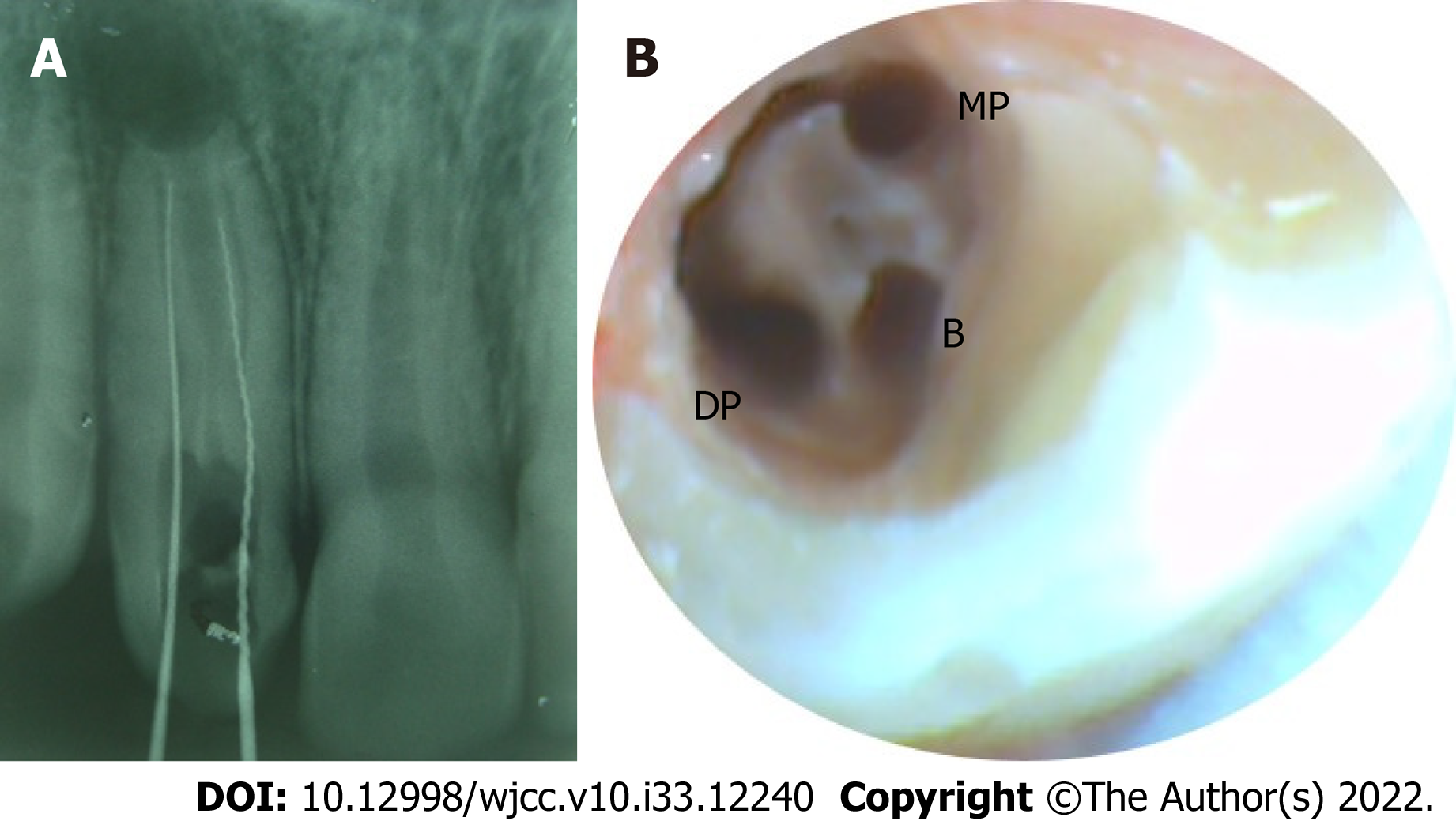
Radiographic examination (Figure 1A) revealed an unusual configuration of root canals in tooth #7, with an invagination extending to the apex, suggesting the possibility of DI Oehler’s type IIIB and a periapical radiolucency. A panoramic radiography (Figure 1B) was undertaken to ascertain the root canal anatomy of the maxillary lateral incisor on the other side of the arch, which was found to be normal.
Pulpal necrosis and symptomatic apical periodontitis with respect to tooth #7, with Oehler’s type IIIB DI.
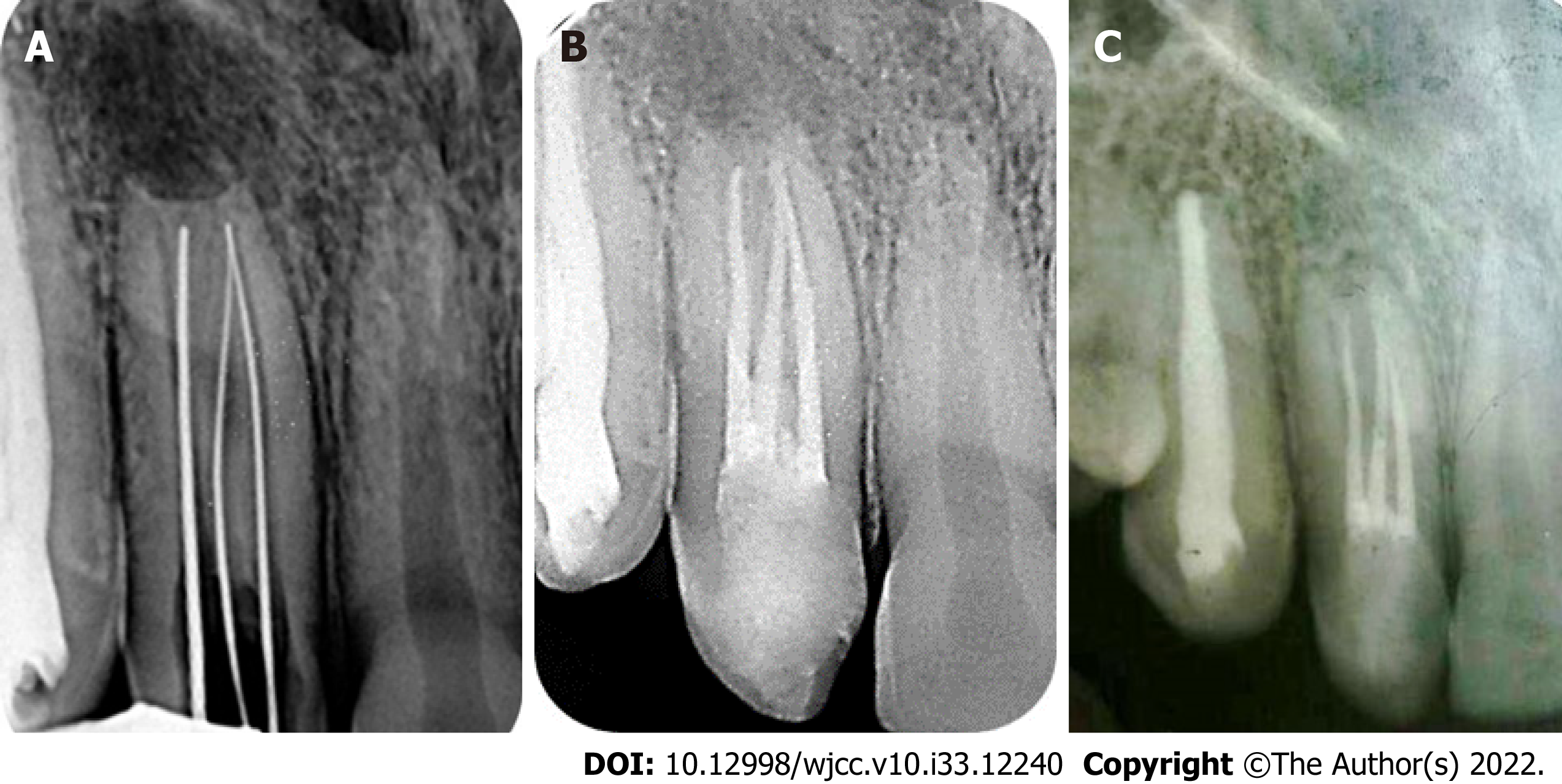
The patient and her guardian were informed about the details of diagnosis, complications associated with treatment, option of non-surgical root canal management, and possible surgical treatment or extraction. Informed consent for the non-surgical root canal treatment was obtained from the patient’s guardian as she was a minor at the time. Under local anesthesia [2% lignocaine with 1:100000 epinephrine (Xylocaine; Dentsply Pharmaceutical, York, PA, United States)], the access cavity was prepared using a rubber dam. The rubber dam was held in place with wedjets instead of clamps because of mal-occluded teeth. At first, access was gained to the two regular palatal root canals [mesio-palatal (MP) and disto-palatal (DP)] (Figure 2A), and then the third canal (buccal canal) was accessed through the invagination on the buccal side with the help of dental operating microscope (DOM) after the access cavity was modified. One distinct buccal orifice and two palatal orifices (MP and DP) connected by a C-shaped groove were observed after removal of the dentin roof and widening the access cavity under DOM (Figure 2B). The working length was determined using a Root ZX Apex Locator (Morita, Tokyo, Japan) and confirmed by periapical radiography (Figure 3A). Three canals were detected, including one buccal and two palatal (MP and DP), with the MP and buccal canals meeting at the apex; a firm hard stop was also felt at the apex. Coronal flaring was carried out using a Protaper SX file (Dentsply Sirona, Charlotte, NC, United States). The root canals were prepared using stainless steel hand K-files (Mani Inc., Utsunomiya, Japan) up to size 40 and a step-back technique. The preparation was facilitated by application of File-Eze lubricant (Ultradent, South Jordan, UT, United States).
Throughout the procedure, the canals were irrigated with 2.5% sodium hypochlorite activated by ultrasonic irrigation and 17% ethylenediamine tetraacetic acid. At the end of the procedure, the canals were dried using paper points (Dentsply Maillefer, Ballaigues, Switzerland), and calcium hydroxide (Metaapex; Meta Biomed Co. Ltd, Cheongju, Korea) was placed as an inter-appointment medicament and sealed with Cavit (3M ESPE AG, Seefeld, Germany). After 1 wk, the calcium hydroxide medicament was replaced with a new dressing of Metaapex. After 2 wk, the root canals were irrigated ultrasonically and the Metaapex was removed. The canals were dried and obturated using a combination technique of lateral condensation and vertical compaction of gutta percha with AH Plus sealer (Detrey-Dentsply, Konstanz, Germany) (Figure 3B). Finally, the access cavity was restored with Solitaire 2 composite resin (Heraeus Kulzer, Wehrheim, Germany).
At the first follow-up (1 wk post-restoration), the patient was asymptomatic. The family relocated abroad soon after that appointment; however, the patient revisited our clinic 6 years later and was completely asymptomatic. Clinical evaluation of tooth #7 revealed no sensitivity to percussion or palpation, and mobility within normal limits. Radiographic examination displayed significant periapical healing (Figure 3C), but slight resorption present at the apex of the tooth root, which might necessitate surgical intervention in the future. The patient was recommended to have follow-up visit at least once a year for examination.
Knowledge of root canal morphology and its anatomic variations is crucial for successful endodontic treatment. In most people, the maxillary lateral incisors have the simple root canal anatomy consisting of one root and one canal, but variations like DI, palatal groove, fusion, gemination and multiple root canals have been reported[1-8]. This case report describes a rare maxillary lateral incisor with DI (Oehler’s type IIIB) and three distinct root canals, including two regular palatal canals and one buccal canal through the invagination present on the buccal side. The management of such cases must start with accurate diagnosis of the anatomical condition. In DI, the crown morphology can be normal, peg- or barrel-shaped, and/or have larger dimensions than usual. Thus, any deviation from normal morphology should be viewed with suspicion; yet, it is important to remember that presence of normal morphology does not rule out DI. In the present case, the morphology was normal but the tooth was slightly rotated. Most of the time, the presence of deep foramen caecum is the only clinical sign of DI[15]. Indeed, our patient showed slight discoloration in the lingual pit of tooth #7, but no opening was present, though it could be microscopic and not penetrable by the probe. Since almost 43% of cases were bilateral[13], a panoramic X-ray was performed, and the contralateral maxillary incisor was found to be normal radiographically.
Multiple angulated radiography is recommended to get a clear picture of the internal tooth anatomy. For our case, radiographic examination revealed an Oehler’s type IIIB DI (with invagination running through the entire root length and forming a separate foramen) and periapical pathology. Thus, retrograde infection could have accounted for the observed necrosis of the pulp. In addition, the indirect communication through the defects might have affected the enamel and dentin surrounding the invagination, facilitating pathogenic access to the pulp, as suggested in previous studies[4,12,16]. The drawback of radiography offering a two-dimensional image with geometric distortion can be overcome by three-dimensional imaging using cone-beam computed tomography (CBCT). CBCT provides accurate assessment of complex root canal anatomy[17-20] and aids in accurate diagnosis, management and follow-up of such cases. As it delivers high radiation dose to the patient, though, it should be used cautiously, after weighing risk vs benefit in each case. Bearing in mind the young age of our patient and the lack of an in-house CBCT facility, this imaging modality was not used.
Management of DI depends on severity of the condition. Even if asymptomatic, treatment is necessary as deep invaginations are difficult to clean and access, leading to early caries and subsequent pulpal necrosis. The management options for severe cases include non-surgical endodontic treatment, surgical treatment, or a combination of the two[21-24]. Case reports have mentioned the treatment of invagination only[25], invagination and root canal[26] and the removal of DI with the help of DOM and subsequent root canal treatment[27]. In type III cases, the treatment depends upon status of pulp vitality, guiding the choice of the following two options: (1) Prophylactically treating the false canal (invaginated canal) as a separate entity, while maintaining the vitality of the root canals; (2) Endodontically treating both the false canal and true canal in the case of pulpal necrosis. In the present case, non-surgical root canal treatment was planned for the tooth since the pulp was necrosed. Initially, only access to the two regular root canals (palatal canals: MP and DP) was gained and then, with the use of DOM, access to the third canal (buccal canal) was gained through the invagination on the buccal side. Treating such cases under DOM has always proven to be beneficial, as highlighted in previous studies[14,26]. The two regular palatal canals (MP and DP) were joined by a C-shaped groove as the invagi
The irregular anatomy of invaginated canals makes the debridement difficult, so irrigation was performed with sodium hypochlorite using ultrasonic activation[28]. For shaping the root canals, rotary instruments were avoided as the enamel lining of the invagination and irregular anatomy can predispose to instrument fracture[29]. Hand K-files were used to prepare the canals, along with the help of lubricant to facilitate the shaping process[30]. In the present case, there was a firm stop present at the apex, so the conventional canal preparation using the step-back technique was carried out and obturation was completed using a combination technique of lateral condensation and vertical compaction. To judge a treatment success, evidence of radiographic healing through longer follow-ups is necessary. For our patient, clinical examination demonstrated asymptomatic condition and radiographic examination demonstrated healing 6 years after the treatment.
The prognosis of DI cases has not been sufficiently studied and most data regarding the condition are available in case reports[4,5,18,19,23-27,29,30]. The follow-up period of successfully managed DI cases varies from 6 mo[4] to 27 years[5], indicating a good prognosis; although, a well-designed systematic review and meta-analysis or a large-sample original research study is needed to draw definite conclusions on prognosis. CBCT was not performed during diagnosis, which can be considered a limitation of the present case report, but the underlying radiation dose concerns for patient age justify our caution. Of note, our patient did not consent to a CBCT examination during her subsequent follow-up visit. Another limitation is the lack of annual follow-up radiographic examinations, which could have shown the progression of healing; however, this was precluded by the patient’s migration abroad.
Treatment of DI requires thorough knowledge of the general internal anatomy of root canals and the effects of invaginations on the anatomy of the tooth. Though CBCT imaging can vastly improve the chances of successful management by enhanced visualization, consideration must be given to the risk vs benefits of this radiation-based modality for each case. Conventional root canal treatments can successfully treat such complex cases by following the basic principles of debridement, irrigation and obturation, but will be greatly facilitated by the use of DOM.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abu Hasna A, Brazil; Ghosh S, India S-Editor: Xing YX L-Editor: Ma JY-MedE P-Editor: Xing YX
| 1. | Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58:589-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1000] [Cited by in RCA: 1103] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 2. | Kottoor J, Murugesan R, Albuquerque DV. A maxillary lateral incisor with four root canals. Int Endod J. 2012;45:393-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 3. | Lee MH, Ha JH, Jin MU, Kim YK, Kim SK. Endodontic treatment of maxillary lateral incisors with anatomical variations. Restor Dent Endod. 2013;38:253-257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Nosrat A, Schneider SC. Endodontic management of a maxillary lateral incisor with 4 root canals and a dens invaginatus tract. J Endod. 2015;41:1167-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. |
Matthews DP, Hansen DE.
Interdisciplinary management of a maxillary central incisor with a palato-radicular groove: A case report with 27 years follow-up |
| 6. | Ali A, Arslan H, Jethani B. Conservative management of Type II dens invaginatus with guided endodontic approach: A case series. J Conserv Dent. 2019;22:503-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Ghosh S, Dhungel S, Subedi B, Pradhan S. Cooccurrence of Talon's Cusp with Dens Invaginatus in the Maxillary Lateral Incisor: A Case Report with Review of Literature. Case Rep Dent. 2022;2022:9165574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 8. | Babaji P. Bilateral supplemental maxillary incisors with both dens invaginatus and dens evaginatus in a non syndromic patient: a rare case report. J Clin Diagn Res. 2015;9:ZJ01-ZJ02. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Hülsmann M. Dens invaginatus: aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J. 1997;30:79-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 94] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Hovland EJ, Block RM. Nonrecognition and subsequent endodontic treatment of dens invaginatus. J Endod. 1977;3:360-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 89] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Kirzioğlu Z, Ceyhan D. The prevalence of anterior teeth with dens invaginatus in the western Mediterranean region of Turkey. Int Endod J. 2009;42:727-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Alani A, Bishop K. Dens invaginatus. Part 1: classification, prevalence and aetiology. Int Endod J. 2008;41:1123-1136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 122] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 13. | Gotoh T, Kawahara K, Imai K, Kishi K, Fujiki Y. Clinical and radiographic study of dens invaginatus. Oral Surg Oral Med Oral Pathol. 1979;48:88-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Oehlers FA. Dens invaginatus (dilated composite odontome). I. Variations of the invagination process and associated anterior crown forms. Oral Surg Oral Med Oral Pathol. 1957;10:1204-18 contd. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 275] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Jung M. Endodontic treatment of dens invaginatus type III with three root canals and open apical foramen. Int Endod J. 2004;37:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Beynon AD. Developing dens invaginatus (dens in dente). A quantitative microradiographic study and a reconsideration of the histogenesis of this condition. Br Dent J. 1982;153:255-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Patel S. The use of cone beam computed tomography in the conservative management of dens invaginatus: a case report. Int Endod J. 2010;43:707-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Teixido M, Abella F, Duran-Sindreu F, Moscoso S, Roig M. The use of cone-beam computed tomography in the preservation of pulp vitality in a maxillary canine with type 3 dens invaginatus and an associated periradicular lesion. J Endod. 2014;40:1501-1504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Kfir A, Telishevsky-Strauss Y, Leitner A, Metzger Z. The diagnosis and conservative treatment of a complex type 3 dens invaginatus using cone beam computed tomography (CBCT) and 3D plastic models. Int Endod J. 2013;46:275-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | M Gul S, Adnan, F Umer. “A variant of the current dens invaginatus classification”. Frontiers in Dentistry. 2020;17:28. |
| 21. | Sauveur G, Sobel M, Boucher Y. Surgical treatment of a lateroradicular lesion on an invaginated lateral incisor (dens in dente). Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 83: 703–706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Er K, Kustarci A, Ozan U, Tasdemir T. Nonsurgical endodontic treatment of dens invaginatus in a mandibular premolar with large periradicular lesion: a case report. J Endod. 2007;33:322-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 23. | Pai SF, Yang SF, Lin LM. Nonsurgical endodontic treatment of dens invaginatus with large periradicular lesion: a case report. J Endod. 2004;30:597-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Chaniotis AM, Tzanetakis GN, Kontakiotis EG, Tosios KI. Combined endodontic and surgical management of a mandibular lateral incisor with a rare type of dens invaginatus. J Endod. 2008;34:1255-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Goncalves A, Gonsalves M, Oliviera DP, Gonsalves N. Dens invaginatus type III:report of a case and 10 year follow up. Int Endod J. 2002;35:873-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Tsurumachi T, Hayashi M, Takeichi O. Non-surgical root canal treatment of dens invaginatus type II in maxillary lateral incisor. Int Endod J. 2002;35:309-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Girsch WJ, McClammy TV. Microscopic removal of dens invaginatus. J Endod. 2002;28:336-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Skoner JR, Wallace JA. Dens invaginatus: another use for the ultrasonics. J Endod. 1994;20:138-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Keleş A, Cakici F. Endodontic treatment of a maxillary lateral incisor with vital pulp, periradicular lesion and type III dens invaginatus: a case report. Int Endod J. 2010;43:608-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 30. | Lichota D, Lipski M, Woźniak K, Buczkowska-Radlińska J. Endodontic treatment of a maxillary canine with type 3 dens invaginatus and large periradicular lesion: a case report. J Endod. 2008;34:756-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |