Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11646
Peer-review started: July 27, 2022
First decision: August 22, 2022
Revised: September 5, 2022
Accepted: September 29, 2022
Article in press: September 29, 2022
Published online: November 6, 2022
Processing time: 91 Days and 22.1 Hours
Apnea caused by retrobulbar anesthesia is a very rare but severe complication during ophthalmic surgery.
We report a rare case of apnea caused by retrobulbar anesthesia, and emergency resuscitation was used. A 74-year-old female patient was diagnosed with rhegmatogenous retinal detachment in the right eye and planned to undergo vitrectomy under retrobulbar anesthesia. After the retrobulbar anesthesia in her right eye, she became unconscious and apneic. It was suggested that she had developed brainstem anesthesia. Assisted ventilation was initiated. Atropine 0.5 mg, epinephrine 1 mg, ephedrine 30 mg, and lipid emulsion were given. Five minutes later, her consciousness and breathing gradually returned, but with uncertain light perception in her right eye. Alprostadil 20 µg was given, and after 2 h her visual acuity resumed to the preoperative level.
Brainstem anesthesia is a serious complication secondary to retrobulbar anesthesia. Medical staff should pay attention to the identification of brainstem anesthesia and be familiar with the emergency treatment for this complication.
Core Tip: Apnea caused by retrobulbar anesthesia is a very rare but severe complication. Failure to recognize brainstem anesthesia or delaying the treatment may be life threatening. We report a rare case of apnea caused by retrobulbar anesthesia, and emergency resuscitation was used. Assisted ventilation and vasodilator treatment were used, and the consciousness and breathing of the patient was gradually recovered. The mechanism of retrobulbar anesthesia is varied, but a skillful operation of retrobulbar anesthesia is important. Doctors and nurses should be aware of the potential risk of retrobulbar anesthesia, and be familiar with the resuscitation procedures.
- Citation: Wang YL, Lan GR, Zou X, Wang EQ, Dai RP, Chen YX. Apnea caused by retrobulbar anesthesia: A case report. World J Clin Cases 2022; 10(31): 11646-11651
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11646.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11646
Retrobulbar anesthesia is commonly used in ophthalmic surgeries, especially for posterior segment surgeries, including vitrectomy, external-route surgery, etc. By injecting anesthetic drug into the posterior musculus cone of the eye to block the III, IV, and VI cranial nerves and the ciliary nerves, rapid analgesia can be achieved. Compared with topical anesthesia (often used for short-time or superficial anterior segment surgeries), peribulbar anesthesia (frequently used for long-time anterior segment surgery) or subtenon capsule injection (which requires conjunctival sac incision and subtenon region blunt dissection), retrobulbar anesthesia is a more effective and convenient anesthesia method for posterior segment surgeries.
However, retrobulbar anesthesia is associated with risk of complications[1], including: (1) Local complications, such as retrobulbar hemorrhage, eyeball perforation, optic nerve injury and retinal vascular occlusion; and (2) systemic complications, such as the ocular-heart reflex and brainstem anesthesia. Among them, brainstem anesthesia is very rare (with an incidence rate of only 0.06%-0.2%) but severe, as anesthetic agents gain access to the central nervous system, causing apnea and cardiac arrest[2]. Failure to recognize brainstem anesthesia and delaying treatment may be life threatening[3].
We report a case of apnea and unconsciousness caused by retrobulbar anesthesia, with saturation of pulse oxygen (SpO2) that dropped to 80%; emergency resuscitation was performed.
A 74-year-old female patient presented to the hospital with decreased vision in the right eye that had persisted for 1 mo.
The patient reported that her symptoms had started in her right eye 1 mo prior.
The patient had a 5-year history of hypertension but denied cerebrovascular diseases or drug allergies. She reported that she had not previously experienced any procedure that necessitated anesthesia.
The patient denied any family history of cardiovascular or cerebrovascular diseases.
Physical examination showed blood pressure (BP) of 111/57 mmHg, respiratory rate (RR) of 17 breaths/min (bpm), SpO2 of 98%, and heart rate (HR) of 75 bpm.
The patient’s right eye visual acuity was HM/30 cm. Retinal detachment with a horseshoe-shaped hole was found in the superior temporal fundus.
The patient’s chest radiography and electrocardiograph examinations gave normal results.
Rhegmatogenous retinal detachment in the right eye.
The patient planned to undergo a vitrectomy with retrobulbar anesthesia of her right eye.
The operation started by performing a retrobulbar anesthesia. No narcotics or muscle relaxants were used prior to retrobulbar anesthesia. The patient was instructed to lay in the supine position. A 28 G needle was used to penetrate the position of the junction of the middle 1/3 and the outer 1/3 of the infraorbital margin. After puncturing the skin and inserting the needle approximately 1.5 cm, the needle was turned towards the foramen magnum and was then slowly advanced approximately 2 cm, with no return of blood. Then, 2 mL (40 mg) lidocaine and 2 mL (20 mg) ropivacaine were injected with slight resistance. Six minutes later, the patient was unconscious and unresponsive. Her right eye was dilated because of drugs, and the pupillary light reflex of the contralateral eye was sluggish. Immediately, an electrocardiogram (ECG) was applied for monitoring; her BP was 150/70 mmHg, her HR was 98 bpm, her RR was undetectable, and her SpO2 dropped to 80%.
The ophthalmologist called the anesthesia team to assist in resuscitation. Mask-assisted ventilation was given, and an intravenous catheter was placed. It was considered that she developed brainstem anesthesia, so the anesthesiologist gave the patient 0.5 mg atropine, 1 mg epinephrine, and 30 mg ephedrine intravenously. Considering local anesthetic poisoning, an intravenous infusion of 250 mL of 20% lipid emulsion (1.5 mL/kg 20% lipid emulsion bolus over 1 min, followed by 0.25 mL/kg/min of infusion) was given. After 5 min, the patient regained consciousness. The patient’s spontaneous breathing was restored with 16 beats/min. The operation was cancelled, and the patient returned to the ward under SpO2, BP, and ECG monitoring. One hour after leaving the operation room, visual acuity in her right eye was uncertain light perception, which was checked at bedside. Alprostadil 20 μg was given, and her vision gradually recovered to the preoperative state.
Two hours after the operation, head computed tomography scan identified a bubble at the posterior of patient’s right eye (Figure 1). The ECG and myocardial enzyme test results were roughly the same as at admission. She had no recall of the incident.
This patient had a clear diagnosis of rhegmatogenous retinal detachment in the right eye, and vitrectomy was indicated[4]. Her vital signs were good preoperatively, and retrobulbar anesthesia was planned.
The patient was unconscious and apneic shortly after retrobulbar anesthesia, so systematic complications such as brainstem anesthesia, anesthetic allergy, and ocular-heart reflex were primarily considered. Brain stem anesthesia was regarded as the most likely complication, because she did not have any allergic history, and her HR was not decreased. The mechanism of brainstem anesthesia may be as follows[5]: (1) The anesthetic could have been injected into the nerve sheath and then could have entered the cerebrospinal fluid, causing a loss of consciousness, apnea, etc; (2) The anesthetic could have entered the blood, causing central anesthesia; and (3) There could be an anaphylactic reaction to the drug. For this patient, loss of consciousness and apnea occurred after retrobulbar anesthesia were found after her recovery from anesthesia. For the differentiation of mechanisms of intraarterial and intrasheath injection, if inadvertent intraarterial injection was achieved, the onset of symptoms such as loss of consciousness, apnea, and seizures would be expected within seconds, while brainstem anesthesia from a nerve sheath injection occurs over a matter of minutes, mostly 5–50 min[2]. For this case, the mechanism may have involved accidental intrasheath injection, because the difficulty in breathing started about 6 min after the injection. The patient did not have any seizure or retrobulbar hemorrhage, and there was no return of blood during the puncture process; therefore, respiratory arrest was unlikely to be caused by intravascular injection. We also considered that the anesthetics and/or bubbles in the needle were injected into the neurovascular tissues around the eye, causing an increase in local pressure, which led to a transient compression of the optic nerve or pressed the anesthetic into the sheath of optic nerve, causing brainstem anesthesia.
Brainstem anesthesia is a rare but severe complication caused by retrobulbar surgery. Patients often develop symptoms within 2 min after injection of the aesthetic drug, and severe symptoms occur within 10-20 min and gradually improve after 2-3 h. Clinical manifestations include amaurosis, hearing loss, dysphagia, dysarthria, contralateral oculomotor nerve, and trochlear nerve palsy. Severe symptoms include disturbances of consciousness, respiratory failure, and cardiac arrest. Therefore, early detection of brainstem anesthesia is important, especially during the first 20 min after retrobulbar injection. During this period, careful monitoring of the patient’s vital signs is important.
Apnea caused by retrobulbar anesthesia is rarely reported. Tong et al[6] reported a patient who was unresponsive 1 min after retrobulbar anesthesia. After oxygen therapy and an intravenous injection of nicosemide and nicardipine, the patient did not improve and subsequently developed respiratory arrest and ventricular fibrillation. Emergency chest compressions, tracheal intubation, and defibrillation were given, and he was transferred to an emergency center. However, the patient died 4 d later due to cerebral hypoxia and edema. Tolesa et al[7] reported a patient who regained consciousness and spontaneous breathing after being given oxygen via a mask, intravenous fluids, and an intravenous injection of atropine 1 mg.
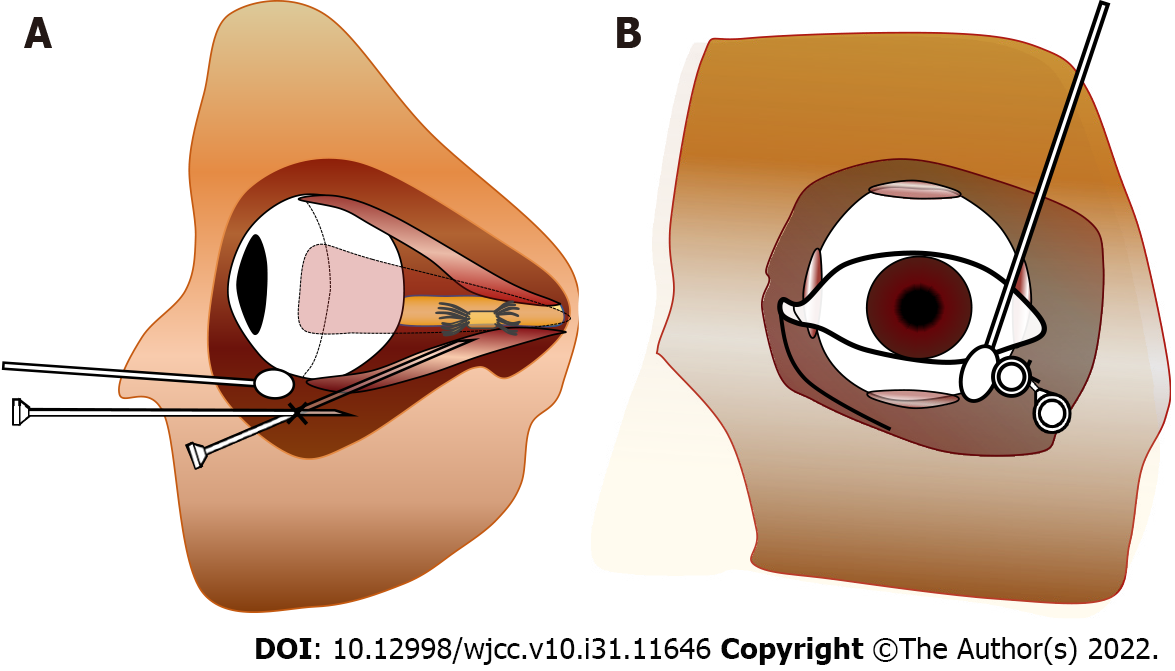
To prevent brainstem anesthesia, skillful operation of retrobulbar anesthesia is important. First, a low volume of anesthetic drug is recommended to reduce systematic side effect. According to our clinical observations, the dose of 2 mL (generally 2-5 mL) anesthetic is enough for a proper anesthetic effect, if the anesthetic infiltrates the ciliary ganglion. Second, longer needles have deeper puncture, which may increase the risk of penetrating the blood vessels or optic nerve sheaths, so the maximum needle length recommended for retrobulbar block is 31 mm according to Kostadinov et al[8]. A blunt needle is less likely to penetrate the optic nerve sheath, but its insertion may be painful and traumatic. Third, it is recommended that the patient look straight forward rather than upwards to avoid stabbing the blood vessels or the optic nerve. Figure 2 illustrates a trick of using cotton-bud to assist retrobulbar anesthesia.
For the treatment of brainstem anesthesia[9,10], first, the operator should immediately stop the injection of the anesthetic drugs. Second, doctors should identify the early clinical manifestations of brainstem anesthesia in a timely manner, and emergency measures such as ECG monitoring, oxygen inhalation, and the placement of an intravenous catheter should be performed immediately. Timely symptomatic treatment can reduce the adverse prognosis caused by brain hypoxia. Then, the patient should be treated with central stimulants and BP stabilizers, including atropine, epinephrine, etc. Meanwhile, anesthetic drug antagonists such as lipid emulsions can be given to reduce the central inhibitory effect of the anesthetic drugs by wrapping lipophilic anesthetics[11]. If there is a further decrease in BP, blood oxygen saturation, or respiratory and cardiac arrest, resuscitation measures such as the usage of pressor agents, tracheal intubation, mechanical ventilation and even chest compressions can be considered; the patient should also receive intensive care after surgery.
Brainstem anesthesia is a serious complication caused by retrobulbar anesthesia. Doctors and nurses should be aware of the potential risk, be familiar with the resuscitation procedures, and treat the relevant symptoms in a timely manner.
Wang YL would like to thank the department of Anesthesiology, Medical, and Pharmacy of Peking Union Medical College Hospital for their support of the treatment of the patient.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Stachiv I, Czech Republic; Tovichien P, Thailand S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Morley M, Menke AM, Nanji KC. Ocular Anesthesia-Related Closed Claims from Ophthalmic Mutual Insurance Company 2008-2018. Ophthalmology. 2020;127:852-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Faccenda KA, Finucane BT. Complications of regional anaesthesia Incidence and prevention. Drug Saf. 2001;24:413-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 105] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 3. | Javitt JC, Addiego R, Friedberg HL, Libonati MM, Leahy JJ. Brain stem anesthesia after retrobulbar block. Ophthalmology. 1987;94:718-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 124] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Feltgen N, Walter P. Rhegmatogenous retinal detachment--an ophthalmologic emergency. Dtsch Arztebl Int. 2014;111:12-21; quiz 22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Gunja N, Varshney K. Brainstem anaesthesia after retrobulbar block: a rare cause of coma presenting to the emergency department. Emerg Med Australas. 2006;18:83-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Tong Y, Dai WZ. [A Fatal Case Of Postbulbar Anesthesia With Respiratory Depression Syndrome]. Zhongguo Shequ Yishi. 2019;34:56-57. [DOI] [Full Text] |
| 7. | Tolesa K, Gebreal GW. Brainstem Anesthesia after Retrobulbar Block: A Case Report and Review of Literature. Ethiop J Health Sci. 2016;26:589-594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Kostadinov I, Hostnik A, Cvenkel B, Potočnik I. Brainstem Anaesthesia after Retrobulbar Block. Open Med (Wars). 2019;14:287-291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Li WS, Chen XD. [Prevention and Management of Ophthalmic Anaesthesia-related Complications]. Zhonghua Shiyan Yanke Zazhi. 2017;5:391-395. [DOI] [Full Text] |
| 10. | Katsev DA, Drews RC, Rose BT. An anatomic study of retrobulbar needle path length. Ophthalmology. 1989;96:1221-1224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 96] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Ok SH, Hong JM, Lee SH, Sohn JT. Lipid Emulsion for Treating Local Anesthetic Systemic Toxicity. Int J Med Sci. 2018;15:713-722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 80] [Article Influence: 11.4] [Reference Citation Analysis (0)] |