Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11555
Peer-review started: June 5, 2022
First decision: August 21, 2022
Revised: September 3, 2022
Accepted: September 27, 2022
Article in press: September 27, 2022
Published online: November 6, 2022
Processing time: 143 Days and 19.8 Hours
Acute myocardial infarction (AMI) can be induced by several factors. However, AMI induced by Kounis syndrome (an allergic reaction) is extremely rare and is highly susceptible to misdiagnosis.
A 70-year-old man presented after suffering an allergic reaction that caused chest pain triggered upon eating ice cream. Troponin I was found to be elevated, and an electrocardiogram showed ST-segment elevation. The diagnosis was AMI. He underwent two coronary angiographies, with one intravascular ultrasound during hospitalization showing no evidence of atherosclerotic coronary artery disease. The final diagnosis was vasospastic myocardial infarction due to Kounis syndrome. The patient was then treated with hydrocortisone and intravenous antihistamines, and his chest pain symptoms resolved.
Allergic reactions (such as Kounis syndrome) can cause serious damage to the heart. Physicians should be alert to the consequences and avoid misdiagnosis.
Core Tip: Kounis syndrome is an acute coronary syndrome caused by an allergic reaction. However, Kounis syndrome is a rare cause of acute myocardial infarction. We describe one of these rare cases in which the patient’s troponin I levels were elevated and electrocardiogram showed ST-segment elevation. After a course of hydrocortisone and antihistamines, the patient’s chest pain was resolved.
- Citation: Xu GZ, Wang G. Acute myocardial infarction due to Kounis syndrome: A case report. World J Clin Cases 2022; 10(31): 11555-11560
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11555.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11555
Acute myocardial infarction (AMI) is a life-threatening cardiovascular event. The common inducements of AMI include overwork, excitement, overeating, cold stimulation, constipation and cannabis[1]. Kounis syndrome[2] (an allergic reaction) can also induce AMI, though it is a rare occurrence. Herein, we describe a 70-year-old man who suffered an allergic reaction causing chest pain that was triggered by eating ice cream. He was diagnosed with AMI.
This case report presents the clinical abnormalities of AMI caused by Kounis syndrome to avoid misdiagnosis of this rare event.
A 70-year-old Chinese man presented to the cardiac clinic with a complaint of chest pain that had persisted for 22 h.
The patient self-reported that recurrent chest pain had started 22 h prior to admission. He estimated that his symptoms had started approximately 20 min after he had eaten ice cream, and included slight dyspnea and palpitations experienced before admission.
Two years prior, the patient had presented to a local hospital with hypertension. He had no history of allergies.
The patient denied familial inherited diseases.
On admission, the patient had a blood pressure of 133/70 mmHg, a pulse of 75 bpm, an axillary temperature of 36.8 °C, and a respiratory rate of 19/min. His central venous pressure was not elevated, and he had neither pulmonary crepitations nor peripheral edema. He had a mid-systolic, 2/6 murmur, loudest in the mitral valve area.
Blood tests revealed a serum troponin I level of 0.68 ng/mL (normal range: < 1.68 ng/mL) and creatine kinase isoenzyme level of 48 U/L (normal range: 0.00-25.00 U/L). Potassium was 3.72 mmol/L (normal range: 3.50-5.50 mmol/L), sodium was 139.8 mmol/L (normal range: 135.0-145.0 mmol/L), and glucose was 4.95 mmol/L (normal range: 3.90-6.10 mmol/L). C-reactive protein was 40 mg/L (normal range: 0.00-5.00 mg/L), antinuclear antibody titer was 1:100 (normal: 1:100), and eosinophils were 0.88 × 109/L (normal range: 0.02-0.52 × 109/L). The total serum IgE antibody concentration increased to 884.9 IU/mL (normal value: < 200 IU/mL).
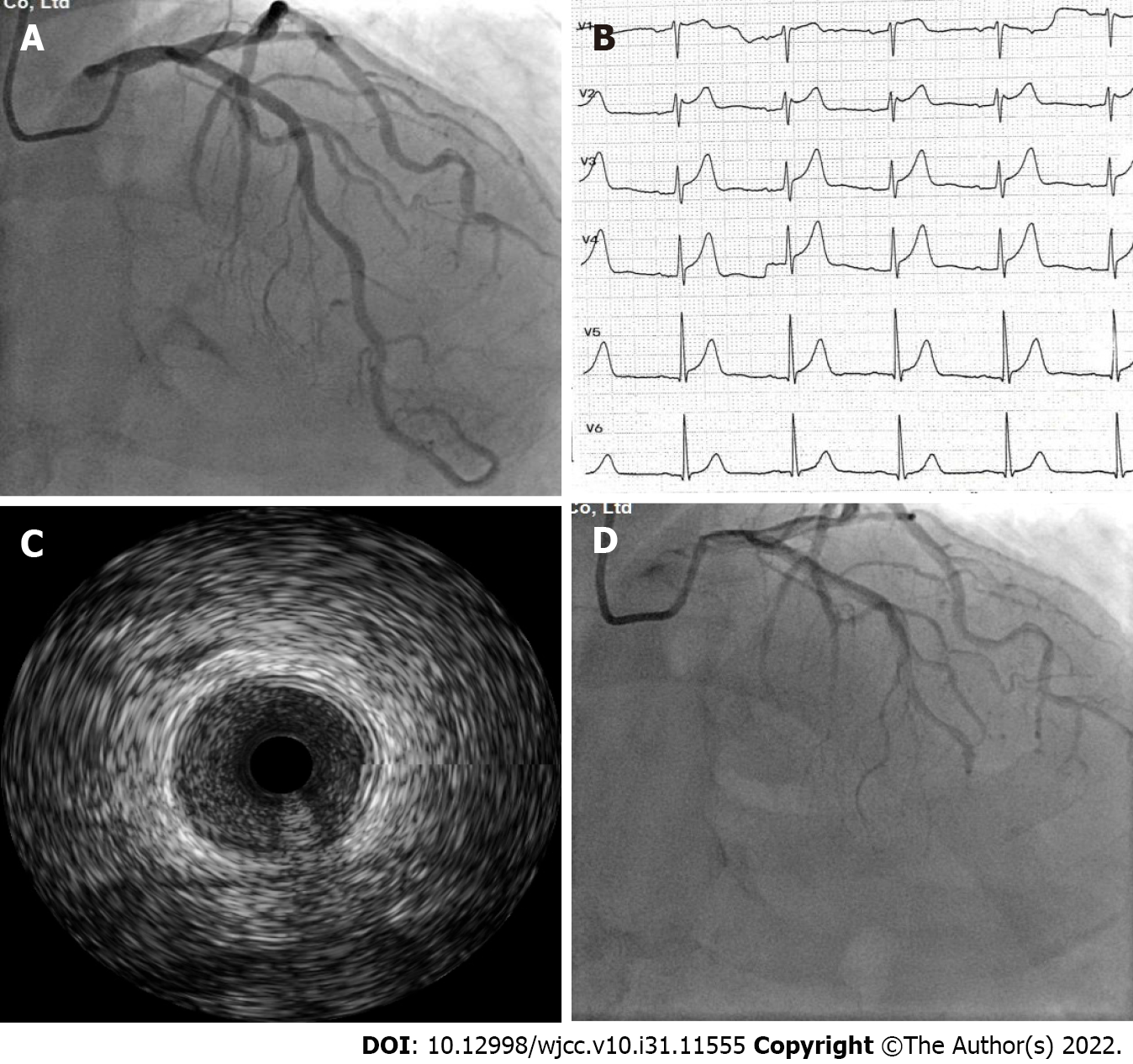
An electrocardiogram (ECG) on admission showed non-specific T wave changes. Echocardiography revealed normal left ventricular ejection fraction and a small amount of mitral regurgitation. Elective coronary angiography revealed that the left and right coronary arteries showed no significant stenosis and occlusion on the day of hospitalization (Figure 1A). However, the patient suddenly developed syncope on day 2 of hospitalization. We confirmed AMI with ECG and troponin I levels. ST-segment elevation was observed in V1-V4 Leads (Figure 1B) and high-sensitivity troponin I was elevated to 1.79 ng/mL (normal range: < 1.68 ng/mL). Emergent coronary angiography demonstrated acute occlusion of the left anterior descending artery (Figure 1C). However, blood flow returned to previous levels after 2 min of diltiazem administration. ECG changes were consistent with coronary artery spasms. Intravascular ultrasound (IVUS) showed that the occlusion of the left anterior descending artery was normal, with no plaque or dissection (Figure 1D). Microvascular coronary artery disease was not detected by the index of microcirculatory resistance. There was no evidence of atherosclerotic coronary artery disease on coronary artery angiogram.
The patient was diagnosed with vasospastic myocardial infarction due to Kounis syndrome. We presumed that Kounis syndrome was caused by chemical additives in ice cream because there was no exposure to other suspected allergic substances and no medications other than antihypertensive medications were taken.
The patient was treated with routine care to prevent coronary artery disease. His medications included 75 mg clopidogrel bisulfate, 5 mg benazepril, 5 mg felodipine, 120 mg isosorbide mononitrate and 20 mg atorvastatin. After the second coronary angiography, we added hydrocortisone and intravenous antihistamines.
With the addition of glucocorticoids and antihistamines, the patient’s chest pain symptoms resolved. After 2 wk, glucocorticoids and clopidogrel bisulfate were discontinued. The patient had good tolerance and compliance, and no adverse effects occurred with the current medications of benazepril, felodipine, isosorbide mononitrate, atorvastatin and loratadine. The patient’s ECG returned to normal after 4 wk, with non-specific T wave changes in V1-V4 Leads.
We report a novel ice cream allergic reaction-induced coronary artery spasm leading to AMI[2]. The patient had no evidence of atherosclerotic coronary artery disease on coronary angiogram. To the best of our knowledge, most cases of acute coronary syndrome result from coronary atherosclerotic plaque erosion or rupture followed by thrombus formation[3]. Allergic reactions can also induce acute coronary syndrome, including coronary artery vasospastic angina, plaque rupture and drug-eluting coronary stent thrombosis. This phenomenon is called Kounis syndrome[4]. The prevalence of Kounis syndrome among patients hospitalized for allergic reactions in the United States was estimated to be 1.1%[5]. Abdelghany et al[6] established a categorization system for the syndrome as types I–III. In this case, the patient had normal coronary arteries and persistent coronary spasms, leading to AMI, elevated cardiac enzyme levels, and ECG-detected ST-segment elevation, thus indicating type I Kounis syndrome.
The clinical presentation of Kounis syndrome is cardiac symptomatology and allergic reaction[7]. In our case, the patient’s initial symptoms were chest pain followed by dyspnea, palpitations and finally syncope. The ECG changes and abnormality of troponin I were delayed by 1 d. A characteristic feature of this case was an allergic reaction with delayed AMI. Food, medications, some conditions and environmental exposures[8] can trigger Kounis syndrome, regardless of the presence of coronary atherosclerosis (Table 1). All drugs and foods have the potential to be allergens. This patient had consumed ice cream, which may have had chemicals that activated an allergic reaction. From our investigation, we found no other reported cases of ice cream-induced Kounis syndrome.
| Food | Drugs | Conditions | Environmental exposure |
| Shellfish | Antibiotics | Stents | Hymenoptera stings |
| Fish | NSAIDs | Skin itching | Jellyfish stings |
| Mushroom | Antineoplastics | Bronchial asthma | Viper venom |
| Fruits | Analgesics | Mastocytosis | Scorpion stings |
| Canned food | Thrombolytics | Serum sickness | Latex |
| Anticoagulants |
The significantly elevated circulating eosinophils and serum IgE antibody levels in this patient suggested a potential relationship between the allergic reaction from frozen food and AMI. Mast cell degranulation is implicated in Kounis syndrome. This is mediated by the release of inflammatory mediators including histamine, leukotrienes, thromboxane and neutral proteases such as tryptase, chymase and cathepsin D[7]. These inflammatory mediators have critical cardiovascular activity. The medial muscle cells of the coronary arteries are affected by these inflammatory mediators. They induce local coronary artery spasm, plaque rupture or in-stent restenosis[8], which could progress to acute myocardial damage or coronary thrombosis[7]. These outcome events can initiate an acute coronary event.
There are no reports assessing Kounis syndrome diagnosed using IVUS or optical coherence tomography (OCT). We suggest that patients suspected of having Kounis syndrome undergo coronary arteriography and IVUS or OCT. Of note, however, blind implantation of coronary stents without IVUS and OCT can cause pain and other problems. Measurement of serum histamine, tryptase, cardiac enzymes and troponin I are critical for diagnosis. Blood samples should be collected immediately after the onset of the chest pain and before any drug administration. However, in this case these tests were not performed in a timely fashion due to the patient’s variable manifestations and the physician’s lack of awareness.
There are no consensus guidelines for treating Kounis syndrome; however, all emphasize immediate cessation of medications, foods and environmental exposures to prevent further heart damage[9,10]. Medications administered to treat cardiac manifestations can worsen the allergic reaction, and medications given for allergic reactions can aggravate cardiac dysfunction[2]. We believe the treatment of Kounis syndrome should consider allergic reactions and coronary artery revascularization[11]. In type I Kounis syndrome, treatment includes antihistamines, glucocorticoids and vasodilators. The treatment of types II and III should be based on acute coronary syndrome guidelines with allergic reaction management[7].
Ice cream additives, including artificial flavors, artificial colors and preservatives, may induce Kounis syndrome, which can cause serious damage to the heart. Coronary angiography and IVUS or OCT can help physicians to differentially diagnose Kounis syndrome and avoid misdiagnosis. Measurement of serum histamine, tryptase, cardiac enzymes and troponin I are critical for accurate diagnosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Abubakar MS, Nigeria; Gupta P, United States; Ozden F, Turkey S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Weresa J, Pędzińska-Betiuk A, Mińczuk K, Malinowska B, Schlicker E. Why Do Marijuana and Synthetic Cannabimimetics Induce Acute Myocardial Infarction in Healthy Young People? Cells. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 2. | Abdelghany M, Subedi R, Shah S, Kozman H. Kounis syndrome: A review article on epidemiology, diagnostic findings, management and complications of allergic acute coronary syndrome. Int J Cardiol. 2017;232:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 179] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 3. | Falk E, Nakano M, Bentzon JF, Finn AV, Virmani R. Update on acute coronary syndromes: the pathologists' view. Eur Heart J. 2013;34:719-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 676] [Cited by in RCA: 732] [Article Influence: 56.3] [Reference Citation Analysis (0)] |
| 4. | Kounis NG. Coronary hypersensitivity disorder: the Kounis syndrome. Clin Ther. 2013;35:563-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 220] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 5. | Desai R, Parekh T, Patel U, Fong HK, Samani S, Patel C, Savani S, Doshi R, Kumar G, Sachdeva R. Epidemiology of acute coronary syndrome co-existent with allergic/hypersensitivity/anaphylactic reactions (Kounis syndrome) in the United States: A nationwide inpatient analysis. Int J Cardiol. 2019;292:35-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 6. | Abdelghany M, Shah S, Subedi R, Kozman H. New classification of Kounis Syndrome. Int J Cardiol. 2017;247:14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Kounis NG. Kounis syndrome: an update on epidemiology, pathogenesis, diagnosis and therapeutic management. Clin Chem Lab Med. 2016;54:1545-1559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 180] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 8. | Nakajima Y, Itoh T, Morino Y. Metal allergy to everolimus-eluting cobalt chromium stents confirmed by positive skin testing as a cause of recurrent multivessel in-stent restenosis. Catheter Cardiovasc Interv. 2016;87:E137-E142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Martinez E, Sahni S, Cheema MA, Iftikhar A. Vancomycin-induced coronary artery spasm: a case of Kounis syndrome. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Leibee C, Getachew B, Ehmann MR. Vancomycin-induced Kounis Syndrome. Am J Emerg Med. 2019;37:1806.e3-1806.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Brown SG. Cardiovascular aspects of anaphylaxis: implications for treatment and diagnosis. Curr Opin Allergy Clin Immunol. 2005;5:359-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 123] [Article Influence: 6.2] [Reference Citation Analysis (0)] |