Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11517
Peer-review started: May 19, 2022
First decision: August 4, 2022
Revised: August 14, 2022
Accepted: August 30, 2022
Article in press: August 30, 2022
Published online: November 6, 2022
Processing time: 160 Days and 19 Hours
Heavy eye syndrome (HES) is an acquired strabismus typically seen in eyes with high myopia. We report a classic case in which a patient was misdiagnosed with esotropia and underwent disinsertion of the medial rectus muscle and lateral rectus muscle resection procedures.
A 71-year-old woman presented with both eyes fixed in adduction and infraduction for 33 years. She had undergone three complicated strabismus surgeries to amputate the left medial rectus (MR) muscle with lateral rectus mus
The Yokoyama procedure was effective in correcting HES.
Core Tip: In highly myopic patients, excessively long axial length can cause a type of myopia-induced strabismus, characterized by progressive esotropia and hypotropia, which means the enlarged globe displace between the superior rectus and lateral rectus muscles. In this case report, a woman had been misdiagnosed with simple esotropia and had undergone three recession-resection surgeries with no improvement. We performed a Yokoyama procedure, and her eyes remained binocularly aligned for 6 mo postoperatively.
- Citation: Yao Z, Jiang WL, Yang X. Yokoyama procedure for a woman with heavy eye syndrome who underwent multiple recession-resection operations: A case report. World J Clin Cases 2022; 10(31): 11517-11522
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11517.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11517
Heavy eye syndrome (HES) is a type of myopia-induced strabismus, characterized by progressive esotropia and hypotropia associated with limited elevation and abduction[1]. The possible pathological mechanism of HES is described as enlarged globe herniation through the superotemporal muscle cone, which can be analyzed and proven through orbital imaging[2]. Although HES has been known for a half century, some HES patients are still not being treated appropriately due to inaccurate diagnosis[3]. In this case report, a 71-year-old woman presented with large esotropia with hypotropia, which had been misdiagnosed as simply esotropia, and she had undergone three recession-resection surgeries with no improvement. We performed a Yokoyama procedure, and her eyes remained binocularly aligned for 6 mo postoperatively.
A 71-year-old woman presented with a 33-year history of fixed adduction and infraduction in both eyes.
Esotropia fixus set in progressively during middle age. She had been diagnosed with esotropia 17 years earlier and had undergone three previous complicated strabismus surgeries: amputation of the left medial rectus (MR) muscle 17 years ago, amputation of the left MR with lateral rectus (LR) muscle recession (10 mm) 15 years ago, and amputation of the left MR muscle with LR muscle recession 13 years ago. However, after each surgery, the esotropia did not improve.
The patient suffered from high myopia for 60 years before the cataract surgery on her right eye 18 years ago. She has had hypertension for 40 years, coronary heart disease for 21 years and autoimmune hepatitis for 6 mo. She had a cesarean section 44 years ago and a stent placed in her left renal artery 19 years ago. She was allergic to sulfonamides and nitroglycerin for unknown periods of time.
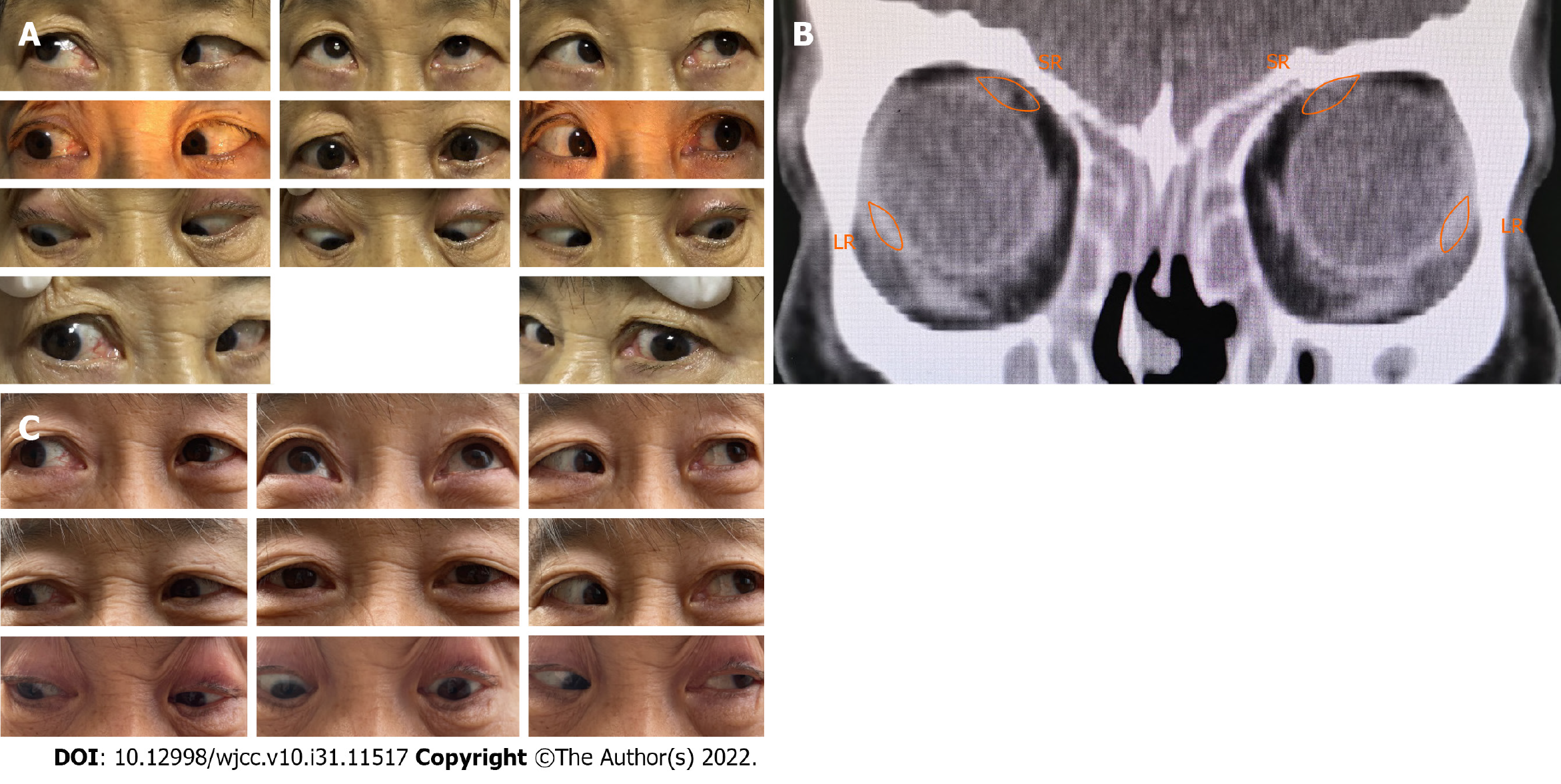
The younger sister of the woman, who was 63 years old, had an 18-year history of progressive fixed adduction in both eyes. She also had high myopia in both eyes in childhood. Her best-corrected visual acuity (BCVA) was 1.0 in the right eye and 0.6 in the left eye; the right eye was her dominant eye. She had primary position esotropia of 95∆ at both near and distance as determined by prism and alternating cover test. Both abductions were restricted (Figure 1A). The axial lengths were 28.36 mm in the right eye and 29.28 mm in the left eye. Orbital computed tomography (CT) revealed an axially enlarged globe associated with obvious nasal displacement of the superior rectus (SR) muscle (Figure 1B). She was also diagnosed with HES and underwent the Yokoyama procedure in her left eye and recession of the left MR muscle (5 mm) under general anesthesia. The forced duction test (FDT) was positive for abduction in her left eye. The patient had binocular alignment on follow-up at 6 mo with obviously improved abduction in the left eye (Figure 1C).
The patient’s temperature was 36 °C, heart rate 95 bpm, respiratory rate 20 breaths/min, and blood pressure 150/83 mmHg.
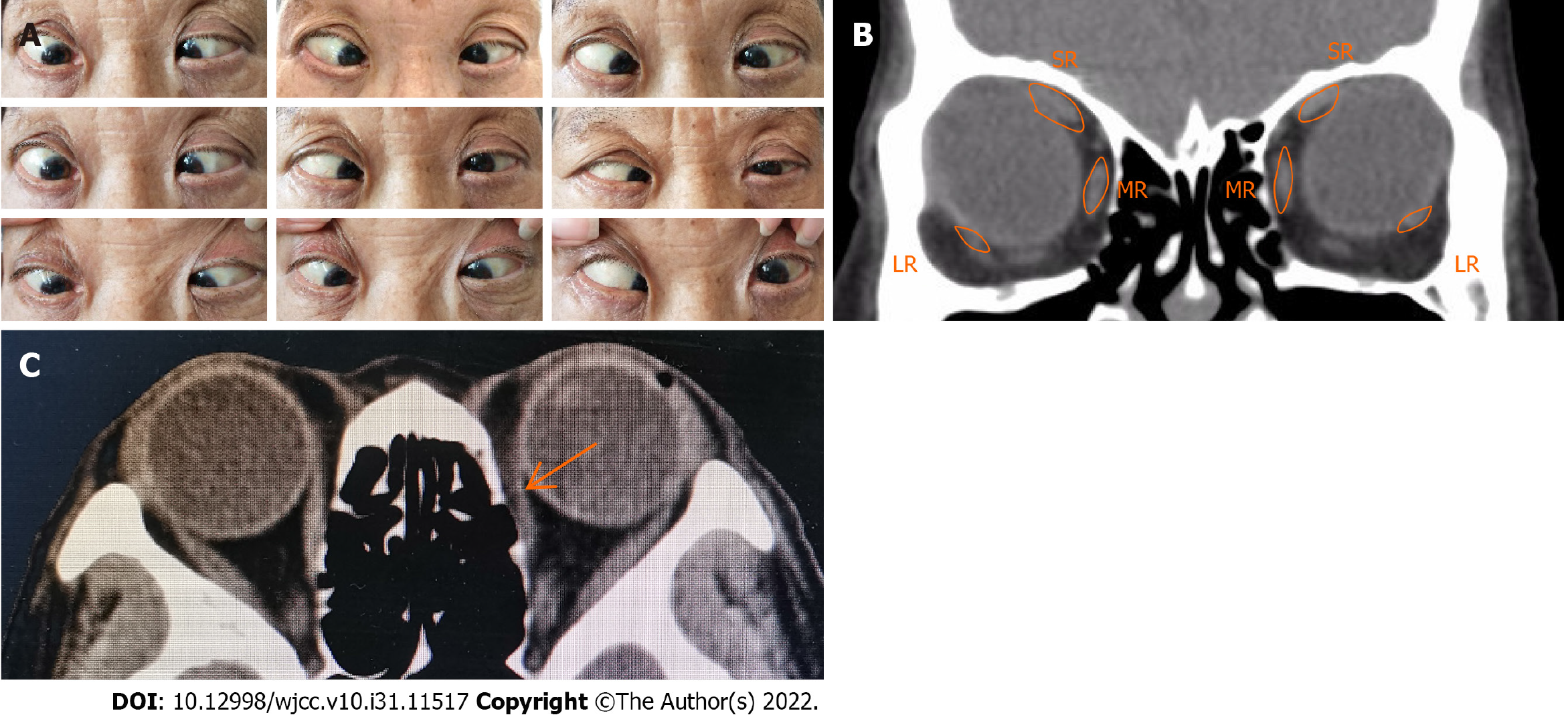
Her BCVA was 0.2 in the right eye and HM/30 cm in the left eye. Her refraction before cataract surgery was about - 10.0 D cycle in both eyes. She had approximately 40° esotropia and 15° hypotropia in the left eye with right eye fixation and 30° esotropia and 15° hypotropia in the right eye with left eye fixation in the primary position by Krimsky test. Both abduction and elevation were restricted, so she was not able to bring her eyes to midline (Figure 2A). As the right eye was her dominant eye, she turned her face to the right.
Serum bilirubin was increased at 25.35 μmol/L, (normal range 3-22 μmol/L).
Ultrasonography showed the axial lengths were 27.19 mm in the right and 26.9 mm in the left eye with obvious posterior scleral staphyloma in both eyes. Orbital CT scan revealed an axially enlarged globe associated with inferior displacement of the LR muscle and nasal displacement of the SR muscle (Figure 2B). There was suspected reattachment of the left MR muscle to the globe (Figure 2C), which was scar adhesion that was confirmed intraoperatively.
The final diagnosis of the present case was HES.
With the patient’s consent, she underwent the Yokoyama procedure under general anesthesia. The FDT was positive for abduction and mildly positive for elevation in both eyes, meaning the eyes could not be easily brought even to midline. The right MR muscle was backward to 7 mm from the original insertion site as in a routine rectus muscle resection. The junctions between the 1/2 muscle bellies of the SR and LR muscles were made approximately 14 mm and 12 mm behind the insertions, respectively, using a nonabsorbable 5/0 suture (Yokoyama procedure). The intranasal bulbar conjunctiva retropulsion was fixed at 3 mm behind the limbus cornea. For the left eye, the incisions were along the original scar, and there was extensive subconjunctival scar adhesion without clear MR muscle structure. After separating the adhesion and excising scar tissue, the intranasal bulbar conjunctiva retropulsion was fixed at 3 mm behind the limbus cornea. The junctions between the SR and LR muscles were made approximately 12 mm and 10 mm behind the insertions, respectively, using the same approach as in the right eye.
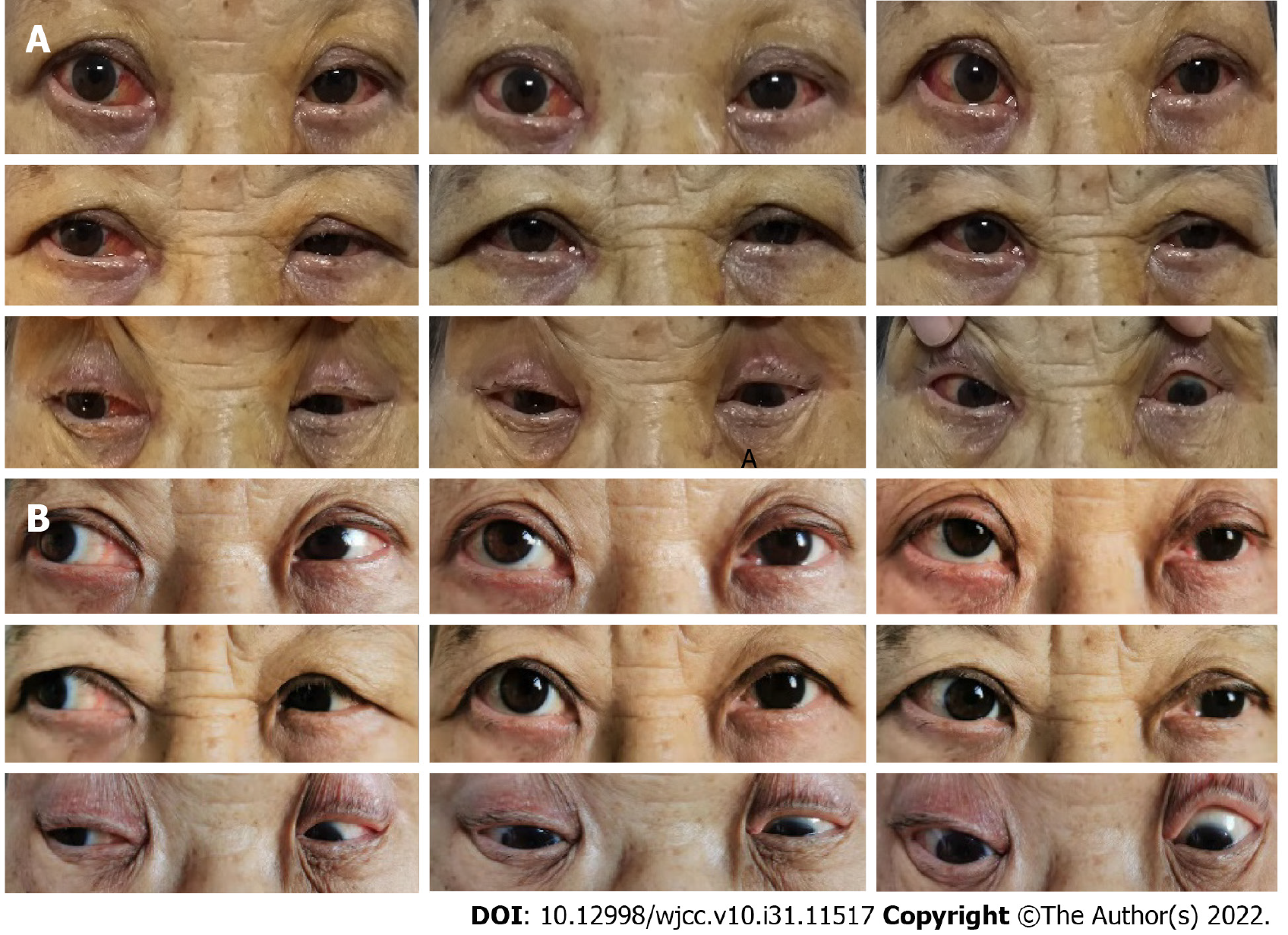
Postoperatively, the patient had a 5-10° exotropia of the left eye (Figure 3A), and the adduction improved from before the operation. The patient had binocular alignment with little exotropia on follow-up at 2 mo, and after 6 mo, her eyes remained binocularly aligned with almost normal abduction in the right eye (Figure 3B).
We reported a classic case in which a patient was misdiagnosed with esotropia and underwent the disinsertion of the MR and LR muscle resection procedures. Hayashi et al[4] have reported that the traditional recession and resection surgery could be effective in the early stages of HES without severe limitation of abduction. In this case, we found that this surgery had not improved the patient’s symptoms at all.
Instead of disorder of the extraocular muscle, the enlarged globe herniation through the superotemporal muscle cone is considered to be the possible pathological mechanism of HES[2]. To restore the herniated globe back into the muscle cone, Yokoyama et al[5] proposed a surgical procedure by uniting the muscle bellies of the SR and LR muscles, which has proven to be effective for highly myopic strabismus. Thus, a sufficient understanding of the pathophysiology of HES allows for an appropriate procedure plan.
Recession or amputation of the MR muscle and resection of the LR muscle often have limited effect in severe high myopia strabismus, and there is susceptibility to postoperative recurrence[6]. The shifts of the LR and SR muscles and the herniated globe may be the main cause of the failure and recurrence; other causes, such as the stretched scar associated with the limitation of ocular duction, were observed during this operation[7]. In addition, reattachment of the severed MR muscle to the globe might contribute to the recurrence of esotropia[8]. However, according to the patient descriptions, the tradi
This case highlights the importance of the pathological mechanism and diagnosis of HES in the esotropia of high myopia. Pertinacious esotropia combined with high myopia should be considered in HES. Orbital imaging and ultrasonography can demonstrate anatomical abnormality and muscle paths to confirm the definite diagnosis. The Yokoyama procedure is effective in correcting this strabismus.
In highly myopic patients, excessively long axial length can cause the enlarged globe to displace between the SR and LR muscles. Orbital imaging and ultrasonography can demonstrate anatomical abnormality and muscle paths to confirm a definite diagnosis. An effective option is join of the superior rectus muscle and lateral rectus muscles, usually with a nonabsorbable suture (Yokoyama procedure).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ghimire R, Nepal; Mohapatra SSD, India S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Hennein L, Robbins SL. Heavy eye syndrome: Myopia-induced strabismus. Surv Ophthalmol. 2021;66:138-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Maiolo C, Fresina M, Campos EC. Role of magnetic resonance imaging in heavy eye syndrome. Eye (Lond). 2017;31:1163-1167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Ward DM. The heavy eye phenomenon. Trans Ophthalmol Soc U K (1962). 1967;87:717-726. [PubMed] |
| 4. | Hayashi T, Iwashige H, Maruo T. Clinical features and surgery for acquired progressive esotropia associated with severe myopia. Acta Ophthalmol Scand. 1999;77:66-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Yamaguchi M, Yokoyama T, Shiraki K. Surgical procedure for correcting globe dislocation in highly myopic strabismus. Am J Ophthalmol. 2010;149:341-346.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 85] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Wei Y, Kang X. Surgical treatment progress of myopic strabismus fixus by Yokoyama's surgery. Zhonghua Yanke Zazhi. 2014;50:547-549. [PubMed] |
| 7. | Farid MF, Mahmoud MR, Awwad MA. Management of stretched scar- induced secondary strabismus. BMC Ophthalmol. 2020;20:58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Akbari MR, Alhashemi LH, Jafari AK, Eshraghi B, Fakhraie G. Large angle esotropia with high myopia and a lost medial rectus muscle: a case report. Binocul Vis Strabolog Q Simms Romano. 2013;28:110-114. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |