Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11454
Peer-review started: April 25, 2022
First decision: June 27, 2022
Revised: July 19, 2022
Accepted: October 9, 2022
Article in press: October 9, 2022
Published online: November 6, 2022
Processing time: 184 Days and 12.3 Hours
Controversy remains around the available choices for the internal fixation of a femoral neck fracture. The femoral neck system (FNS) was developed in 2018 and has been widely applied since then as it can provide rigid fixation stability with less damage to the bone mass around the fracture. However, no systematic reviews and meta-analyses have investigated the efficacy of the FNS in comparison with that of traditional internal fixation in the treatment of femoral fractures.
To assess the efficacy of the FNS in comparison with that of cannulated compression screws (CCS) in the treatment of femoral fractures through systematic review and meta-analysis.
Five electronic databases (PubMed, Embase, Cochrane Central Register of Controlled Trials, China National Knowledge Infrastructure, and Wanfang) were searched from the earliest publication date to December 31, 2021. Reference Citation Analysis (https://www.referencecitationanalysis.com/) was used to check the results and further analyze the related articles. Controlled trials were included if the FNS was applied for the femoral neck fracture in adults and if it was compared with CCS for the achievement of internal fixation. The measurement outcomes included the required operation time, observed patient’s blood loss, extent of fracture healing, patient’s Harris Hip score (HHS) at the last follow-up, and records of any complications (such as failure of internal fixation, femoral neck shortness, avascular necrosis of the femoral head, and delayed union or nonunion).
Ten retrospective controlled studies (involving 711 participants) were included in this meta-analysis. The meta-analysis showed that compared with CCS, use of the FNS could not decrease the operation time [standardized mean difference (SMD): -0.38, 95% confidence interval (CI): -0.98 to 0.22, P = 0.21, I2 = 93%), but it could increase the intraoperative blood loss (SMD: 0.59, 95%CI: 0.15 to 1.03, P = 0.009, I2 = 81%). The pooled results also showed that compared with CCS, the FNS could better promote fracture healing (SMD: -0.97, 95%CI: -1.65 to -0.30, P = 0.005, I2 = 91%), improve the HHS at the last follow-up (SMD: 0.76, 95%CI: 0.31 to 1.21, P = 0.0009, I2 = 84%), and reduce the chances of developing femoral neck shortness (OR: 0.29, 95%CI: 0.14 to 0.61, P = 0.001, I2 = 0%) and delayed union or nonunion (OR: 0.47, 95%CI: 0.30 to 0.73, P = 0.001; I2 = 0%) in adult patients with femoral neck fractures. However, there was no statistically significant difference between the FNS and CCS in terms of failure of internal fixation (OR: 0.49, 95%CI: 0.23 to 1.06, P = 0.07, I2 = 0%) and avascular necrosis of the femoral head (OR: 0.46, 95%CI: 0.20 to 1.10, P = 0.08, I2 = 0%).
Compared with CCS, the FNS could decrease the chances of developing femoral neck shortness and delayed union or nonunion in adults with femoral neck fractures. Simultaneously, it could accelerate fracture healing and improve the HHS in these patients.
Core Tip: This study aimed to investigate the efficacy of the femoral neck system (FNS) in comparison with cannulated compression screws (CCS) in the treatment of femoral neck fractures in adults. A total of 10 studies involving 711 participants were included. This study revealed that compared with CCS, the FNS could decrease the chances of developing short femoral neck and delayed union or nonunion as well as accelerate fracture healing and improve the Harris Hip score at the last follow-up in adult patients with femoral neck fractures. These results could help in the selection of the most appropriate treatment for patients with femoral neck fractures.
- Citation: Wu ZF, Luo ZH, Hu LC, Luo YW. Efficacy of the femoral neck system in femoral neck fracture treatment in adults: A systematic review and meta-analysis. World J Clin Cases 2022; 10(31): 11454-11465
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11454.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11454
Femoral neck fracture is one of the most common traumatic injuries, and it is believed to occur in 150000 patients per year in the United States (US) alone[1]. The incidence of this type of injury is increasing among elderly patients, and it is expected to exceed 250000 cases per year in the next 25 years, thereby accounting for approximately 50% of hip fracture cases in the US[2,3]. A femoral neck fracture can seriously affect the patient’s quality of life and increase the risk of severe complications[4].
Patients with femoral neck fractures tend to be treated surgically. Most elderly patients with displaced femoral fractures receive the golden standard treatment involving hemiarthroplasty or total hip arthroplasty[5]. However, there remains controversy regarding the choice of treatment for nondisplaced femoral neck fractures in the elderly and younger adult patients. Recent studies have demonstrated that the issues associated with existing internal fixation methods, such as the lack of an antirotation force, nail back, and loosening, can have a negative impact on the offset of femoral neck fractures, which may ultimately necessitate reoperation[6,7]. Several commonly used implants for establishing internal fixation in the femoral neck fracture include cannulate screws, dynamic hip screws, compression locking plates, and other newer plate systems.
In recent years, the femoral neck system (FNS; DePuy-Synthes, Johnson & Johnson Medical Devices, New Brunswick, NJ, United States) has been developed for the treatment of femoral neck fractures. The FNS requires minimal invasion and exerts antirotation, antisliding, and antishearing forces. However, there is insufficient evidence on the efficacy of the FNS in the treatment of femoral fractures when compared with traditional internal fixation methods. The aim of this study was to provide a systematic review of the literature in order to examine the efficacy of the FNS in the treatment of femoral neck fractures in adults.
Five electronic databases (PubMed, Embase, Cochrane Central Register of Controlled Trials, China National Knowledge Infrastructure, and Wanfang) were searched from the earliest publication date to December 31, 2021. The PubMed search strategy was as follows: (((((femoral neck fracture[Title/Ab
Inclusion criteria: A study was included if: (1) It was a randomized controlled trial (RCT) or a controlled clinical trial; (2) It discussed patients aged > 18 years with femoral neck fractures; (3) The patients were treated with internal fixation; (4) There was a comparison between the FNS and cannulated compression screws (CCS); and (5) It was available as a full-text article.
Exclusion criteria: A study was excluded if: (1) The patients did not suffer from a femoral neck fracture; (2) It was not a clinical study (e.g., basic research articles, review articles, case reports, etc.); (3) The patients suffered from pathological fractures and necrosis of the femoral head; (4) The control group did not refer to patients treated with CCS; and (5) The statistical methodologies used were inappropriate.
Data extraction from the included studies was independently undertaken by two authors. Data included the first author’s name, publication year, patient sample size, patients’ age, intervention group characteristics, control group characteristics, follow-up time, test type, outcome measurements, and fracture types. The outcome measurements included operation time, intraoperative blood loss, fracture healing time, hip function outcomes, and recorded complications. The failure of internal fixation of complications was defined by incidents involving screw loosening, back-offs, and penetration.
The methodological quality of the included studies was independently assessed by two authors. The quality of each nonrandomized controlled study was assessed according to the methodological index for nonrandomized studies (MINORS) entry based on the MINORS scores: Studies with scores of > 12 were included[8]. The quality of each RCT was assessed by using the Cochrane Collaboration tool based on the following factors: random sequence generation, allocation concealment, participant and personnel blinding, outcome assessment blinding, incomplete outcome data, selective reporting, and other biases. Any dispute between the two authors was resolved via mutual discussion or with the assistance of the third author.
Both the meta-analysis and statistical analysis were performed using RevMan version 5.3 (Cochrane London, United Kingdom). Odds ratio (OR) and 95% confidence interval (CI) were used for dichotomous data analyses. Continuous data were presented as mean difference (MD) or standardized MD (SMD) and 95%CI. The Cochrane I2 test was used for assessing heterogeneity among the analyzed studies. Quartile data were converted into median and deviation with the use of an online resource (https://www.math.hkbu.edu.hk/); if the data skewed away from normality, they were subsequently excluded from the meta-analysis[9,10]. A random-effects model was applied if I2 was > 50%; otherwise, a fixed-effects model was applied. A P value of < 0.05 was considered to indicate statistical significance. This study was a systematic review and meta-analysis and did not require ethical approval. All data were obtained from published papers.
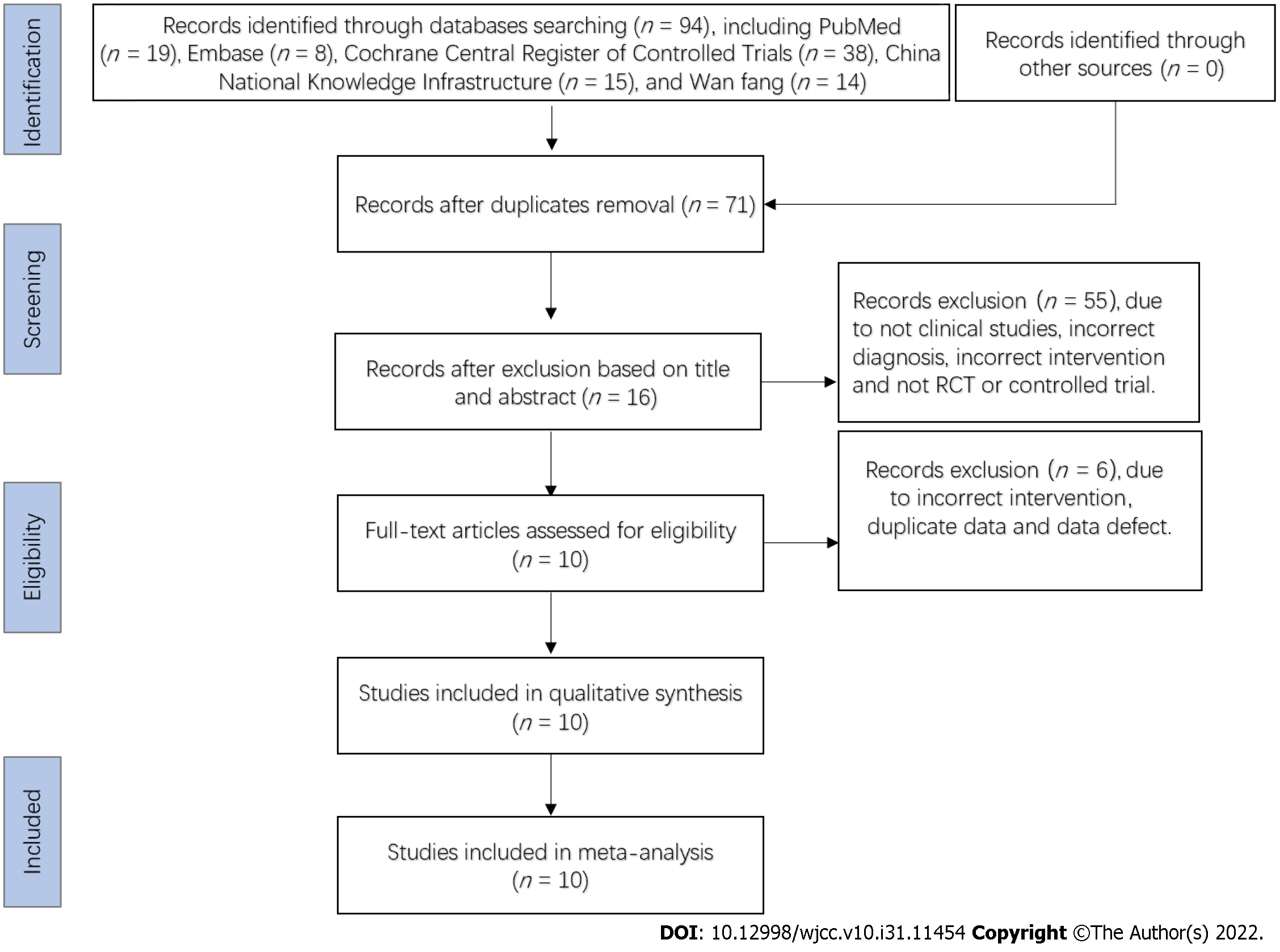
A total of 94 studies were initially identified from the search of the aforementioned 5 electronic databases. After eliminating duplicates, the titles and abstracts of 71 relevant studies were screened. Of these, 61 studies were excluded for various reasons (e.g., studies referring to nonclinical trials, studies that were not RCTs or controlled trials, studies including a different diagnosis, studies using a different intervention, studies presenting duplicate data, and studies characterized by data defects). Based on their full text, 10 studies[11-20] conformed to the set inclusion criteria. The literature search procedure followed herein is illustrated in Figure 1.
As shown in Table 1, the included studies were 10 retrospective controlled studies with a total of 711 participants. All of these studies compared use of the FNS with the use of CCS. Other detailed characteristics of these studies are presented in Table 1.
| Complications | A; B; C; D; E | A; B; C; F; G | A; B; D; E | A; B; E | B; I | |
| Outcomes | Operation time; intraoperative blood loss; fracture healing time; HHS at the last follow-up | Operation time; intraoperative blood loss; fracture healing time; HHS at the last follow-up | Operation time; intraoperative blood loss; fracture healing time; HHS at the last follow-up | Operation time; intraoperative blood loss; fracture healing time; HHS at the last follow-up | Operation time; intraoperative blood loss; fracture healing time; HHS at the last follow-up | |
| Type of fracture | Garden II/III/IV | Pauwels I/II/III | Garden II/III/IV | Garden II/III/IV | Garden I/II/III/IV | |
| Study type | Retrospective study | Retrospective study | Retrospective study | Retrospective study | Retrospective study | |
| Follow-up time | ≥ 6 mo | 5-18 mo | ≥ 12 mo | 3-18 mo | Unknown | |
| G2 | CCS | CCS | CCS | CCS | CCS | |
| G1 | FNS | FNS | FNS | FNS | FNS | |
| Participants | G2 | 38, 48.8 ± 10.1 | 47, 43.7 ± 13.1 | 57, 53.2 ± 11.3 | 58, 49 | 19, 41.2 |
| (n, age: mean ± SD) | G1 | 32, 49.4 ± 11.0 | 47, 47.8 ± 9.8 | 62, 54.0 ± 13.0 | 24, 52 | 15, 42.0 |
| First author, year | Ren C (2021) [11] | Yang J (2021) [12] | Xiong W (2021) [13] | Yan C (2021) [14] | Yang Y (2021) [15] | |
| Complications | A; B; E; H | A; D; E | B; E; H; I | A; B; E; D | B | |
| Outcomes | Operation time; intraoperative blood loss; fracture healing time; HHS at the last follow-up | Operation time; intraoperative blood loss; HHS at the last follow-up | Operation time; fracture healing time; HHS at the last follow-up | Operation time; intraoperative blood loss; fracture healing time; HHS at the last follow-up | Operation time | |
| Type of fracture | Pauwels I/II/III | Pauwels III | Garden I/II/III/IV | Pauwels I/II/III | Garden I/II | |
| Study type | Retrospective study | Retrospective study | Retrospective study | Retrospective study | Retrospective study | |
| Follow-up time | ≥ 6 mo | 10-22 mo | 12-24 mo | 14-24 mo | 3-6 mo | |
| G2 | CCS | CCS | CCS | CCS | CCS | |
| G1 | FNS | FNS | FNS | FNS | FNS | |
| Participants | G2 | 24, 50.46 ± 9.26 | 30, 53.14 ± 7.19 | 36, 47.58 ± 10.31 | 45, 54.8 ± 11.7 | 32, 85 ± 6.6 |
| (n, age: mean ± SD) | G1 | 20, 50.45 ± 8.45 | 30, 54.53 ± 6.71 | 33, 50.61 ± 10.30 | 47, 57.4 ± 15.0 | 15, 86.1 ± 4.6 |
| First author (year) | Hu H (2021) [16] | Zhou X (2021) [17] | He C (2021) [18] | Tang Y (2021) [19] | Vazquez O (2021) [20] | |
The RCTs’ risk of bias assessment was evaluated using the Cochrane Collaboration tool. The results showed that there were no RCTs among the included studies. For the retrospective controlled studies, MINORS was used to assess the methodological quality. The interval scores of these were 17-19 points. Among these studies, two scored 17 points, six scored 18 points, and two scored 19 points in the MINORS assessment. Thus, the current meta-analysis is characterized by methodological quality limitations.
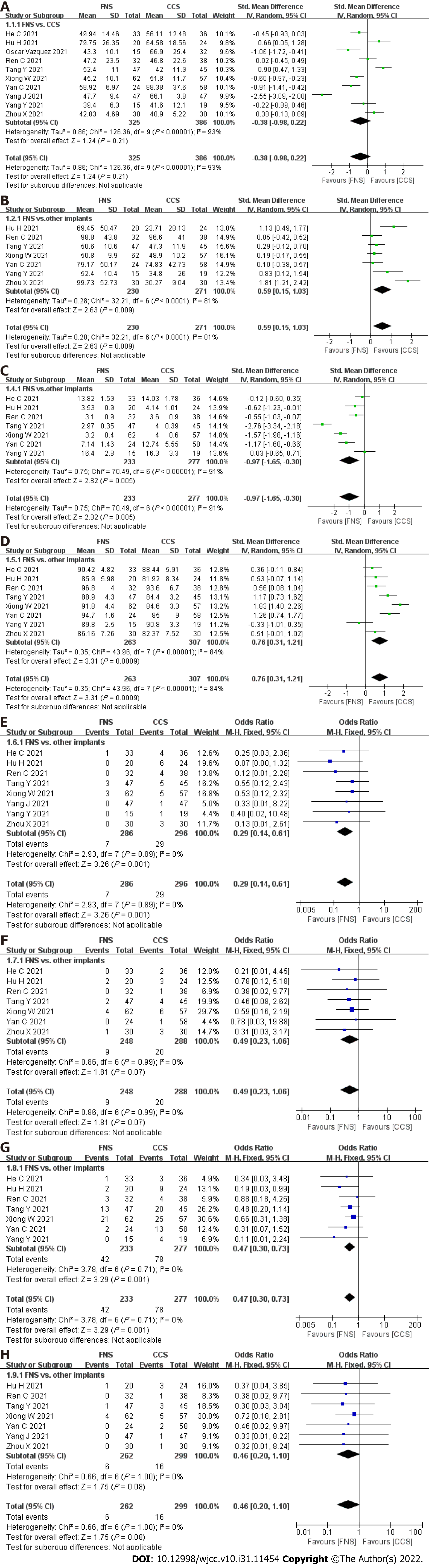
In the meta-analysis presented in Figure 2A, 10 articles were included to analyze the operation time required for the surgical treatment of femoral neck fractures. The pooled results of included articles showed that compared with CCS, the FNS could not decrease the required operation time (SMD: -0.38, 95%CI: -0.98 to 0.22, P = 0.21, I2 = 93%).
Seven studies reported blood loss, as presented in Figure 2B. The random-effects model was used due to the high level of heterogeneity observed (P < 0.001, I2 = 81%). The pooled results of these trials revealed that compared with CCS, the FNS could increase intraoperative blood loss (SMD: 0.59, 95%CI: 0.15 to 1.03, P = 0.009, I2 = 81%).
Among the studies included in this meta-analysis, seven studies, which included 510 participants, reported the fracture healing time (see Figure 2C). The random-effects model was used due to the high level of heterogeneity observed (P < 0.001, I2 = 91%). The pooled results of these trials revealed that compared with CCS, the FNS could shorten the fracture healing time (SMD: -0.97, 95%CI: -1.65 to -0.30, P = 0.005, I2 = 91%).
Eight studies were included in the analysis of the Harris Hip score (HHS) at the last follow-up (Figure 2D). The random-effects model was used due to the high level of heterogeneity observed (P < 0.001, I2 = 86%). The meta-analysis revealed that compared with CCS, the FNS could improve the HHS recorded at the last follow-up (SMD: 0.76, 95%CI: 0.31 to 1.21, P = 0.0009, I2 = 84%).
Eight studies were included in the analysis of femoral neck shortening (Figure 2E). The fixed-effects model was used due to the low level of heterogeneity observed (P = 0.89, I2 = 0%). The incidence of femoral neck shortening was lower after surgical treatment with the FNS than after surgical treatment with CCS (OR: 0.29, 95%CI: 0.14 to 0.61, P = 0.001, I2 = 0%).
Seven studies were included in the analysis of failure of internal fixation (Figure 2F). The fixed-effects model was used due to the low level of heterogeneity observed (P = 0.95, I2 = 0%). The included studies revealed that compared with CCS, the FNS could not reduce the incidence of the failure of internal fixation (OR: 0.49, 95%CI: 0.23 to 1.06, P = 0.07, I2 = 0%).
Seven studies were included in the meta-analysis of the occurrence of delayed union or nonunion (Figure 2G). The fixed-effects model was used due to the high level of heterogeneity observed (P = 0.71, I2 = 0%). Compared with CCS, the FNS reduced the incidence of delayed union or nonunion (OR: 0.47, 95%CI: 0.30 to 0.73, P = 0.001; I2 = 0%).
The development of avascular necrosis of the femoral head was reported in 7 studies, including 6 and 16 cases in the FNS and CCS groups, respectively (Figure 2H). No heterogeneity was observed (P = 1.00, I2 = 0%) and, as such, the fixed-effects model was used. The obtained results revealed that there was no statistically significant difference in terms of the incidence of avascular necrosis of the femoral head between the two studied groups (OR: 0.46, 95%CI: 0.20 to 1.10, P = 0.08, I2 = 0%).
Other complications were also analyzed in this meta-analysis, and the obtained results are summarized in Table 2.
| Complications | Number of cases (FNS/other implants) | OR (95%CI) | P | I2 (%) |
| Deep venous thrombosis | 3/5 | 0.64 (0.15, 2.78) | 0.55 | 0 |
| Thigh irritation | 0/15 | 0.02 (0.00, 0.38) | / | / |
With the increase in the aging population, femoral neck fractures are becoming increasingly common every year; they are typically treated via internal fixation surgery, which tends to have several complications, such as fracture nonunion, femoral neck avascular necrosis, femoral neck shortening, and hip deformity[21,22]. To date, no harmonized standards exist regarding the choice of the right internal fixation technique. The FNS, which has superior biomechanical characteristics, was introduced in China in 2018, but there is insufficient evidence of its efficacy in the treatment of femoral fractures compared with traditional internal fixation techniques, such as CCS[23]. Thus, this study aimed to assess the efficacy of the FNS in comparison with that of CCS in the treatment of femoral fractures through systematic review and meta-analysis.
We searched 5 databases and identified 10 retrospective controlled studies (with a total of 711 participants) that met the inclusion criteria. In this meta-analysis, we found that there was no significant difference in the operation time between the FNS and CCS. Although the FNS has been introduced recently, it features simple operation (short learning curve) and low-level trauma[18]. CCS requires better spatial distribution of three screws, which may warrant the repeated adjustment of guidewires and increase the number of intraoperative fluoroscopies[18]. These may be the reasons why both required similar operation times. However, the pooled results revealed that intraoperative blood loss was higher when using the FNS than when using CCS. It is possible that all patients treated with the FNS required open reduction, which could lead to surgical trauma with a small window of exposure. This may lead to similar operation times but more blood loss.
Our data indicated that the chances of femoral neck shortening were lower when using the FNS than when using CCS. CCS are widely used for internal fixation in patients with femoral neck fractures owing to the minimally invasive surgical procedure, low cost, and antirotation force[18]. However, recent research has reported poor biomechanical properties of CCS for unstable femoral neck fractures[24]. A biomechanical study suggested that the FNS is a reliable implant for femoral neck fractures as it has biomechanical characteristics similar to those of dynamic hip screws (DHS) as well as stability superior to that of CCS[23]. In addition, a finite element analysis showed that the FNS exerts a higher internal fixation stress than CCS, which is about 1.6-3.0 times that of CCS[25]. Taken together, the FNS (which is characterized by the angular stability constructs of its bolt, antirotation screws, a lateral plate, and locking screws), provides superior resistance against femoral neck shortening, and its sliding design of antirotation and locking screws allow the surgeon to achieve the maximum sliding compression of 20 mm during the operation[19]. Interestingly, the incidence of internal fixation failure for the FNS was the same as that for CCS. In this meta-analysis, fixation failure included screw loosening, back-off, penetration, etc. It is possible that the incidence of fixation failure associated with the FNS is actually lower due to fracture type, bone quality and reduction, and implant position. However, we may have observed similar incidences for the FNS and CCS due to factors such as small sample size and short follow-up time.
Previous studies showed that the nonunion rate of femoral neck fracture treated with CCS was higher than that of femoral neck fracture treated with angle-stabilized internal fixators[26,27]. Our study identified that compared with CCS, use of the FNS for treating femoral neck fractures could shorten the required fracture healing time as well as decrease the incidence of delayed union or nonunion. Time to surgery, fracture type, and bone reduction and quality may be the major determinants of bone healing. In addition, current evidence has shown that the stability of the femoral neck fracture is also crucial for promoting bone healing[28,29]. In general, the mechanical stability of a fractured bone osteosynthesis is composed of the stability of the internal implant and the stability of the bone. The FNS meets the demand of stability of the implant in the osteosynthesis of bone fracture and conserves less strength at the femoral head than that of intact bone after bone healing[30,31]. It is thought that the FNS accelerated the healing of the fracture and reduced the incidence of delayed union or nonunion owing to the stability of the osteosynthesis construct in the fracture gap. The pooled results showed that compared with CCS, use of the FNS for treating femoral neck fractures could improve the HHS at the last follow-up. Previous studies have reported that femoral neck shortening can decrease hip function, especially in severe cases[26,32,33]. The FNS decreases the incidence of femoral neck shortening, and patients treated with the FNS could perform the timely postoperative weight-bearing activities[18]. Although the HHS was higher in the FNS group, no difference between the FNS and CCS groups was observed for the incidence of femoral head avascular necrosis in this meta-analysis. Apart from factors such as fracture type, stability, and bone reduction and quality, it is reported that the large volume of the implant could damage the blood vessels of the femoral head[34]. As far as the design of the FNS is concerned, the diameters of the screw bolt and antirotation screws were 6.4 mm and 10 mm, respectively. Therefore, similar to CCS, the FNS could also preserve the peripheral vessels in the femoral head.
This meta-analysis has several limitations. First, all the included studies were classified as retrospective controlled studies with MINORS scores between 17 and 19; hence, there is a high risk of bias and methodological quality limitations in these studies. Second, the overall sample size of the analyzed studies was small. Third, the follow-up time in most of the included studies was short. Fourth, fracture type, reduction quality, implant position, patient age, and time from injury to surgery were important factors in gaining good results in this meta-analysis; however, these could not be analyzed as the included studies did not describe these data specifically. Finally, “control” referred to only CCS; as a result, this study does not provide a definite conclusion on whether the FNS is a superior internal fixation method for the surgical treatment of femoral neck fractures compared with other implants (apart from CCS).
The results of this meta-analysis could help in the selection of the most appropriate treatment for patients with femoral neck fractures. However, considering the high risk of biases and poor methodological quality of the studies included in this meta-analysis, further studies (preferably RCTs) are required to draw more reliable conclusions on the efficacy of the FNS in the treatment of femoral neck fractures in adult patients.
This meta-analysis showed that compared with CCS, the FNS cannot shorten the operation time but increases intraoperative blood loss. The pooled results also revealed that compared with CCS, the FNS can better promote fracture healing, improve the HHS at the last follow-up, and reduce the chances of developing femoral neck shortness and delayed union or nonunion in adult patients with femoral neck fracture. Nevertheless, further studies (preferably RCTs) are required to validate the findings of our study.
Controversy remains around the available choices for the internal fixation of a femoral neck fracture. The femoral neck system (FNS) was developed in 2018 and has been widely applied since then as it can provide rigid fixation stability with less damage to the bone mass around the fracture.
No systematic reviews and meta-analyses have investigated the efficacy of the FNS in comparison with that of traditional internal fixation in the treatment of femoral fractures.
The purpose of our study was to assess the efficacy of the FNS in comparison with that of cannulated compression screws (CCS) in the treatment of femoral fractures through systematic review and meta-analysis.
Five electronic databases (PubMed, Embase, Cochrane Central Register of Controlled Trials, China National Knowledge Infrastructure, and Wanfang) were searched from the earliest publication date to December 31, 2021. Reference Citation Analysis (https://www.referencecitationanalysis.com/) was used to check the results and further analyze the related articles. Controlled trials were included if the FNS was applied to the femoral neck fracture in adults and if it was compared with CCS for the achievement of internal fixation. The measurement outcomes included the required operation time, observed patient blood loss, extent of fracture healing, patient’s Harris Hip score (HHS) at the last follow-up, and records of any complications (such as failure of internal fixation, femoral neck shortness, avascular necrosis of the femoral head, and delayed union or nonunion).
Ten retrospective controlled studies (involving 711 participants) were included in this meta-analysis. The meta-analysis showed that compared with CCS, use of the FNS could not decrease the operation time [standardized mean difference (SMD): -0.38, 95% confidence interval (CI): -0.98 to 0.22, P = 0.21, I2 = 93%], but it could increase the intraoperative blood loss (SMD: 0.59, 95%CI: 0.15 to 1.03, P = 0.009, I2 = 81%). The pooled results also showed that compared with CCS, the FNS could better promote fracture healing (SMD: -0.97, 95%CI: -1.65 to -0.30, P = 0.005, I2 = 91%), improve the HHS at the last follow-up (SMD: 0.76, 95%CI: 0.31 to 1.21, P = 0.0009, I2 = 84%), and reduce the chances of developing femoral neck shortness (OR: 0.29, 95%CI: 0.14 to 0.61, P = 0.001, I2 = 0%) and delayed union or nonunion (OR: 0.47, 95%CI: 0.30 to 0.73, P = 0.001; I2 = 0%) in adult patients with femoral neck fractures. However, there was no statistically significant difference between the FNS and CCS in terms of failure of internal fixation (OR: 0.49, 95%CI: 0.23 to 1.06, P = 0.07, I2 = 0%) and avascular necrosis of the femoral head (OR: 0.46, 95%CI: 0.20 to 1.10, P = 0.08, I2 = 0%).
Contemporary evidence indicates that compared with CCS, the FNS could decrease the chances of developing femoral neck shortness and delayed union or nonunion in adults with femoral neck fractures. Simultaneously, it could accelerate fracture healing and improve the HHS in these patients.
The FNS is an internal fixation method with superior characteristics in the treatment of femoral neck fractures. The results of this meta-analysis could help in the selection of the most appropriate treatment for patients with femoral neck fractures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Baek SH, South Korea; Kazeminia M, Iran; Virarkar M, United States S-Editor: Wu YXJ L-Editor: Webster JR P-Editor: Zhao S
| 1. | Number of All-Listed Diagnoses for Discharges from Short-Stay Hospitals, by ICD-9-CM Code: United States National Hospital Discharge Summary: CDC/NCHS National Hospital Discharge Survey; 2010 . [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 2. | Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res. 1990;252:163-166. [PubMed] [DOI] [Full Text] |
| 3. | Parker MJ. The management of intracapsular fractures of the proximal femur. J Bone Joint Surg Br. 2000;82:937-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Bretherton CP, Parker MJ. Early surgery for patients with a fracture of the hip decreases 30-day mortality. Bone Joint J. 2015;97-B:104-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 113] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 5. | Roberts KC, Brox WT. AAOS Clinical Practice Guideline: Management of Hip Fractures in the Elderly. J Am Acad Orthop Surg. 2015;23:138-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 111] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 6. | Hoshino CM, O'Toole RV. Fixed angle devices versus multiple cancellous screws: what does the evidence tell us? Injury. 2015;46:474-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Li J, Zhao Z, Yin P, Zhang L, Tang P. Comparison of three different internal fixation implants in treatment of femoral neck fracture-a finite element analysis. J Orthop Surg Res. 2019;14:76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 51] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 8. | Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3743] [Cited by in RCA: 5636] [Article Influence: 256.2] [Reference Citation Analysis (0)] |
| 9. | Shi J, Luo D, Weng H, Zeng XT, Lin L, Chu H, Tong T. Optimally estimating the sample standard deviation from the five-number summary. Res Synth Methods. 2020;11:641-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 285] [Article Influence: 57.0] [Reference Citation Analysis (0)] |
| 10. | Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785-1805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2418] [Cited by in RCA: 2321] [Article Influence: 331.6] [Reference Citation Analysis (0)] |
| 11. | Ren C, Ma T, Li M, Xu Y, Li Z, Sun L. Short-term effectiveness of femoral neck system in treatment of femoral neck fracture in young and middle-aged patients. Chin J Orthop Trauma. 2021;23:769-774. |
| 12. |
Yang J, Zhou X, Zhu W, Li L, Xu W, Xia R.
Comparison of short-term effectiveness of femoral neck system and cannulate compression screw in treatment of femoral neck fracture in young and middle-aged patient |
| 13. | Xiong W, Yi M, Long C, Liu L, Cen S, Huang F. Comparison of effectiveness of femoral neck system and inverted triangle cannulate screws in treatment of femoral neck fracture in adults. Zhonghua Chuangshang Guke Zazhi. 2021;23:748-753. |
| 14. | Yan C, Wang X, Xiang C, Jiang K, Li Y, Chen Q, Deng C, Chen L. [Comparison of effectiveness of femoral neck system and cannulate compression screw in treatment of femoral neck fracture in young and middle-aged patients]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35:1286-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 15. | Yang Y, Ma T, Zhang X, Luo X, Fan T, Wang Y. [Short-term effectiveness of femoral neck system in the treatment of femoral neck fracture]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35:539-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res. 2021;16:370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 17. | Zhou XQ, Li ZQ, Xu RJ, She YS, Zhang XX, Chen GX, Yu X. Comparison of Early Clinical Results for Femoral Neck System and Cannulated Screws in the Treatment of Unstable Femoral Neck Fractures. Orthop Surg. 2021;13:1802-1809. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 18. | He C, Lu Y, Wang Q, Ren C, Li M, Yang M, Xu Y, Li Z, Zhang K, Ma T. Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Musculoskelet Disord. 2021;22:994. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 19. | Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res. 2021;16:504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 55] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 20. | Vazquez O, Gamulin A, Hannouche D, Belaieff W. Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): short-term clinical and radiological outcomes. J Orthop Surg Res. 2021;16:477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 21. | Duffin M, Pilson HT. Technologies for Young Femoral Neck Fracture Fixation. J Orthop Trauma. 2019;33 Suppl 1:S20-S26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 22. | Slobogean GP, Stockton DJ, Zeng BF, Wang D, Ma B, Pollak AN. Femoral neck shortening in adult patients under the age of 55 years is associated with worse functional outcomes: Analysis of the prospective multi-center study of hip fracture outcomes in China (SHOC). Injury. 2017;48:1837-1842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 74] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 23. | Schopper C, Zderic I, Menze J, Müller D, Rocci M, Knobe M, Shoda E, Richards G, Gueorguiev B, Stoffel K. Higher stability and more predictive fixation with the Femoral Neck System versus Hansson Pins in femoral neck fractures Pauwels II. J Orthop Translat. 2020;24:88-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 24. | Ye Y, Chen K, Tian K, Li W, Mauffrey C, Hak DJ. Medial buttress plate augmentation of cannulated screw fixation in vertically unstable femoral neck fractures: Surgical technique and preliminary results. Injury. 2017;48:2189-2193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 25. | Fan Z, Huang Y, Su H, Jiang T. How to choose the suitable FNS specification in young patients with femoral neck fracture: A finite element analysis. Injury. 2021;52:2116-2125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 26. | Weil YA, Qawasmi F, Liebergall M, Mosheiff R, Khoury A. Use of fully threaded cannulated screws decreases femoral neck shortening after fixation of femoral neck fractures. Arch Orthop Trauma Surg. 2018;138:661-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 27. | Samsami S, Saberi S, Sadighi S, Rouhi G. Comparison of Three Fixation Methods for Femoral Neck Fracture in Young Adults: Experimental and Numerical Investigations. J Med Biol Eng. 2015;35:566-579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 94] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 28. | Sevitt S. Avascular necrosis and revascularisation of the femoral head after intracapsular fractures; a combined arteriographic and histological necropsy study. J Bone Joint Surg Br. 1964;46:270-296. [PubMed] |
| 29. | Dargan DP, Callachand F, Diamond OJ, Connolly CK. Three-year outcomes of intracapsular femoral neck fractures fixed with sliding hip screws in adults aged under sixty-five years. Injury. 2016;47:2495-2500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 30. | Augat P, Bliven E, Hackl S. Biomechanics of Femoral Neck Fractures and Implications for Fixation. J Orthop Trauma. 2019;33 Suppl 1:S27-S32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 89] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 31. | Rupprecht M, Grossterlinden L, Ruecker AH, de Oliveira AN, Sellenschloh K, Nüchtern J, Püschel K, Morlock M, Rueger JM, Lehmann W. A comparative biomechanical analysis of fixation devices for unstable femoral neck fractures: the Intertan versus cannulated screws or a dynamic hip screw. J Trauma. 2011;71:625-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 32. | Zielinski SM, Keijsers NL, Praet SF, Heetveld MJ, Bhandari M, Wilssens JP, Patka P, Van Lieshout EM; FAITH Trial Investigators. Femoral neck shortening after internal fixation of a femoral neck fracture. Orthopedics. 2013;36:e849-e858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 33. | Haider T, Schnabel J, Hochpöchler J, Wozasek GE. Femoral shortening does not impair functional outcome after internal fixation of femoral neck fractures in non-geriatric patients. Arch Orthop Trauma Surg. 2018;138:1511-1517. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 34. | van Walsum ADP, Vroemen J, Janzing HMJ, Winkelhorst T, Kalsbeek J, Roerdink WH. Low failure rate by means of DLBP fixation of undisplaced femoral neck fractures. Eur J Trauma Emerg Surg. 2017;43:475-480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |