Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11442
Peer-review started: June 19, 2022
First decision: August 22, 2022
Revised: September 10, 2022
Accepted: September 27, 2022
Article in press: September 27, 2022
Published online: November 6, 2022
Processing time: 127 Days and 13.2 Hours
It remains unclear whether video aids can improve the quality of bystander cardiopulmonary resuscitation (CPR).
To summarize simulation-based studies aiming at improving bystander CPR associated with the quality of chest compression and time-related quality parameters.
The systematic review was conducted according to the PRISMA guidelines. All relevant studies were searched through PubMed, EMBASE, Medline and Cochrane Library databases. The risk of bias was evaluated using the Cochrane collaboration tool.
A total of 259 studies were eligible for inclusion, and 6 randomised controlled trial studies were ultimately included. The results of meta-analysis indicated that video-assisted CPR (V-CPR) was significantly associated with the improved mean chest compression rate [OR = 0.66 (0.49-0.82), P < 0.001], and the proportion of chest compression with correct hand positioning [OR = 1.63 (0.71-2.55), P < 0.001]. However, the difference in mean chest compression depth was not statistically significant [OR = 0.18 (-0.07-0.42), P = 0.15], and V-CPR was not associated with the time to first chest compression compared to telecommunicator CPR [OR = -0.12 (-0.88-0.63), P = 0.75].
Video real-time guidance by the dispatcher can improve the quality of bystander CPR to a certain extent. However, the quality is still not ideal, and there is a lack of guidance caused by poor video signal or inadequate interaction.
Core Tip: This study conducted a systemic review and meta-analysis to summarized the outcomes of training programs aimed at improving bystander cardiopulmonary resuscitation associated with the quality of chest compressions and time-related quality parameters.
- Citation: Pan DF, Li ZJ, Ji XZ, Yang LT, Liang PF. Video-assisted bystander cardiopulmonary resuscitation improves the quality of chest compressions during simulated cardiac arrests: A systemic review and meta-analysis. World J Clin Cases 2022; 10(31): 11442-11453
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11442.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11442
Although the likelihood of survival with cardiac arrest (CA) is increasing, CA has emerged as the leading cause of death worldwide[1,2]. A meta-analysis showed that the aggregate survival rate of hospital discharge of adult patients with cardiac arrest (OHCA) was only 7.6%, which remained stable over the past 30 years[3]. Immediate cardiopulmonary resuscitation (CPR) is the most effective measure to improve the prognosis of patients with CA[4]. Studies have shown that the first witness's CPR can double the survival rate of patients with OHCA[5]. Generally, the patient’s family members are most likely to witness the occurrence of CA, and they are more willing to perform CPR on the spot. However, most CA witnesses are lacking life support knowledge and have not received any CPR training. Thus, they are not able to perform on-site CPR for patients with CA. An effective way to fill such short
DA-CPR has been widely carried out in European and American countries[6]. It has been proven that DA-CPR can increase the quality of CPR performed by the first witnesses[7] and improve the survival rate of victims with CA[8,9]. In 2015, the American Heart Association (AHA) included DA-CPR in the guidelines for cardiopulmonary resuscitation for the first time[10]. Many emergency medical service systems have established verbal CPR instructions to help callers cope with CPR. However, the quality of DA-CPR is still not ideal[11,12]. Although many efforts have been made to improve the quality of DA-CPR by modifying the command protocol, its actual effect is still not satisfactory[13-16].
The communication method of DA-CPR guidance is usually based on voice and telephone guidance. As a result, the quality of CPR performed by bystanders cannot be intuitively controlled, and a low-quality CPR is more likely to occur. Low-quality CPR may not improve the prognosis of patients with CA. Therefore, improving the quality of bystander CPR has become a focus of attention in recent years. With the advancement of wireless telecommunications, the introduction of video phones enables simultaneous voice and video commands. Video guidance via mobile phones can be a powerful tool for CPR guidance in emergency situations. For example, bystanders call CPR guidance and receive real-time voice instructions and video demonstrations via mobile phones, such as video self-learning programs. At the same time, the CPR performance of bystanders can be monitored and fed back to the dispatcher. Some preliminary studies have evaluated the possibility of applying video link instructions to improve the quality of bystander CPR[17], and the effect of video-assisted CPR (V-CPR) training has been extensively studied. Video self-learning procedures or video-based instructions have been documented to have more or at least as effective CPR training than conventional training methods[18-24]. However, the outcomes associated with V-CPR during simulated CAs remain unclear and await further study.
To address this issue, we conducted a systematic review and meta-analysis of quantitative studies to assess the effectiveness of video-assisted and telephone-assisted CPR in increasing chest compression rates during simulated CAs. The outcomes of training programs aimed at improving bystander CPR, including the quality of chest compression and time-related quality parameters, were analyzed in this study.
To answer the PICOS question, the inclusion criteria for our systematic review were as follows:
P: Subjects were adult volunteers or high school students, without any previous CPR training.
I: Intervention is a dispatcher initiated standardized video-guided CPR.
C: Control group dispatcher initiated standardized telephone-guided CPR.
O: Outcome indicators were: (1) The quality of chest compression, including the mean compression rate, the number of subjects who performed an adequate compression rate, the mean compression depth (between 5 and 6 cm), the number of subjects who performed an adequate compression depth, and adequate positioning of hands (on the lower half of the sternum); and (2) Time-related quality parameters, including time to initiate continuous compression, and total hands-off time (the pause between compressions longer than 1.5 s).
S: Research design is randomized simulation-based studies. We did not consider articles published in non-English journals, repetitive publications, no relevant outcome indicators, and unavailable or incomplete original data.
We searched PubMed, EMBASE, Medline, and Cochrane Library databases for studies published between the establishment time of the database to May 2021. The following search terms were used: “heart arrest”, “cardiopulmonary resuscitation”, “cardiac arrest” and “video-assisted”, “telephone-assisted”, “dispatcher-assisted”, etc. Take PubMed as a working example, Box 1 Lists the specific search strategy. In addition, we manually checked the reference list of each article for further appropriate studies.
Two researchers independently screened the articles, extracted data, and cross-checked them. If there is a disagreement, it will be resolved through discussion or negotiation with a third party. After excluding the irrelevant documents, the abstract and full text of each article were thoroughly read to determine its eligibility. If necessary, the authors of an original research article will be contacted via email or telephone to obtain the missing information. The following data were extracted: (1) Basic information of the included studies, including research titles, first authors, published journals, etc.; (2) Baseline characteristics and intervention measures of the research object; (3) Key elements of the risk of bias evaluation; and (4) Outcome measures and performance indicators.
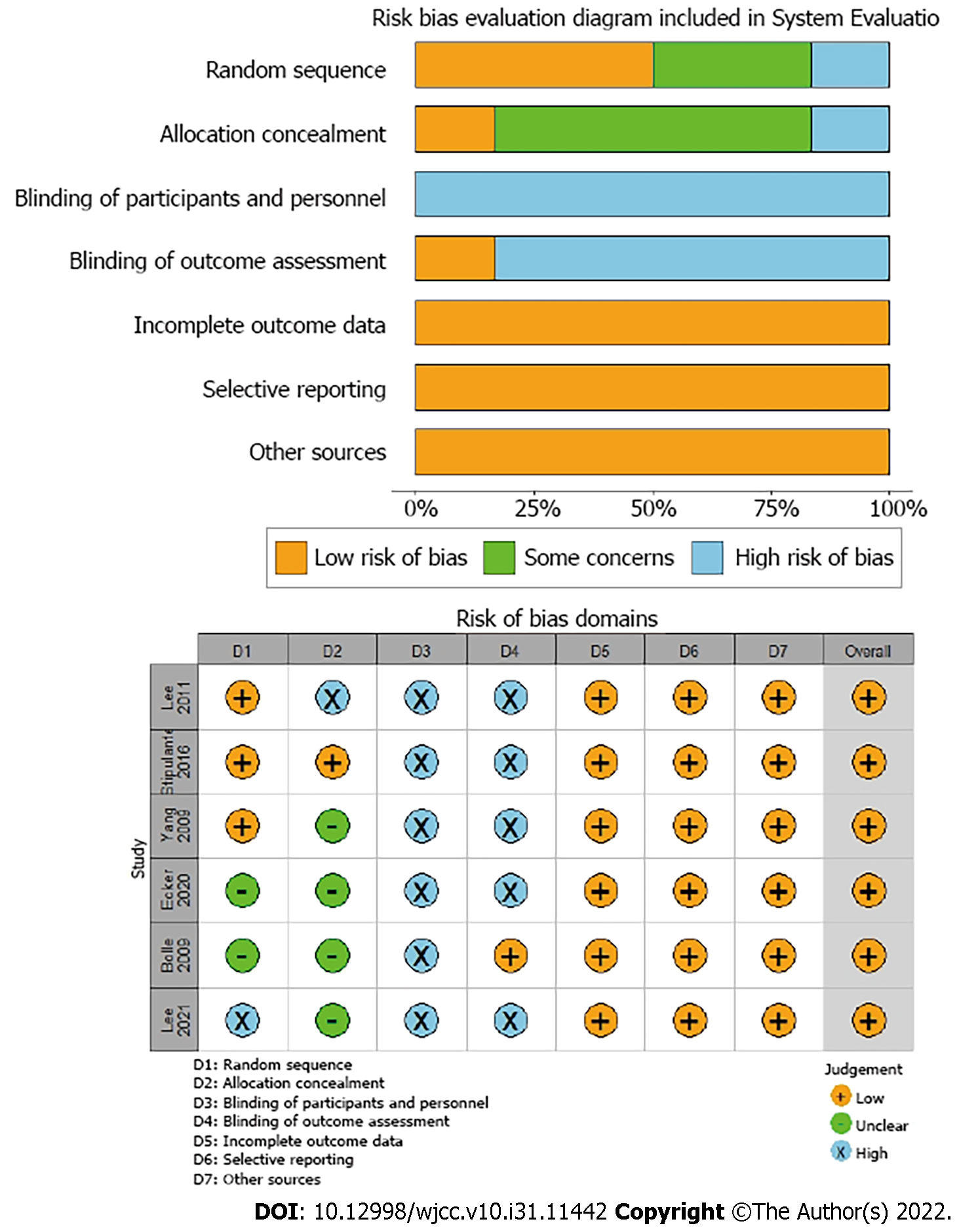
Two investigators independently evaluated the risk of bias for the included studies and cross-checked the results. The Cochrane handbook version 5.1.0 was used for assessing the risk of bias.
Meta-analysis was conducted with version 13.0 Stata software. The count data were analyzed by calculating the odds ratio (OR) and its 95% confidence interval (CI). The measurement data involved different research types and measurement methods. Thus, the standardized mean difference was used as an effect indicator, and each effect size was given a point. The heterogeneity among the included studies was analyzed by the χ2 test (α = 0.1), and the I2 statistic was used to quantitatively judge the size of the heterogeneity. If there was no statistical heterogeneity, the fixed-effects model was used for interpreting the meta-analysis results; otherwise, the random-effects model was chosen and the source of the heterogeneity was further analyzed. Meanwhile, obvious clinical heterogeneity was analyzed descriptively.
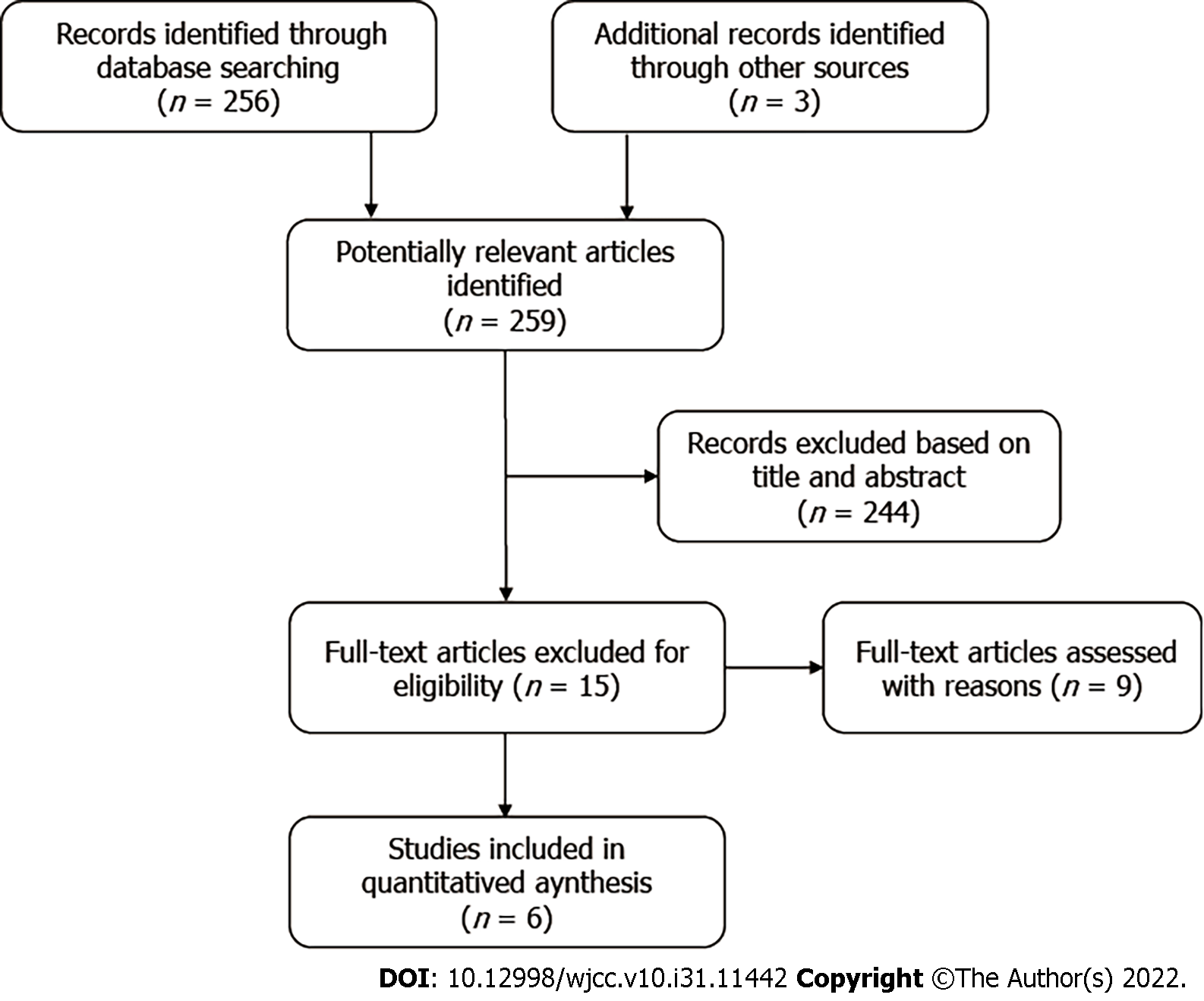
A total of 259 relevant articles were retrieved by searching the online databases. Six studies[25], involving 537 volunteers, were included after layer-by-layer screening. The flow diagram of the study selection is illustrated in Figure 1. The basic characteristics of the included studies are demonstrated in Table 1. The results of the risk of bias assessment are shown in Figure 2.
| Ref. | Loction | Study period | Subjects | Number of Subjects | Scenarios duration | Experiment procedure | Assessment | ||
| V-CPR | T-CPR | V-CPR | T-CPR | ||||||
| Lee et al[25], 2021 | Korea | October 2019 to July 2020 | Volunteers aged 18 years or older | 88 | 43 | 6 min | Video call transition was performed after initiation of by stander chest compression | The dispatcher uses a standard audio instructed protocol to help the participant initiate and perform chest compression-only CPR | (1) The mean proportion of ade quate hand positioning during chest compressions; (2) The mean compres sion depth; (3) Mean compression rate; and (4) Total no-flow time |
| Yang et al[26], 2009 | Taiwan | - | Volunteers above 16 years of age who have not received any CPR training within the last 5 years | 43 | 53 | 4 min | Received interactive voice and video demonstration and feedback via a video cell phone | Received only voice CPR instruction | (1) Chest compressions rate; (2) Chest compressions depth; (3) Proportion of subjects with sufficient rate; (4) Proportion of chest compressions with appropriate depth; (5) Proportion of correct hand positioning; (6) Hands-off time; (7) Time to first chest compression; and (8) Total duration of CPR instructions |
| Ecker et al[27], 2020 | Cologne | July to August 2018 | Adult volunteer, lay people without any previous CPR training | 50 | 50 | 8 min | The study assistant operated the camera function of the phone, volunteers activated EmergencyEye and started standardised video guided CPR | The study assistant enabled the phone’s speaker function, the EMS dispatcher then initiated standardised telephone guided CPR | (1) Compression frequency 100 to 120 min–1; (2) Ccompression depth 5 to 6 cm; and (3) Correct hand position on the lower third of the sternum |
| Lee et al[28], 2011 | Korea | May 2010 to June 2010 | Adult volunteer,lay people without any previous CPR training | 39 | 39 | 5 min | Instructed to make a voice call to a number, guided on how to play a video stored on the phone, and were further asked to do as shown on the video until the emergency medical technicians arrived | Instructed to make a phone call to the same number, where they were guided by a dispatcher using the standardised protocol to perform compression-only CPR | (1) The mean compression rate; (2) The number of subjects who performed an adequate compression rate; (3) The mean compression depth; (4) The number of subjects who performed an adequate compression depth; (5) Adequate positioning of hands; (6) Time to initiate continuous compressions; (7) Hands-off time; and (8) The number of subjects who had no “hands-off” event after starting compressions |
| Stipulante et al[29], 2016 | Belgium | March 2013 | High school Students volunteers, 16-25 | 60 | 60 | 8 min | Developed an original protocol of videoconference CPR instructions on the basis of the ALERT algorithm, followed the dispatcher’s instructions and performed CPR | Guided according to the ALERT protocol, given the instruction to ‘put the speaker on’ and to ‘put the phone down’ to receive further instruction | (1) Rate of chest compressions; (2) Total number of chest compressions; (3) Depth of chest compressions; (4) Proportion of chest compressions with appropriate rate; (5) Proportion of chest compression with appropriate depth; (6) Proportion of chest compressions with correct hand positioning; (7) Time for responsiveness check; (8) Time for airway opening; (9) Time for breathing check; (10) Time to first compression; and (11) Hands-off time |
| Bolle et al[30], 2009 | Norway | December 2006 and January 2007 | High-school students | 29 | 26 | 10 min | Dispatchers used a lap_x0002_top with a UMTS (3G) card, video camera, videovcommunication software and a standard headset | Dispatchers used a telephone with a standard headset | (1) Total number of compressions; (2) Average depth (mm); (3) Average rate (n/min); (4) Average number per minute; (5) Proportion done without error; (6) Proportion done to correct depth; (7) Proportion with correct hand position; (8) Proportion done with full release; (9) Time to first compression (s); and (10) Total hands-off-chest time (s) |
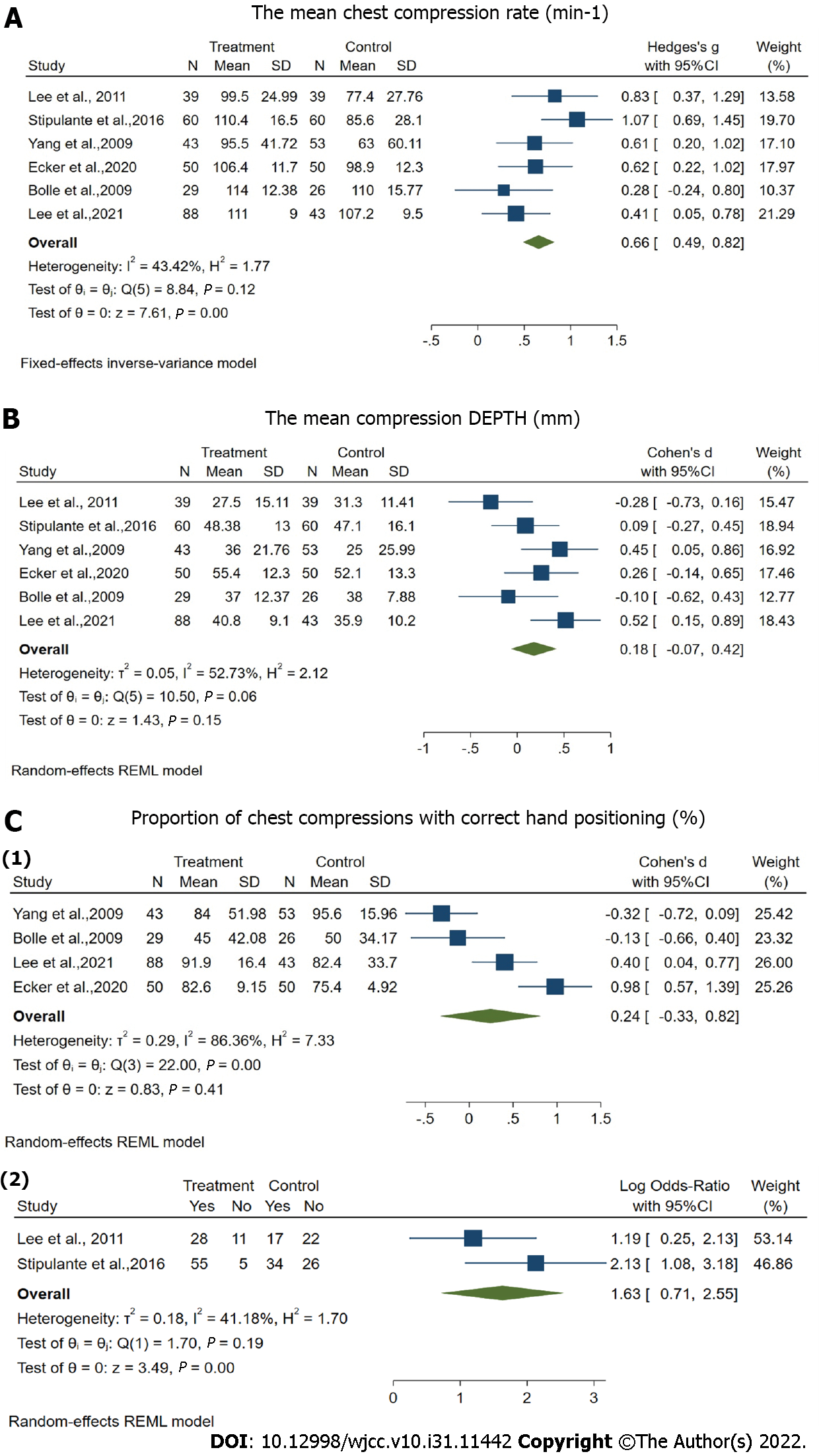
The mean chest compression rate was reported in all six studies involving 537 volunteers[25]. The results of the fixed-effects inverse-variance model indicated that video-guided CPR was significantly associated with the improved mean chest compression rate [OR = 0.66, 95%CI: 0.49-0.82, P < 0.001] (Figure 3A). The weighted mean chest compression rate increased from 92.01 min-1 in telecommunicator CPR (T-CPR) group to 105.62 min-1 in V-CPR group.
The mean chest compression depth was reported in all six studies (25-30) involving 537 volunteers. The results of random-effects REML model showed that the difference in the mean chest compression depth between the two groups was not statistically significant [OR = 0.18, 95%CI: -0.07-0.42, P = 0.15] (Figure 3B). The proportion of chest compression with correct hand positioning was reported in all six studies. However, four studies set this indicator as a continuous variable and the other two studies set as the dichotomous variables[26,27]. The first four studies included 382 volunteers, and the results of random-effects REML model indicated that no significant difference was found between the T-CPR and V-CPR groups [OR = 0.24, 95%CI: -0.33-0.82, P = 0.41] (Figure 3C). The last two studies included 155 volunteers, and the results of random-effects REML model indicated that V-CPR was significantly associated with the improved proportion of chest compression with correct hand positioning [OR = 1.63, 95%CI: 0.71-2.55, P < 0.001] (Figure 3C).
There was obvious statistical heterogeneity in the number of subjects who performed adequate chest compression and the proportion of chest compression with appropriate depth. Thus, a qualitative description was provided. Three out of the four studies[26-28] demonstrated that the number of subjects who performed adequate chest compression was significantly higher in V-CPR group than in T-CPR group. One out of the five studies[28] indicated that the proportion of chest compression with appropriate depth in V-CPR was significantly greater than that in T-CPR group.
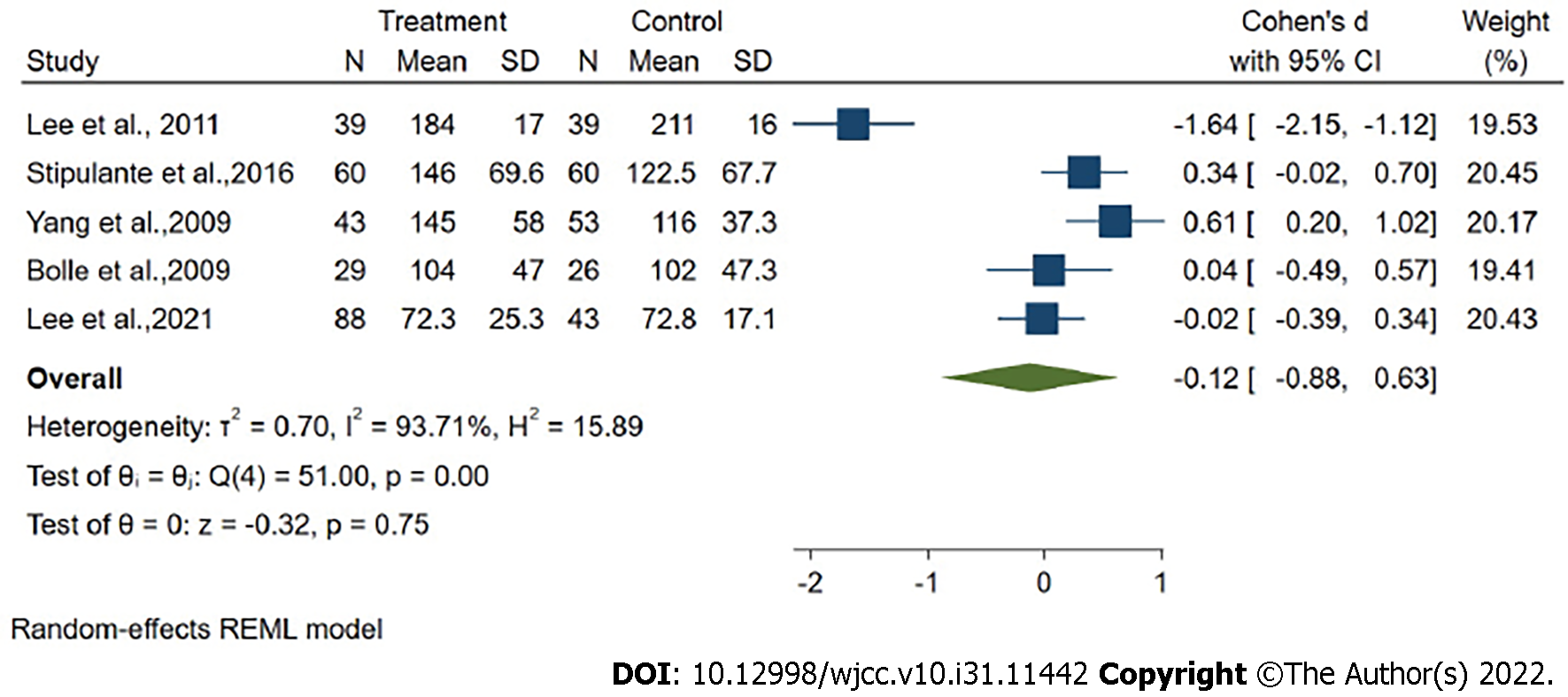
Time to first chest compression was reported in five studies[25] involving 480 volunteers. The results of random-effects REML model showed that V-CPR was not associated with the time to first chest compression compared to T-CPR[OR = -0.12, 95%CI: -0.88-0.63, P = 0.75] (Figure 4).
“Hands-off” time was reported in four studies[26-29]. However, the statistical heterogeneity was apparent; thus, the qualitative description was used. Two studies[27,29] indicated that volunteers guided by telephone interrupted their chest compression more frequently; and two other studies[26,28] showed a longer hands-off time in V-CPR group due to the poor quality of the signal, and chest compression was delayed or broken off.
In addition to the instructor and guidance factors, the modes of communication, including telephone voice guidance and remote video online guidance, are important factors affecting the quality of DA-CPR. Video instructions through a telephone can be a potentially powerful tool for CPR instruction in emergencies. Previous studies showed that DA-CPR with video instructions improved rescuers’ self-reported confidence, which could positively affect the number of bystanders willing to start CPR[30]. Besides, video-calls influenced the information basis and understanding of the dispatchers, thereby improving the rescuer compliance[17].
There is no unified quality evaluation standard for DA-CPR at home and abroad, but in the comprehensive literature[31,32], the overall quality evaluation index recommends the time of dispatcher accepting emergency calls to judge suspected OHCA, time of starting guidance CPR, time of starting chest compression, location of chest compression, frequency and depth, etc. The AHA 2015 guidelines recommended high-quality CPR requiring adequate chest compression depth (50-60 mm), adequate chest compression rate (100-120/min), full chest wall recoil, minimal pause in chest compression, correct hand position during compression, and avoidance of hyperventilation[10].
Our systematic review included 6 randomized controlled trials reporting on the quality of DA-CPR under different communication methods. The meta-analysis results showed that video communication could improve the average chest compression rate of bystanders during simulated CAs. The compression speed increased from an average of 92 min-1 in the telephone group to more than 100 min-1, reaching the standard compression rate for CPR. Abella et al[22] found that a high chest compression rate was significantly related to the initial return of spontaneous circulation. It is expected that the compression speed improved by video communication can be transformed into a better chance of survival in reality. If the chest compressions are guided by a moving video, it will be easier to maintain a proper chest compression rate. However, by judging from the number of subjects who performed an adequate compression rate, there was still a 10%-70% proportion of subjects who did not achieve an adequate compression rate. This reminds us that when guiding bystanders to perform cardiopulmonary resuscitation, we must emphasize that the compression frequency of bystanders reaches 100-120 times/min as recommended by the AHA guidelines.
The depth of chest compression is another key factor in high-quality CPR. Our meta-analysis revealed that video communication did not improve the average chest compression depth of bystanders during simulated CAs. At the same time, most of the compression depths did not meet the 2015 AHA guidelines for high-quality CPR to a depth of at least 5-6 cm in adults. Regardless of T-CPR or V-CPR, it is realized through interactive real-time feedback between dispatchers and subjects. In this study, most CPR performances did not meet the recommended compression depth. Therefore, it is necessary to emphasize the depth of chest compression during interactive counseling, either through video presentations or phone calls.
According to the AHA and European Resuscitation Council guidelines as the correct hand position on the lower half of the sternum[33]. In the included 6 randomized controlled trials, different description methods resulted in divergent results regarding the correct hand position during chest compression. When as a continuous variable, four studies indicated there was no significant difference between the V-CPR and T-CPR groups, but as dichotomous variable, the other two studies showed V-CPR was significantly associated with the included proportion of chest compression with correct hand positioning. In the included studies, the correct hand position of the participants in T-CPR group was only 43.6%, and that of the participants in V-CPR group was only 45%. The possible reason is that the subjects in T-CPR group may call the dispatcher to ask questions, thus, the position of their hands is changed during chest compression. Video-guided CPR should be able to guide the correct hand position more intuitively to improve the correct hand position. However, some volunteers did not correct their hand position according to the instructions provided in the CPR video, which might be attributed to the small screen or location of the mobile phone. Different positions of the video phone may help to monitor and feedback the quality of CPR performed, such as the horizontal positioning, thereby achieving the adequate compression depth; on the other hand, the bird's eye view can optimize the judgment of hand positioning. Nevertheless, further research is needed to determine the best location of the video phone and the information obtained during DA-CPR.
Time to first chest compression is an important time-related quality parameter. In this meta-analysis, the V-CPR group had no significant improvement in time to first chest compression compared to the T-CPR group. In fact, only one study showed that the time to first chest compression was 72 s; while the remaining 5 studies were all greater than 100 s, and the longest record reached 211 s. Such delay can exhibit an impact on the survival rate of patients with CA. These were limited by the low quality of the video connection and poor training of the dispatcher in using video calls. Although the dispatcher gave accurate instructions, the bystanders in T-CPR group lacked a clear understanding and repeatedly asked questions, thus resulting in a time extension.
There were some inevitable limitations to this systematic review and meta-analysis. Firstly, this study incorporated simulation trials with mannequins, while might not represent real-life CAs. In fact, some bystanders can get plagued with fear; thus, more real-life studies with standardized protocols are needed in the future. Secondly, although the 2015 AHA guidelines recommended that dispatchers should provide CPR instructions with only chest compression for adults with suspected OHCA, the emergency medical services are different and there are no unified standardized scheduling tools, hence, the instructions provided by the dispatcher may be varied. Thirdly, the research subjects included both adult volunteers and high school students, which could lead to differences in CPR quality due to their ability to learn from mobile videos. Although adult volunteers (average age = 50 years) reported that they had no difficulty watching and understanding mobile videos, further research should target on older volunteers who are more likely to encounter patients with CA. Fourthly, most included studies did not report the adjusted ORs of primary outcomes, and the ORs calculated by cross-tabs did not consider confounding factors. Therefore, the results of this meta-analysis should be interpreted with caution.
This study reveals that the average rate of chest compression during simulated CAs can be improved by video-guided bystander CPR. However, the mean chest compression depth and time-related quality parameters, such as the first chest compression and “hand-off” time, demonstrate no significant improvement in V-CPR group. Video real-time guidance by the dispatcher can improve the quality of the bystander CPR to a certain extent, but the quality is still not ideal, and there is a lack of guidance caused by poor video signal or inadequate interaction.
It remains unclear whether video aids can improve the quality of bystander cardiopulmonary resuscitation (CPR).
To prove whether video aids can improve the quality of bystander CPR.
To summarize simulation-based studies aiming at improving bystander CPR associated with the quality of chest compression and time-related quality parameters.
Meta analysis.
V-CPR was significantly associated with the improved mean chest compression rate, and the proportion of chest compression with correct hand positioning.
Video real-time guidance by the dispatcher can improve the quality of bystander CPR to a certain extent. However, the quality is still not ideal, and there is a lack of guidance caused by poor video signal or inadequate interaction.
Real-time video coaching of clinical application dispatchers to improve the quality of bystander CPR.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Emergency medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aydin S, Turkey; Gupta P, United States; Lakusic N, Croatia; Shanmugasundaram M, United States S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation. 2010;81:1479-1487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1588] [Cited by in RCA: 1474] [Article Influence: 98.3] [Reference Citation Analysis (0)] |
| 2. | Wong CX, Brown A, Lau DH, Chugh SS, Albert CM, Kalman JM, Sanders P. Epidemiology of Sudden Cardiac Death: Global and Regional Perspectives. Heart Lung Circ. 2019;28:6-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 318] [Article Influence: 53.0] [Reference Citation Analysis (0)] |
| 3. | Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1316] [Cited by in RCA: 1569] [Article Influence: 98.1] [Reference Citation Analysis (0)] |
| 4. | Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, Abella BS, Kleinman ME, Edelson DP, Berg RA, Aufderheide TP, Menon V, Leary M; CPR Quality Summit Investigators, the American Heart Association Emergency Cardiovascular Care Committee, and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128:417-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 582] [Cited by in RCA: 705] [Article Influence: 58.8] [Reference Citation Analysis (0)] |
| 5. | Dumas F, Rea TD, Fahrenbruch C, Rosenqvist M, Faxén J, Svensson L, Eisenberg MS, Bohm K. Chest compression alone cardiopulmonary resuscitation is associated with better long-term survival compared with standard cardiopulmonary resuscitation. Circulation. 2013;127:435-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Zachariah BS, Pepe PE. The development of emergency medical dispatch in the USA: a historical perspective. Eur J Emerg Med. 1995;2:109-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Mirhaghi A, Shafaee H, Malekzadeh J, Hasanzadeh F. Recognizing Sudden Cardiac Arrest May Require More Than Two Questions during Telephone Triage: Developing a Complementary Checklist. Bull Emerg Trauma. 2017;5:104-109. [PubMed] |
| 8. | Kellermann AL, Hackman BB, Somes G. Dispatcher-assisted cardiopulmonary resuscitation. Validation of efficacy. Circulation. 1989;80:1231-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 75] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Ro YS, Shin SD, Lee YJ, Lee SC, Song KJ, Ryoo HW, Ong MEH, McNally B, Bobrow B, Tanaka H, Myklebust H, Birkenes TS. Effect of Dispatcher-Assisted Cardiopulmonary Resuscitation Program and Location of Out-of-Hospital Cardiac Arrest on Survival and Neurologic Outcome. Ann Emerg Med. 2017;69:52-61.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 101] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 10. | Perkins GD, Travers AH, Berg RA, Castren M, Considine J, Escalante R, Gazmuri RJ, Koster RW, Lim SH, Nation KJ, Olasveengen TM, Sakamoto T, Sayre MR, Sierra A, Smyth MA, Stanton D, Vaillancourt C. Part 3: Adult basic life support and automated external defibrillation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation Oct. 2015;95:e43-69. [RCA] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 147] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 11. | Zhang L, Luo M, Myklebust H, Pan C, Wang L, Zhou Z, Yang Q, Lin Q, Zheng ZJ. When dispatcher assistance is not saving lives: assessment of process compliance, barriers and outcomes in out-of-hospital cardiac arrest in a metropolitan city in China. Emerg Med J. 2021;38:252-257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Soar J, Maconochie I, Wyckoff MH, Olasveengen TM, Singletary EM, Greif R, Aickin R, Bhanji F, Donnino MW, Mancini ME, Wyllie JP, Zideman D, Andersen LW, Atkins DL, Aziz K, Bendall J, Berg KM, Berry DC, Bigham BL, Bingham R, Couto TB, Böttiger BW, Borra V, Bray JE, Breckwoldt J, Brooks SC, Buick J, Callaway CW, Carlson JN, Cassan P, Castrén M, Chang WT, Charlton NP, Cheng A, Chung SP, Considine J, Couper K, Dainty KN, Dawson JA, de Almeida MF, de Caen AR, Deakin CD, Drennan IR, Duff JP, Epstein JL, Escalante R, Gazmuri RJ, Gilfoyle E, Granfeldt A, Guerguerian AM, Guinsburg R, Hatanaka T, Holmberg MJ, Hood N, Hosono S, Hsieh MJ, Isayama T, Iwami T, Jensen JL, Kapadia V, Kim HS, Kleinman ME, Kudenchuk PJ, Lang E, Lavonas E, Liley H, Lim SH, Lockey A, Lofgren B, Ma MH, Markenson D, Meaney PA, Meyran D, Mildenhall L, Monsieurs KG, Montgomery W, Morley PT, Morrison LJ, Nadkarni VM, Nation K, Neumar RW, Ng KC, Nicholson T, Nikolaou N, Nishiyama C, Nuthall G, Ohshimo S, Okamoto D, O'Neil B, Yong-Kwang Ong G, Paiva EF, Parr M, Pellegrino JL, Perkins GD, Perlman J, Rabi Y, Reis A, Reynolds JC, Ristagno G, Roehr CC, Sakamoto T, Sandroni C, Schexnayder SM, Scholefield BR, Shimizu N, Skrifvars MB, Smyth MA, Stanton D, Swain J, Szyld E, Tijssen J, Travers A, Trevisanuto D, Vaillancourt C, Van de Voorde P, Velaphi S, Wang TL, Weiner G, Welsford M, Woodin JA, Yeung J, Nolan JP, Hazinski MF. 2019 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation. 2019;140:e826-e880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 135] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 13. | Panchal AR, Berg KM, Cabañas JG, Kurz MC, Link MS, Del Rios M, Hirsch KG, Chan PS, Hazinski MF, Morley PT, Donnino MW, Kudenchuk PJ. 2019 American Heart Association Focused Update on Systems of Care: Dispatcher-Assisted Cardiopulmonary Resuscitation and Cardiac Arrest Centers: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2019;140:e895-e903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Craig-Brangan KJ, Day MP. Update: AHA guidelines for CPR and emergency cardiovascular care. Nursing. 2020;50:58-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Ecker H, Lindacher F, Adams N, Hamacher S, Wingen S, Schier R, Böttiger BW, Wetsch WA. Video-assisted cardiopulmonary resuscitation via smartphone improves quality of resuscitation: A randomised controlled simulation trial. Eur J Anaesthesiol. 2020;37:294-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 16. | Tanaka Y, Taniguchi J, Wato Y, Yoshida Y, Inaba H. The continuous quality improvement project for telephone-assisted instruction of cardiopulmonary resuscitation increased the incidence of bystander CPR and improved the outcomes of out-of-hospital cardiac arrests. Resuscitation. 2012;83:1235-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 17. | Johnsen E, Bolle SR. To see or not to see--better dispatcher-assisted CPR with video-calls? Resuscitation. 2008;78:320-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Hamasu S, Morimoto T, Kuramoto N, Horiguchi M, Iwami T, Nishiyama C, Takada K, Kubota Y, Seki S, Maeda Y, Sakai Y, Hiraide A. Effects of BLS training on factors associated with attitude toward CPR in college students. Resuscitation. 2009;80:359-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 19. | Cho GC, Sohn YD, Kang KH, Lee WW, Lim KS, Kim W, Oh BJ, Choi DH, Yeom SR, Lim H. The effect of basic life support education on laypersons' willingness in performing bystander hands only cardiopulmonary resuscitation. Resuscitation. 2010;81:691-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 81] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 20. | Einspruch EL, Lynch B, Aufderheide TP, Nichol G, Becker L. Retention of CPR skills learned in a traditional AHA Heartsaver course versus 30-min video self-training: a controlled randomized study. Resuscitation. 2007;74:476-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 182] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 21. | Reder S, Cummings P, Quan L. Comparison of three instructional methods for teaching cardiopulmonary resuscitation and use of an automatic external defibrillator to high school students. Resuscitation. 2006;69:443-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 102] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 22. | Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O'Hearn N, Wigder HN, Hoffman P, Tynus K, Vanden Hoek TL, Becker LB. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111:428-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 500] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 23. | Batcheller AM, Brennan RT, Braslow A, Urrutia A, Kaye W. Cardiopulmonary resuscitation performance of subjects over forty is better following half-hour video self-instruction compared to traditional four-hour classroom training. Resuscitation. 2000;43:101-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 121] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Monsieurs KG, Vogels C, Bossaert LL, Meert P, Manganas A, Tsiknakis M, Leisch E, Calle PA, Giorgini F. Learning effect of a novel interactive basic life support CD: the JUST system. Resuscitation. 2004;62:159-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Lee SGW, Kim TH, Lee HS, Shin SD, Song KJ, Hong KJ, Kim JH, Park YJ. Efficacy of a new dispatcher-assisted cardiopulmonary resuscitation protocol with audio call-to-video call transition. Am J Emerg Med. 2021;44:26-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | Stipulante S, Delfosse AS, Donneau AF, Hartsein G, Haus S, D'Orio V, Ghuysen A. Interactive videoconferencing versus audio telephone calls for dispatcher-assisted cardiopulmonary resuscitation using the ALERT algorithm: a randomized trial. Eur J Emerg Med. 2016;23:418-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 27. | Lee JS, Jeon WC, Ahn JH, Cho YJ, Jung YS, Kim GW. The effect of a cellular-phone video demonstration to improve the quality of dispatcher-assisted chest compression-only cardiopulmonary resuscitation as compared with audio coaching. Resuscitation. 2011;82:64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 28. | Yang CW, Wang HC, Chiang WC, Hsu CW, Chang WT, Yen ZS, Ko PC, Ma MH, Chen SC, Chang SC. Interactive video instruction improves the quality of dispatcher-assisted chest compression-only cardiopulmonary resuscitation in simulated cardiac arrests. Crit Care Med. 2009;37:490-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 29. | Bolle SR, Scholl J, Gilbert M. Can video mobile phones improve CPR quality when used for dispatcher assistance during simulated cardiac arrest? Acta Anaesthesiol Scand. 2009;53:116-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 30. | Bolle SR, Johnsen E, Gilbert M. Video calls for dispatcher-assisted cardiopulmonary resuscitation can improve the confidence of lay rescuers--surveys after simulated cardiac arrest. J Telemed Telecare. 2011;17:88-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Dameff C, Vadeboncoeur T, Tully J, Panczyk M, Dunham A, Murphy R, Stolz U, Chikani V, Spaite D, Bobrow B. A standardized template for measuring and reporting telephone pre-arrival cardiopulmonary resuscitation instructions. Resuscitation. 2014;85:869-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 32. | Lerner EB, Rea TD, Bobrow BJ, Acker JE 3rd, Berg RA, Brooks SC, Cone DC, Gay M, Gent LM, Mears G, Nadkarni VM, O'Connor RE, Potts J, Sayre MR, Swor RA, Travers AH; American Heart Association Emergency Cardiovascular Care Committee; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Emergency medical service dispatch cardiopulmonary resuscitation prearrival instructions to improve survival from out-of-hospital cardiac arrest: a scientific statement from the American Heart Association. Circulation. 2012;125:648-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 150] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 33. | Maconochie IK, Bingham R, Eich C, López-Herce J, Rodríguez-Núñez A, Rajka T, Van de Voorde P, Zideman DA, Biarent D; Paediatric life support section Collaborators. European Resuscitation Council Guidelines for Resuscitation 2015: Section 6. Paediatric life support. Resuscitation. 2015;95:223-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 284] [Article Influence: 28.4] [Reference Citation Analysis (0)] |