Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11349
Peer-review started: February 4, 2022
First decision: June 15, 2022
Revised: July 28, 2022
Accepted: September 27, 2022
Article in press: September 27, 2022
Published online: November 6, 2022
Processing time: 265 Days and 1 Hours
Patellar tendon rupture after total knee arthroplasty (TKA) is a catastrophic com
To introduce a direct repair method for early patella tendon rupture following TKA and determine the clinical outcomes and complications of this method.
During the period of 2008 to 2021, 3265 consecutive TKAs were retrospectively reviewed. Twelve patients developed early patellar tendon rupture postoperatively and were treated by a direct repair method. Mean follow-up was 5.7 years. Demographic, operative, and clinical data were collected. The clinical outcomes were assessed using the Western Ontario and McMaster Universities (WOMAC) score, the Hospital for Special Surgery (HSS) score, knee range of motion, extensor lag, and surgical complications. Descriptive statistics and paired t test were employed to analyze the data.
For all 12 patients who underwent direct repair for early patellar tendon rupture, 3 patients failed: One (8.3%) for infection and two (17.6%) for re-fracture. The two patients with re-fracture both underwent reoperation to reconstruct the extensor mechanism and the patient with infection underwent revision surgery. The range of motion was 109.2° ± 10.6° preoperatively to 87.9° ± 11° postoperatively, mean extensor lag was 21° at follow-up, and mean WOMAC and HSS scores were 65.8 ± 30.9 and 60.3 ± 21.7 points, respectively.
This direct repair method of early patellar tendon rupture is not an ideal therapy. It is actually ineffective for the recovery of knee joint function in patients, and is still associated with severe knee extension lag and high complication rates. Compared with the outcomes of other repair methods mentioned in the literature, this direct repair method shows poor clinical outcomes.
Core Tip: This direct repair method of early patella tendon rupture showed unsatisfactory clinical results in this group of patients, and it was actually ineffective for the recovery of knee joint function in patients. Therefore, we suggested that direct repair should not be the preferred method to treat early patella tendon rupture, but other reconstruction methods should be boldly chosen. Our experience would be instructive for clinicians to treat early patella tendon rupture.
- Citation: Li TJ, Sun JY, Du YQ, Shen JM, Zhang BH, Zhou YG. Early patellar tendon rupture after total knee arthroplasty: A direct repair method. World J Clin Cases 2022; 10(31): 11349-11357
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11349.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11349
Patellar tendon rupture after total knee arthroplasty (TKA) is a catastrophic complication. Although the occurrence of this injury is rare, with a reported prevalence between 0.17%-1%, it can lead to significant dysfunction for the patient and is very tricky to deal with[1]. The cause of the lesion can be traumatic or atraumatic[2]. Traumatic rupture is mostly caused by direct trauma, such as a fall[1]. Atraumatic ruptures may occur in degenerative tendons, and are usually secondary to immunocompromised conditions such as rheumatoid arthritis, systemic lupus erythematosus, diabetes mellitus, or long-term use of steroids, to an infection, or to iatrogenic causes[3,4].
Patellar tendon rupture occurring within 3 mo of TKA were considered early injuries, and all other injuries were considered late injuries[5]. Non-operative treatment of these injuries often results in chronic pain, difficulty with ambulation, extensor lag, decreased range of motion (ROM), limb instability, and increased fall risk[6]. Operation must be considered if return to previous level of function and optimal ROM is desired. There are multiple surgical options for patellar tendon rupture, including direct repair (e.g., suture or suture anchor), reconstruction with allograft [e.g., Achilles tendon allograft and whole extensor mechanism (EM) allograft], augmentation (e.g., semitendinosus tendon), and synthetic material (e.g., Marlex mesh)[7-9].
For early patellar tendon rupture, most surgeons still attempt to perform direct repair by drilling tunnels or suture anchors, but the results have been historically poor with complication rates approaching 50%[10]. For chronic injuries, direct repair is not suitable, while reconstruction with allografts has been proposed as an alternative treatment for EM injuries[10]. Results following allograft reconstruction are uncertain, with some series reporting failure rates closing to 40%, while others report patient satisfaction rates of approximately 89%[11-15]. Direct repair of the EM presents many challenges both to the surgeon as well as the patient, and there is no consensus regarding optimal treatment. For the treatment of patellar tendon rupture, many surgical methods have not obtained satisfactory results. Nevertheless, there are very limited published reports of direct repair of early patellar tendon rupture in arthroplasty patients at present.
The primary aim of this study was to introduce a direct repair method for early patella tendon rupture following TKA, determine the clinical outcomes and complications of this method, and compare these results to similar studies to summarize potential advantages and disadvantages.
We retrospectively reviewed the medical records of all patients who underwent TKA from 2008 to 2021 and were eligible for inclusion in this study. Patients with early patellar tendon rupture after TKA were included. Patients with EM injuries and limited motion of the hip or ankle before surgery were excluded. Sex, age, weight, and height of each patient were recorded. Radiological data included a weightbearing full length lower extremity antero-posterior radiograph performed with centered patella showing the entire lower limb, a medio-lateral view performed strictly perpendicularly to the superior face of tibial condyles, and an anterio-posterior view performed with strictly centered patella. These radiological data included films taken by the patients before and 3 mo after operation. A consecutive series of 12 patients (1 man and 11 women; mean age 69 years; age range 59-81 years) were found to have patellar tendon rupture following TKA. In the 12 patients, three had a partial rupture of the patellar tendon, while the remaining nine had a complete rupture. All the patients had good tissue quality. The preoperative diagnosis was osteoarthritis in 11 patients and inflammatory arthritis in one. The median follow-up period was 5.7 years (range 3.3-10.6 years). The average time from patellar tendon rupture to repair was 1.0 ± 1.1 mo (range 0-3 mo). No patients were lost to follow-up. All surgeries were performed by a senior surgeon. Patients were clinically assessed pre- and post-operatively using ROM, extensor lag, Western Ontario and McMaster Universities (WOMAC) score, the Hospital for Special Surgery (HSS) score, and radiographic evaluation.
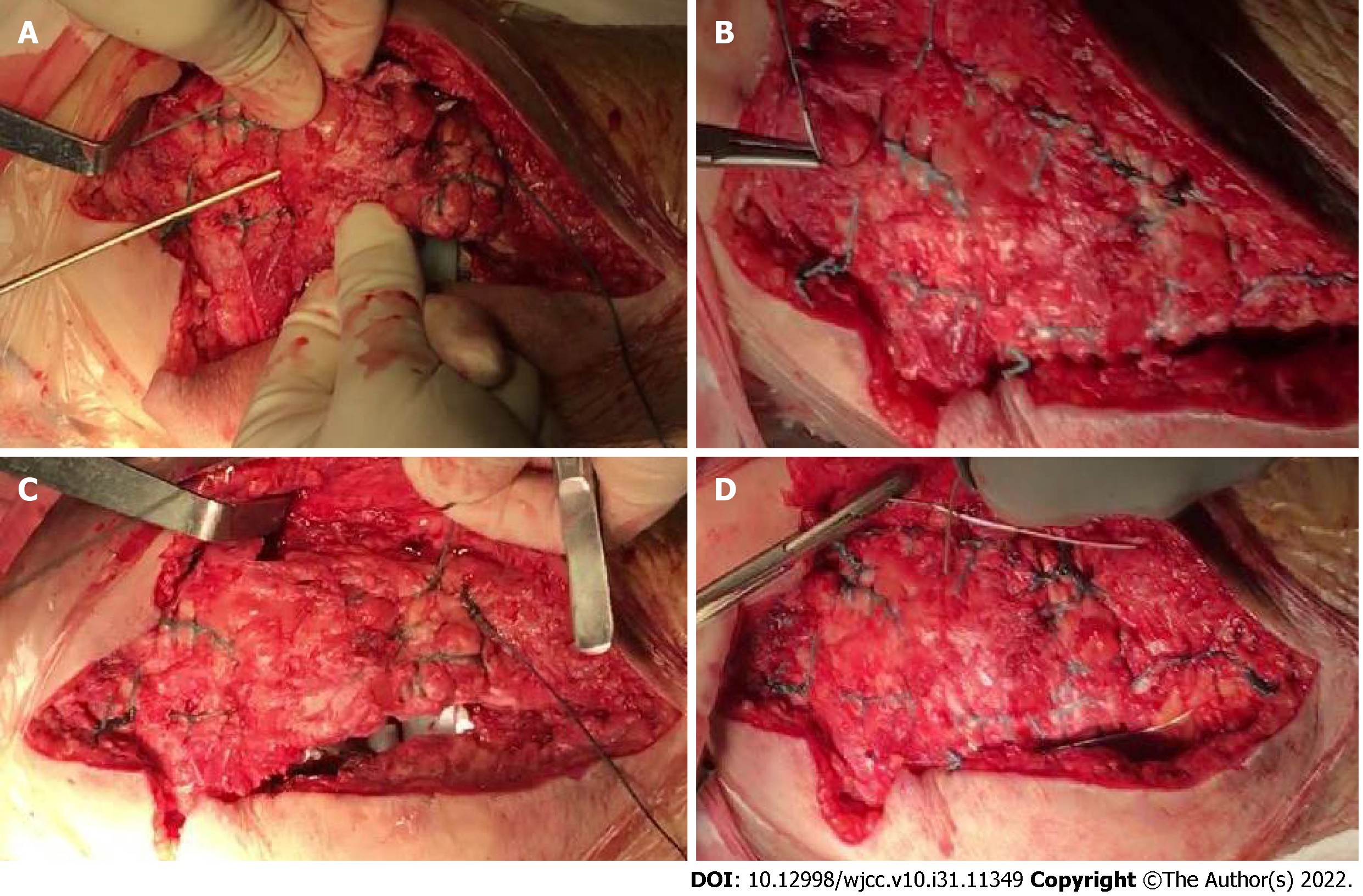
Patients were positioned supine on the operating table. An anterior midline incision, generally through or excising the prior surgical scar, was made, and medial and lateral fasciocutaneous flaps were raised, exposing the EM. Devitalized tissue was debrided, and the patellar tendon was assessed. Two longitudinal tunnels were drilled in the patella using a 3 mm drill. We used two No. 5 non-absorbable sutures running in a locked fashion on the medial and lateral aspect of the quadriceps tendon, then two sutures were passed through the two longitudinal patellar tunnels and sutured to the medial and lateral sides of the patellar tendon, and the patellar tendon rupture was sutured separately (Figure 1A and B), followed by suturing the joint capsule (Figure 1C). Finally, titanium cable was used to pass through the superior edge of the patella, while the distal end of the titanium cable needed to pass through the tibial tuberosity. The titanium cable was tightened to form a tension band, the titanium cable was fixed with cable clamps, and the excessive titanium cable was cut off (Figure 1D). The purpose of the titanium cable is to further reduce tension on the patellar tendon during postoperative knee movement. Titanium cable is generally removed 2-3 mo after operation. It is necessary to avoid prolonged indwelling of titanium cable, otherwise it may cause irritation to surrounding tissues and titanium cable fracture and limit the ROM of the knee joint, etc. In the process of stitching, the suture lines must be continuously tightened to ensure that the EM is still at a certain tension. All patients were immobilized with a brace for at least 6 wk and instructed to stay non-weight bearing, after that they were allowed to start partial weight bearing with passive and active physiotherapy[16].
Descriptive statistics are reported as the mean and standard deviation, as the mean and range, or as the number and percentage, as appropriate. Potential risk factors for these events included age, sex, and body mass index. All statistical tests were two-sided, the differences in variables were compared using the paired t test, and a P value < 0.001 was considered significant. Statistical analyses were performed using SPSS Version 25.0 software (IBM, Armonk, NY, United States).
Demographic and clinical data are summarized in Table 1. For all 12 patients who underwent direct repair for early patellar tendon rupture, ROM was 109.2° ± 10.6° preoperatively to 87.9° ± 11° postoperatively, average extensor lag was reduced from 30.2° ± 19.9° to 21° ± 18.1°, and mean WOMAC and HSS scores were 65.8 and 60.3 points, respectively (P < 0.001). Among these patients, the patient with the best recovery had a postoperative ROM of 112°, extensor lag of 0°, HSS score of 90, and WOMAC score of 6. However, the patient with the worst recovery had a postoperative ROM of 70°, extensor lag of 60°, HSS score of 35, and WOMAC score of 96. The complication rate was 25%: One (8.3%) patient with infection and two (16.7%) with re-rupture, all of whom underwent reoperation. The result of this direct repair method after early patellar tendon rupture showed poor outcomes at long-term follow-up. The postoperative patients had low ROM, accompanied by severe extension lag, and the incidence of postoperative complications was high.
| Variable | Value | P value |
| Age (yr) | 69.1 ± 7.4 (59-81) | |
| Gender (M/F) | 1/11 | |
| BMI (kg/m2) | 26.5 ± 2.7 (22.3-30.3) | |
| Number of surgeries per patient | 2-8 | |
| Complications | ||
| Infection | 1 (8.3%) | |
| Re-fracture | 2 (16.7%) | |
| WOMAC score | ||
| Post-operation | 65.8 ± 30.9 | |
| HSS scorePost-operation | 60.3 ± 21.7 | |
| Range of motion | < 0.001 | |
| Pre-operation | 109.2° ± 10.6° | |
| Post-operation | 87.9 ± 11° | |
| Extensor lagPre-operation | 30.2 ± 19.9 | < 0.001 |
| Post-operation | 21 ± 18.1 |
The patient with postoperative early patellar tendon rupture underwent primary knee arthroplasty because of right knee osteoarthritis, and underwent four operations because of postoperative complications after primary TKA. The patient suffered from patellar tendon rupture due to trauma, and was treated by suture anchor repair technique in another hospital (Figure 2A). However, a large amount of exudation occurred in the knee incision after operation, so open irrigation, debridement, and liner exchange were performed, but the knee was painful and had poor flexion. A few months later, the patient was treated by open reduction and the direct repair (Figure 2B). Unfortunately, the titanium cable in the knee joint was broken after 2 mo and the broken titanium cable punctured the skin to form a sinus (Figure 2C). To make matters worse, we found Streptococcus aureus in the patient's synovial fluid. After consideration, we performed revision TKA on the patient, and reconstructed the EM with Marlex mesh (Figure 2D). After operation, the knee joint was fixed with plaster for 6 wk, the ROM increased gradually, and the inflammatory indexes tended to be normal. For two patients with re-rupture after operation, we used the semitendinosus as autograft to reconstruct the EM. After operation, both patients achieved a good final outcome, with good ROM of the knee joint at the latest follow-up.
The most important findings of the present study were that the result of the direct repair method after early patellar tendon rupture showed poor outcomes at long-term follow-up. The postoperative patients had low ROM, accompanied by severe extension lag, and the incidence of postoperative complications was high. Previous studies were limited by the relatively small case number. We provided a more complete case series. Second, our study showed a low success rate of this direct repair and low patient satisfaction compared with other studies. We suggest that direct repair should not be the first choice for the treatment of early patellar tendon rupture.
Although the occurrence of patellar tendon rupture is rare, with a reported prevalence between 0.17%-1%[1]. Once happened, it would have a devastating impact on the patients' daily life after operation, and often resulted in frequent falls, difficulty in walking, and pain[17,18]. The treatment of EM disruption after TKA had remained a challenge for decades, and the ideal method of treatment remained unclear[19]. There have been few recent reports of direct repair after EM disruption in arthroplasty patients, except for those published in 2005 and 2018[10,20]. And the article published in 2005 specifically studied the quadriceps tendon. Our current case series provides an updated report about patellar tendon rupture.
Tracing back to the source, we found two reports about direct repair of EM disruption after TKA in earlier years. In 1987, Lynch et al[21] reported EM complications in 281 TKAs. Among these complications were eight EM disruptions. All of these complications occurred within 9 mo of the arthroplasty. Of the four patellar tendon ruptures that were directly repaired, one re-ruptured at 4 wk after the operation, two had residual extensor lags of 18° and 22°, and one became infected. The failure rate of direct repair of EM disruption was 50%, the average residual extensor lag in successful cases was 17.8°, and the knee flexion was 70°. In 1989, Rand et al[22] reported EM complications in 16 TKAs, all of which were repaired directly except three cases. Of the nine patella tendon ruptures treated by direct repair, all nine failed with six re-rupturing after the operation and three became infected. The mean interval from the last TKA to diagnosis of rupture was 7 mo (range, 0 to 42 mo). The failure rate of direct repair of EM disruption was 85%, the mean ROM was extension of -22° (range, 0" to -35") and flexion of 86" (range, 30" to 145"). The results from the studies of Lynch et al[21] and Rand et al[22] showed equally severe knee extensor lag and poor ROM compared to our current study.
In the report of Courtney et al[10], 19 patients with patella tendon ruptures underwent direct repair. The reoperation rate was 53%, the mean preoperative extensor lag was 11.7° and the mean postoperative extensor lag was 5.5°, the mean preoperative flexion was 106.0 and the mean postoperative flexion was 103.5°, and the mean postoperative Knee Society score was 106.6. Although the postoperative ROM of the patients in this report was high, there was no significant improvement compared with that before operation, and the incidence of complications was still very high. Reconstruction with EM allografts has been proposed as an alternative treatment for disruption of the EM in cases of chronic injury or poor tissue quality that would preclude direct repair. However, their data suggest that there is no difference in outcomes between the direct repair and allograft reconstruction groups.
In our research, the failure rate of direct repair was 25%, the average residual extensors lag in cases was 21°, average knee flexion was 87.9°, and the mean WOMAC and HSS scores were 65.8 and 60.3 points, respectively. Combined with the above reports, the postoperative ROM decreased or had hardly changed compared with that before operation, and the motion was limited. What's more serious was that there was severe knee extension lag, which will seriously affect the knee joint function. The high incidence of postoperative complications also greatly increased the failure rate of surgery, and the postoperative scores showed poor recovery. It was far from enough to meet the patients' normal daily life after operation. Judging from these results, the result of direct repair is not satisfactory.
In addition to direct repair, there were other multiple surgical options for EM disruption, including reconstruction with allograft, autograft, and synthetic material[23]. There was no consensus in the report as to the type of EM reconstruction that yields the best results. At present, more and more evidence proved that the therapeutic effect of direct repair was unsatisfactory, which made us have to compare it with other treatments, in order to judge whether there is a better treatment.
Allograft augmentation had been considered the gold standard with multiple reports[13,14]. In the report of Wise et al[24], 16 patients with 17 reconstructions (10 patellar tendons, 7 quadriceps tendons) were treated with achilles tendon allograft. All patients underwent evaluation at an average of 45.7 mo. After reconstruction, the average extensor lag was 6.6° and average knee flexion was 105.1°, the extensor lag (6.6° vs 21°) was significantly lower, and the knee flexion(105.1° vs 87.9°) was significantly higher than ours. In addition to allograft, we found an up-to-date literature on synthetic material. Besides, monofilament polypropylene mesh has emerged as the preferred treatment[9]. In the report of Buller et al[9], 30 patients were treated with Marlex mesh. The failure rate of the operation was 27%. Of the successful EM reconstructions, extensor lag improved by a mean of 34°, with the average final lag measuring 9° ± 8°, the average final active ROM was 9° to 107 ± 15 degrees of flexion. The extensor lag (9° ± 8° vs 21° ± 18.1°) was significantly lower and the knee flexion (107 ± 15° vs 87.9 ± 11°) was significantly higher than ours. Similar results were found in comparison with the literature on autograft, where postoperative ROM and the extensor lag were better than those with direct repair[25]. Patellar tendon reconstruction with autologous hamstring tendon graft allows for acceptable outcomes in the setting of patellar tendon disruption when direct repair is not possible[26].
In clinical practice, an extended knee fixation period of 4 wk must be performed after patellar tendon rupture to allow wound and tissue healing. Depending on the type of reconstruction performed and patient-related factors, weight-bearing limitations may range from nonweight-bearing to partial weight-bearing[27]. Some studies argued that immobilisation of the knee for 4 or 8 wk could generate postoperative stiffness with adherence and arthrofibrosis[28,29]. Therefore, some studies have proposed early rehabilitation after 4 wk, but there is no evidence of superiority of a protocol over another. Based on available data, the postoperative rehabilitation regimen does not influence extensor lag and ROM at follow-up, although early mobilisation has been reported to be associated with a greater knee flexion range at follow-up[27].
There were several limitations to this study, including its retrospective design. A limitation of our study was the small number of cases due to the low incidence of early patellar tendon rupture. We present the largest series to our knowledge. The operative reports were also not consistent in commenting on the quality of the tissues and the characteristics of the rupture.
After comparison with these reports, no matter whether we choose allograft, autograft, or synthetic material to reconstruct the EM, the result of direct repair is not as ideal as that of these treatments. And direct repair had the severe extensor lag after operation, which will have a great impact on the postoperative function of the patients. After the failure of direct repair, these reconstruction methods can also be used as remedial measures. Just like the three patients who failed after operation in our cases, they received semitendinosus reconstruction and Marlex mesh reconstruction respectively, and all the patients recovered well after operation.
The direct repair method for early patella tendon rupture showed unsatisfactory clinical results in this group of patients, and it was actually ineffective for the recovery of knee joint function in patients. More and more new surgical techniques had also shown better clinical results. Therefore, we suggested that direct repair should not be the preferred method to treat early patella tendon rupture, but other reconstruction methods should be boldly chosen. Our experience would be instructive for clinicians to treat early patella tendon rupture.
Patellar tendon rupture after total knee arthroplasty (TKA) is a catastrophic complication.
There has been no unified treatment for early patella tendon rupture after TKA, and long-term follow-up data are lacking. The purpose of this study was to introduce a direct repair method for early patella tendon rupture following TKA and determine the clinical outcomes and complications of this method.
To compare the results to similar studies to summarize potential advantages and disadvantages.
We retrospectively reviewed the medical records of all patients who underwent TKA from 2008 to 2021 and were eligible for inclusion in this study. Patients with early patellar tendon rupture after TKA were included.
For all the 12 patients who underwent direct repair for early patellar tendon rupture, three patients failed: One (8.3%) for infection and two (17.6%) for re-fracture. The two patients with re-fracture both underwent reoperation to reconstruct the extensor mechanism and the patient with infection underwent revision surgery.
This direct repair method for early patellar tendon rupture is not an ideal therapy.
We suggested that direct repair should not be the preferred method to treat early patella tendon rupture, but other reconstruction methods should be boldly chosen.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bagaria V, India; Koumantakis GA, Greece; Oommen AT, India S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Bonnin M, Lustig S, Huten D. Extensor tendon ruptures after total knee arthroplasty. Orthop Traumatol Surg Res. 2016;102:S21-S31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 2. | Cottino U, Abdel MP, Hanssen AD. Chronic extensor mechanism insufficiency in total knee arthroplasty (TKA). Curr Rev Musculoskelet Med. 2015;8:368-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Goldstein ZH, Yi PH, Haughom BD, Hellman MD, Levine BR. Bilateral extensor mechanism disruption after total knee arthroplasty in two morbidly obese patients. Orthopedics. 2015;38:e443-e446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Seng C, Lim YJ, Pang HN. Spontaneous disruption of the bilateral knee extensor mechanism: a report of two cases. J Orthop Surg (Hong Kong). 2015;23:262-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Vajapey SP, Blackwell RE, Maki AJ, Miller TL. Treatment of Extensor Tendon Disruption After Total Knee Arthroplasty: A Systematic Review. J Arthroplasty. 2019;34:1279-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 6. | Lim CT, Amanatullah DF, Huddleston JI 3rd, Harris AHS, Hwang KL, Maloney WJ, Goodman SB. Reconstruction of Disrupted Extensor Mechanism After Total Knee Arthroplasty. J Arthroplasty. 2017;32:3134-3140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Kim TW, Kamath AF, Israelite CL. Suture anchor repair of quadriceps tendon rupture after total knee arthroplasty. J Arthroplasty. 2011;26:817-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Cadambi A, Engh GA. Use of a semitendinosus tendon autogenous graft for rupture of the patellar ligament after total knee arthroplasty. A report of seven cases. J Bone Joint Surg Am. 1992;74:974-979. [PubMed] |
| 9. | Buller LT, Warth LC, Deckard ER, Meneghini RM. Extensor Mechanism Reconstruction Using Marlex Mesh: Is Postoperative Casting Mandatory? J Arthroplasty. 2020;35:3747-3753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Courtney PM, Edmiston TA, Pflederer CT, Levine BR, Gerlinger TL. Is There Any Role for Direct Repair of Extensor Mechanism Disruption Following Total Knee Arthroplasty? J Arthroplasty. 2018;33:S244-S248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Leopold SS, Greidanus N, Paprosky WG, Berger RA, Rosenberg AG. High rate of failure of allograft reconstruction of the extensor mechanism after total knee arthroplasty. J Bone Joint Surg Am. 1999;81:1574-1579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 102] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Nazarian DG, Booth RE Jr. Extensor mechanism allografts in total knee arthroplasty. Clin Orthop Relat Res. 1999;367:123-129. [RCA] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 68] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Springer BD, Della Valle CJ. Extensor mechanism allograft reconstruction after total knee arthroplasty. J Arthroplasty. 2008;23:35-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Brown NM, Murray T, Sporer SM, Wetters N, Berger RA, Della Valle CJ. Extensor mechanism allograft reconstruction for extensor mechanism failure following total knee arthroplasty. J Bone Joint Surg Am. 2015;97:279-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 70] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 15. | Burnett RS, Butler RA, Barrack RL. Extensor mechanism allograft reconstruction in TKA at a mean of 56 months. Clin Orthop Relat Res. 2006;452:159-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Rosa B, Campos P, Barros A, Karmali S, Gonçalves R. Spontaneous bilateral patellar tendon rupture: case report and review of fluoroquinolone-induced tendinopathy. Clin Case Rep. 2016;4:678-681. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Barrack RL, Stanley T, Allen Butler R. Treating extensor mechanism disruption after total knee arthroplasty. Clin Orthop Relat Res. 2003;98-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 64] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Emerson RH Jr, Head WC, Malinin TI. Reconstruction of patellar tendon rupture after total knee arthroplasty with an extensor mechanism allograft. Clin Orthop Relat Res. 1990;260:154-161. [RCA] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 98] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Nam D, Abdel MP, Cross MB, LaMont LE, Reinhardt KR, McArthur BA, Mayman DJ, Hanssen AD, Sculco TP. The management of extensor mechanism complications in total knee arthroplasty. AAOS exhibit selection. J Bone Joint Surg Am. 2014;96:e47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Dobbs RE, Hanssen AD, Lewallen DG, Pagnano MW. Quadriceps tendon rupture after total knee arthroplasty. Prevalence, complications, and outcomes. J Bone Joint Surg Am. 2005;87:37-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Lynch AF, Rorabeck CH, Bourne RB. Extensor mechanism complications following total knee arthroplasty. J Arthroplasty. 1987;2:135-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 231] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 22. | Rand JA, Morrey BF, Bryan RS. Patellar tendon rupture after total knee arthroplasty. Clin Orthop Relat Res. 1989;233-238. [RCA] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 46] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Papalia R, Vasta S, D'Adamio S, Albo E, Maffulli N, Denaro V. Complications involving the extensor mechanism after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23:3501-3515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Wise BT, Erens G, Pour AE, Bradbury TL, Roberson JR. Long-term results of extensor mechanism reconstruction using Achilles tendon allograft after total knee arthroplasty. Int Orthop. 2018;42:2367-2373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 25. | Lamberti A, Balato G, Summa PP, Rajgopal A, Vasdev A, Baldini A. Surgical options for chronic patellar tendon rupture in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018;26:1429-1435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 26. | Friedman JM, You JS, Hodax JD, Aung MS, Feeley BT, Zhang AL, Ma CB, Lansdown DA. Patellar tendon reconstruction with hamstring autograft for the treatment of chronic irreparable patellar tendon injuries. Knee. 2020;27:1841-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | De Franco C, de Matteo V, Lenzi M, Marano E, Festa E, Bernasconi A, Smeraglia F, Balato G. The active knee extension after extensor mechanism reconstruction using allograft is not influenced by "early mobilization": a systematic review and meta-analysis. J Orthop Surg Res. 2022;17:153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Cheuy VA, Foran JRH, Paxton RJ, Bade MJ, Zeni JA, Stevens-Lapsley JE. Arthrofibrosis Associated With Total Knee Arthroplasty. J Arthroplasty. 2017;32:2604-2611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 168] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 29. | González Della Valle A, Leali A, Haas S. Etiology and surgical interventions for stiff total knee replacements. HSS J. 2007;3:182-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |