Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.830
First decision: November 6, 2021
Revised: November 19, 2021
Accepted: December 25, 2021
Article in press: December 25, 2021
Published online: January 21, 2022
Processing time: 166 Days and 9.8 Hours
Intussusception can be managed by pneumatic reduction, ultrasound-guided hydrostatic reduction, open or laparoscopic surgery, but laparoscopy in such cases remains controversial.
To explore the clinical characteristics, effectiveness, and complications of surgical reduction for intussusception using laparoscopy in children.
This study was a retrospective case series of pediatric patients with intussusception who underwent surgical reduction by laparoscopy from May 2011 to April 2016 at Taizhou Hospital of Zhejiang Province. Clinical characteristics (operation time, intraoperative blood loss, conversion rate of laparotomy, reasons for conversion, postoperative hospital stay, and adverse events) were described.
The 65 patients included 45 boys and 20 girls. The average age was 2.3 years (27.5 ± 24.5 mo). Of the 65 patients, 61 underwent surgical reduction by laparoscopy after a failed enema reduction of intussusception, and four underwent the procedure directly. All patients were treated successfully and 57 (87.7%) patients underwent successful laparoscopic surgery, two of which had a spontaneous reduction. Among the remaining cases, one was converted to open surgery via right upper quadrant incision, and seven required enlarged umbilical incisions. Intestinal resection was performed in 5 patients because of abnormal bowel lesions. There were no complications (intestinal perforations, wound infections, or intestinal adhesions) during the follow-up of 3 years to 8 years. Two patients experienced a recurrence of intussusception; one was resolved with pneumatic reduction, and the other underwent a second laparoscopic surgery.
Laparoscopic approach for pediatric intussusception is feasible and safe. Bowel resection if required can be performed by extending umbilical incision without the conventional laparotomy.
Core Tip: This study aimed to explore the clinical characteristics, effectiveness, and complications of surgical reduction for intussusception using laparoscopy in children. Laparoscopic intussusception reduction can be beneficial and without significant complications if well indicated, and if an extension of the umbilical incision is used if needed. Laparoscopic assistance can also yield good treatment outcomes in some complicated cases requiring intestinal resection.
- Citation: Li SM, Wu XY, Luo CF, Yu LJ. Laparoscopic approach for managing intussusception in children: Analysis of 65 cases. World J Clin Cases 2022; 10(3): 830-839
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/830.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.830
For intussusception, the laparoscopic approach is a feasible alternative when pneumatic reduction or ultrasound-guided hydrostatic reduction failure. Laparoscopic intussusception reduction can be beneficial and without significant complications if well indicated, and an extension of the umbilical incision is used if needed. Laparoscopic assistance can also yield good treatment outcomes in some complicated cases requiring intestinal resection. Next, we can take the results of this study as a starting point for further prospective multicenter cohort studies.
Intussusception can be managed by laparoscopic surgery, but it remains controversial. The results of this study strongly suggest that intussusception reduction using the laparoscopic approach is effective and without complications in patients with complex conditions or those requiring bowel resection.
Laparoscopy has been reported to be effective and without major complications for the management of intussusception[1,2], supporting the present study. In the present study, the success rate of laparoscopy was 88%, which is within the 79%-90% range reported by many case series[1-3]. Nevertheless, the use of laparoscopy remains controversial because laparoscopic intussusception reduction has a high rate of conversion to laparotomy, as high as 70% in some reports[4]. Nevertheless, with the improvement of laparoscopic techniques in recent years, the conversion rate of laparoscopic intussusception reduction to laparotomy has decreased from 14.3% to 5.4%[5,6]. In this study, the overall conversion rate to open laparotomy was 12%, including seven patients with extension of the umbilical incision. Considering that the small transverse umbilical incision is concealed, it is more aesthetically appealing than traditional open surgery. Besides, laparoscopically-assisted surgery can be considered a form of minimally invasive surgery with laparoscopic assistance; thus, there was only one case of true conversion to open surgery, resulting in a rate of conversion to open surgery of only 1.5%.
It has been reported that patients over 3 years of age have a higher probability of intestinal resection[7,8]; for these patients, laparoscopic intussusception reduction surgery is not recommended[9]. In this study, two patients were > 3 years of age, in whom intussusception was diagnosed using preoperative B-mode ultrasound. Considering the patients’ age, there was a possibility of intestinal lesions, and laparoscopic surgery was performed directly. After reduction was completed, erosion was found in the terminal ileum in one patient, and the tissue was frozen and rapidly sent for pathological examination, revealing lymphoma. The umbilical incision was extended to remove the diseased tissue and the ileocecal segment. The patient recovered after chemotherapy, and the incision site maintained a good aesthetic appearance. It was also reported that laparoscopic reduction is not recommended for patients aged < 3 mo[7,8]. In this study, one 1-month-old patient underwent difficult laparoscopic reduction, and the umbilical incision had to be extended. It was found that the terminal ileum had duplication malformations that were managed with intestinal resection and anastomosis. With the improvement of laparoscopic techniques and instrumentation, we believe that laparoscopic surgery will not be contraindicated by age or intestinal resection because minimally invasive surgery through a small umbilical incision can be achieved even for intestinal resection[1-3].
Another major controversy involves the fact that laparoscopic intussusception reduction is associated with a higher recurrence rate than is conventional open surgery. Nevertheless, it was recently reported that the recurrence rate after laparoscopic intussusception was 3.4%[6]. In this study, there were two recurrences (3.1%), nearly the same as traditional open surgery[10]. The ileum's seromuscular layers and the ascending colon were repaired with two sutures, and the terminal ileum and the ascending colon were juxtaposed. If the ileocecal segment was relatively isolated, it was fixed to the lower right abdominal wall with two sutures to prevent relapse. The recurrence rate in our cohort of only 3.1% suggests good effectiveness. One patient experienced recurrence and required re-operation. The original fixation suture was found to be loose and was re-fixed, without subsequent recurrence. In our opinion, intestine fixation to the abdominal wall may be an effective method for intussusception. Although this method of intestine fixation to the abdominal wall has not occurred intestinal torsion in this stuty, but we do not know whether it is a risk factor for intestinal torsion. Therefore, we need longer follow-up time and more cases.
It has been reported that the appendix is also a site susceptible to intussusception[4]. The appendix is prone to becoming a lead point for intussusception because of viral or bacterial infection or abnormal anatomical position. Therefore, when intussusception is found in the appendix during operation, the appendix exhibiting congestion and swelling is resected. There were no recurrences after appendicular resection in this study. Besides, there were no complications in our cohort, such as intestinal adhesions, wound infections, and intestinal perforations, as supported by the low rates of complications observed in previous studies[2,4].
The short operative time and hospital stay reflect the advantages of laparoscopic techniques[5,6]. Besides, laparoscopic techniques have obvious advantages for intussusception reduction. First, owing to muscle relaxation after anesthesia, some of the intussuscepted intestines might resolve spontaneously. Second, laparoscopic surgery can more intuitively locate organic lesions such as lymphomas of the terminal ileum and intestinal polyps. With open surgery, only the intussusception at the diverticulum's distal end might have been discovered, and the intussusception of the diverticulum itself might have been missed. Nevertheless, laparoscopy might also have some disadvantages, mainly related to the small abdominal cavity in children and the significant amount of edema in intussusception. First, if the intra-abdominal pressure is too high, the cardiopulmonary function of the patient will be affected. If it is too low, the operating field will be too small. Second, given the abdominal cavity's limited space, a gastric tube could be placed before surgery. Third, intussusception masses are often found in the upper right abdomen because the appendix is sometimes involved. Therefore, searching along the terminal ileum and the appendix is more difficult. Fourth, during reduction, the right-hand grasping forceps pulls the neck of the intussuscepted ileum along the fan-shaped curvature of the mesentery, while the left-hand grasping forceps pulls the neck of the intussuscepted sheath to the opposite direction; in this way, the two forces are maintained in the fan-shaped curvature of the mesentery. If the directions of the two forces are along a straight line, the traction on the mesentery tends to be insufficient. In addition, in the reduced intestine, it is important to change the two forceps' positions at an appropriate time to maintain some tension between the two forces. Finally, if it is found that the intussusception is challenging to reduce by laparoscopy, the umbilical incision should be extended, and the reduction should be performed through the umbilical incision. If necessary, bowel resection should be performed. Although laparoscopic intussusception reduction has many advantages, there are specific contraindications. First, laparoscopic surgery should not be performed in cases with longer times of onset (especially > 48 h), instability of the respiratory or circulatory systems, intestinal perforation, peritonitis, severe abdominal distension, or other manifestations. Second, the intussusceptum ideally should not extend past the middle segment of the transverse colon. Those advantages and disadvantages have been highlighted in previous studies[2,4-6], but this study innovates by indicating that the umbilical excision can be enlarged when laparoscopy is difficult, without the need to convert the surgery to a true open surgery.
This study has limitations. The sample size was relatively small and from a single center. A treatment bias might be observed due to local practices. The retrospective nature of the study prevented the observation of some variables. Prospective multicenter cohort studies should be performed in the future.
During the study period, laparoscopic intussusception reduction was performed in 65 patients (Table 1). There were 45 (69.2%) boys and 20 (30.8%) girls, of whom the youngest was 1 mo old, and the oldest was 13 years old, and the average age was 2.3 years (27.5 ± 24.5 mo). The clinical presentations included paroxysmal crying or abdominal pain in 60 cases. There was an abdominal mass in 45 patients, and jam-colored bowel movements in 48 patients. The time of onset was 26.3 ± 7.8 h and was within 48 h in 64 cases and up to 52 h in one patient. Sixty (92.3%) had primary intussusception. Among all patients, three (4.6%), 40 (61.5%), and 22 (33.9) had ileum, ascending colon, and transverse colon involvement, respectively. Nine (13.8%) patients had acute gastroenteritis, seven (10.8%) had respiratory infection, and one (1.5%) had urinary tract infection. Six (9.2%) were taking probiotics, eight (12.3%) proton pump inhibitors, 13 (20.0%) antibiotics, and four (6.2%) gastrointestinal motility drugs.
| Characteristic | Total (n = 65) |
| Age, means ± SD (range) | 27.5 ± 24.5 mo (1 mo-13 yr) |
| Sex, n (%) | |
| Male | 45 (69.2) |
| Female | 20 (30.8) |
| Time of onset, h, means ± SD | 26.3 ± 7.8 |
| Clinical presentations, n (%) | |
| Paroxysmal crying or abdominal pain | 60 (92.3) |
| Abdominal mass | 45 (69.2) |
| Jam-colored bowel movements | 48 (73.8) |
| Type of intussusception, n (%) | |
| Primary | 60 (92.3) |
| Secondary | 5 (7.7) |
| Level of intussusceptum, n (%) | |
| Ileum | 3 (4.6) |
| Ascending colon | 40 (61.5) |
| Transverse colon | 22 (33.9) |
| Descending colon | 0 |
| Comorbidities, n (%) | |
| Acute gastroenteritis | 9 (13.8) |
| Respiratory infection | 7 (10.8) |
| Urinary tract infection | 1 (1.5) |
| Medication, n (%) | |
| Probiotics | 6 (9.2) |
| Proton pump inhibitor | 8 (12.3) |
| Antibiotics | 13 (20.0) |
| Gastrointestinal motility | 4 (6.2) |
Of the 65 patients, laparoscopic reduction surgery was completed in 57 (87.7%) (Table 2). For two (3.1%) patients, laparoscopy revealed that the intussusception had spontaneously resolved. Among the other 8 patients, one patient's intussusceptum was found to have extended past the middle segment of the transverse colon. The mass was large and challenging to reduce under laparoscopy, and the procedure was directly converted to a transverse incision in the right upper abdomen to complete the operation; the operation of the other seven patients was completed with an extension of the umbilical incision. Among them, five (7.7%) patients had abnormal bowel lesions, one (1.5%) had intestinal necrosis, and one (1.5%) had severe bowel nesting. Postoperative pathological findings indicated two patients with lymphoma of the terminal ileum, one patient with Meckel’s diverticulum, one patient with small intestinal duplication, and one patient with small intestine polyps. There were 15 with appendicular intussusception among all patients, in which the appendixes exhibited congestion and swelling and were resected. The average operative time was 42.2 ± 12.2 min. All patients were discharged uneventfully, and the hospital stays were 3-12 d, with an average of 4.5 d (4.5 ± 1.3). The intraoperative blood loss was 2.2 ± 1.6 mL.
| Characteristic | Total (n = 65) |
| Operation time, min, means ± SD | 42.2 ± 12.2 |
| Intraoperative blood loss, mL, means ± SD | 2.2 ± 1.6 |
| Conversion rate of laparotomy, n (%) | 8 (12.3) |
| With a transverse incision in the right upper abdomen | 1 (1.5) |
| With an extension of the umbilical incision | 7 (10.8) |
| Reasons for conversion, n (%) | |
| Abnormal bowel lesions | 5 (7.7) |
| Intestinal necrosis | 1 (1.5) |
| Severe bowel nesting | 1 (1.5) |
| Postoperative pathology, n (%) | |
| Lymphoma of the terminal ileum | 2 (3.0) |
| Meckel’s diverticulum | 1 (1.5) |
| Small intestinal duplication | 1 (1.5) |
| Small intestine polyps | 1 (1.5) |
| Intraoperative appendectomy | 15 (23.1) |
| Postoperative hospital stay, d, means ± SD | 4.5 ± 1.3 |
| Postoperative complications, n (%) | |
| Intestinal adhesion, intestinal obstruction | 0 |
| Infection of incision | 0 |
| Intussusception recurred | 2 (3.0) |
The follow-up period ranged from 3 years to 8 years. There were no complications, such as intestinal adhesions, wound infections, or intestinal perforations. There were two cases of recurrent intussusception, one of which was resolved with pneumatic reduction, and one underwent a second laparoscopic surgery.
This study was a retrospective case series of pediatric patients with intussusception who underwent surgical reduction by laparoscopy from May 2011 to April 2016 at the Department of Pediatric Surgery of Taizhou Hospital of Zhejiang Province. The cases in this study were consecutive cases and were operated by the same surgical team. The study was approved by the ethics committee of Taizhou Hospital. The committee waived the requirement for informed consent because of the study's retrospective nature. The indications for laparoscopic surgery: (1) Diagnosed with intussusception by B-mode ultrasound[11]; (2) Unsuccessful gaseous enema reduction; (3) Organic lesions are highly suspected; and (4) Repeated intussusception times were more than three times within 1 wk.
The contra-indications for laparoscopic surgery: (1) Children with high abdominal distension and pneumoperitoneum could not be established; (2) Patients with abnormal cardiopulmonary functions and unable to tolerate pneumoperitoneum; or (3) The intussusception was large, and its head exceeded the middle section of the transverse colon. The cases in this study were consecutive cases and were operated by the same surgical team.
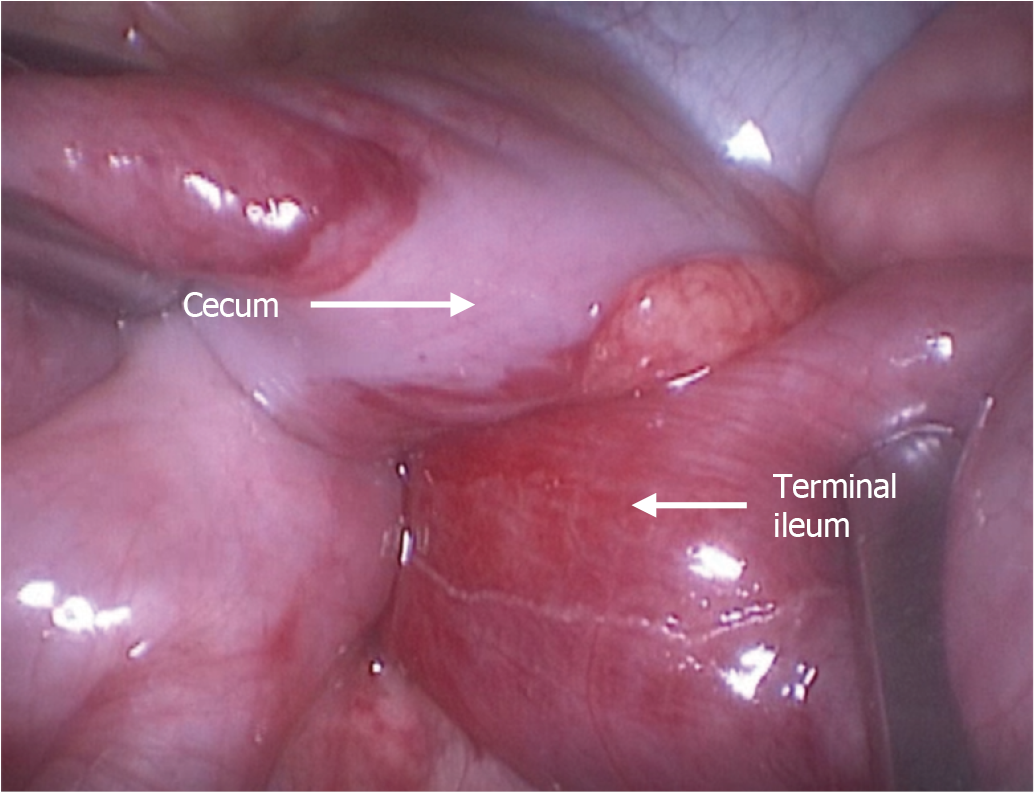
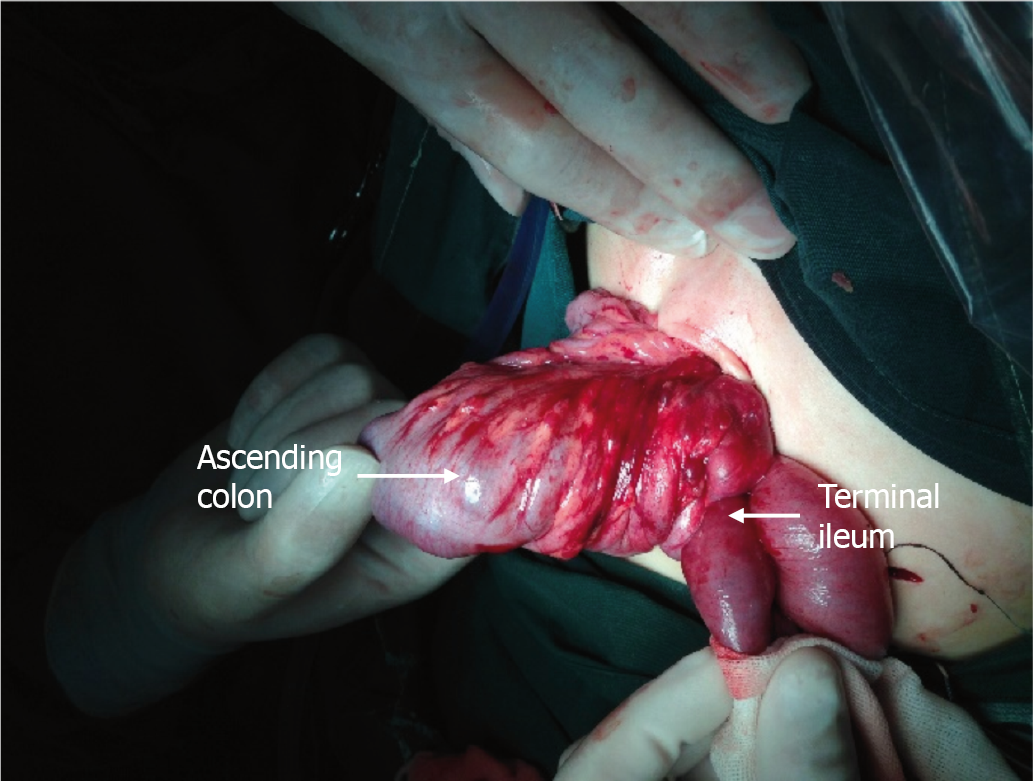
Routine blood tests, electrolyte tests, and blood gas analyses were performed before surgery. Before the operation, a gastric tube and an indwelling catheter were placed when ity was considered necessary. General anesthesia by tracheal intubation was used in all cases. The patient was positioned with the head downward and tilted to the left to expose the ileocecal segment of the intestine fully. The operator was positioned on the left side of the patient. An incision of 0.5-1.0-cm in length was made at the lower margin of the umbilicus. A trocar was placed under direct vision. CO2 was slowly injected, and the pressure was maintained at 8-12 mmHg. A 0° laparoscope was placed, 5-mm trocars were inserted in the lower right abdomen and the lower left abdomen under laparoscopic monitoring, and minimally invasive grasping forceps were placed. First, we find the hepatic segment of the transverse colon below the liver, and then find the intussusception along its proximal direction. With the right hand, the ileum's neck was grasped with the grasping forceps and pulled outward, paying attention to pull along the fan-shaped curvature of the mesentery. With the left hand, the intussuscepted sheath's neck was pulled in the opposite direction (Figure 1). Based on the length of the reduced intestine, the positions of the two grasping forceps were changed appropriately so that the two forces maintained some tension and were in the mesentery's curvature. The neck of the intussuscepted mass was frequently tight, and the left-hand forceps were used to open the neck of the outer sheath, while the right-hand forceps were used to pull the neck of the intussuscepted ileum so that some of the fluid in the neck could be drained. Simultaneously, part of the mesenteric tissue was pulled outward so that the neck was relatively loose and easy to reduce. After reduction, the intestines were examined for necrosis and other organic lesions. If none were found, the ileum's seromuscular layer and the ascending colon were repaired with two sutures. If the ileocecal segment was relatively isolated, it was fixed to the lower right abdominal wall with two sutures. Appendectomy was performed depending on the condition of the appendicular blood supply and swelling. When there was a reduction with a single laparoscope were found to be complicated or organic lesions were present, the neck of the intussusception mass or the intestine with organic lesions was fixed with grasping forceps under laparoscopic monitoring, and then the umbilical incision was extended transversely. The intussusception mass was then pulled out of the umbilical incision for manual reduction or intestinal resection (Figure 2). After anesthesia and return to consciousness, the patients were transferred to the general pediatric surgical ward. They received conventional second-generation cephalosporin antibiotics (50-100 mg/kg/d), omeprazole injection (0.7 mg/kg/d), and intravenous fluids for 3-7 d. The patients began to eat and gradually returned to normal diet 1-5 d after the operation according to their condition.
The data of all patients were collected from the paper medical records of the Department of Pediatric Surgery of Taizhou Hospital of Zhejiang Province, including basic characteristics (age, sex, time of onset, type of intussusception, level of intussusceptum, comorbidities, and medication) and clinical characteristics (operation time, intraoperative blood loss, conversion rate of laparotomy, reasons for conversion, postoperative hospital stay, and adverse events).
The family members of all patients were followed until June 2019 by outpatient reexamination, telephone or Wechat contact at 1 wk, 1 mo, half a year and 1 year, respectively, to collect data including wound healing, diet, bowel movements, abdominal pain and vomiting, sleep, growth and development, etc. Follow-up was conducted by 3 practicing physicians with more than 5 years of clinical experience in pediatric surgery.
All data were analyzed using SPSS 19.0 for Windows (IBM, Armonk, NY, United States). The continuous data were tested for normal distribution using the Kolmogorov-Smirnov test; those meeting the normal distribution are presented as means ± SD; otherwise, they are presented as medians (ranges). The categorical data are presented as n (%). Descriptive statistics were used.
Intussusception is an invagination of a proximal segment of the intestine into a distal part of the intestine that may result in bowel obstruction, venous congestion, and bowel wall edema[12-15]. It is a common cause of acute abdominal emergency in infants and children. It is most common in infants and children aged 3 mo to 3 years, with a peak incidence between 5 and 9 mo of age[12,13,16]. The vast majority of cases are ileocolic, but small bowel to small bowel and colocolonic intussusceptions may also occur[12,13]. The incidence is 3-40 cases per 10000 live births in the United States of America, Europe, and Australia[7,14,17,18]. Typical clinical presentation of intussusception includes paroxysmal crying, vomiting, an abdominal sausage-like mass, and jam-like, bloody stool[8,12,13]. It is primarily diagnosed through medical history taking, physical examination, ultrasound, and computed tomography[8,12,13]. Pneumatic reduction and ultrasound-guided hydrostatic reduction are the most widely used methods for treating intussusception in children[12,13,16,19-21]. They have a success rate as high as 95%, but pneumatic reduction and ultrasound-guided hydrostatic reduction still fails in some intussusception cases[7,8], and such children will require surgical treatment.
In the past, conventional open surgery was the mainstream surgical treatment for intussusception[12,13,20,21]. However, conventional surgery is associated with significant trauma in children[12,13]. With the development of laparoscopic techniques, there have been increasingly more reports of successful laparoscopic treatment of intussusception, limiting the surgical trauma and allowing faster recovery[1,21]. Nevertheless, laparoscopic treatment for intussusception remains controversial because the port setting is challenging because of the small working space in infants and small children and because the affected segment may vary among children. Besides, the reported series are small.
Therefore, this retrospective study aimed to explore the clinical characteristics, effectiveness, and complications of surgical reduction for intussusception using laparoscopy in children. The results could provide additional data for the management of this condition.
Intussusception can be managed by pneumatic reduction, ultrasound-guided hydrostatic reduction, open or laparoscopic surgery. On the other hand, the use of laparoscopy in such cases remains controversial.
The use of laparoscopy in infants with intussusception could be less morbid for the patients.
To explore the clinical characteristics, effectiveness, and complications of surgical reduction for intussusception using laparoscopy in children.
This retrospective case series included pediatric patients with intussusception who underwent surgical reduction by laparoscopy from May 2011 to April 2016 at Taizhou Hospital of Zhejiang Province. The clinical characteristics (operation time, intraoperative blood loss, conversion rate of laparotomy, reasons for conversion, postoperative hospital stay, and adverse events) of the patients were described.
The study could include 65 patients (45 boys and 20 girls). They were 2.3 years (27.5 ± 24.5 mo). Of the 65 patients, 61 underwent surgical reduction by laparoscopy after a failed enema reduction of intussusception, and four underwent the procedure directly. All patients were treated successfully. Fifty-seven (87.7%) patients underwent successful laparoscopic surgery, two of which had a spontaneous reduction. Among the remaining cases, one was converted to open surgery via right upper quadrant incision, and seven required enlarged umbilical incisions. Intestinal resection was performed in five patients because of abnormal bowel lesions. There were no complications (intestinal perforations, wound infections, or intestinal adhesions) during the follow-up of 3 years to 8 years. Two patients experienced a recurrence of intussusception; one was resolved with pneumatic reduction, and the other underwent a second laparoscopic surgery.
Laparoscopic approach for pediatric intussusception is feasible and safe. Bowel resection if required can be performed by extending umbilical incision without the conventional laparotomy.
This study provides useful data for the management of infants with intussusception.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abraha M, Gupta R, Osorno JF S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Chang PC, Duh YC, Fu YW, Hsu YJ, Wei CH. Single-incision laparoscopic surgery for idiopathic intussusception in children: Comparison with conventional laparoscopy. J Pediatr Surg. 2019;54:1604-1608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Vilallonga R, Himpens J, Vandercruysse F. Laparoscopic treatment of intussusception. Int J Surg Case Rep. 2015;7C:32-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Song EJ, Nam SH. Feasibility of Laparoscopic Surgery for Intussusception in Pediatric Patients and Risk of Bowel Resection. J Minim Invas Surg. 2018;21:154-159. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Kao C, Tseng SH, Chen Y. Laparoscopic reduction of intussusception in children by a single surgeon in comparison with open surgery. Minim Invasive Ther Allied Technol. 2011;20:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Almaramhy HH. Laparoscopic reduction of intussusception in children: role in primary and revisional reduction after failed non-surgical therapies. Int J Health Sci (Qassim). 2011;5:71-78. [PubMed] |
| 6. | Wei CH, Fu YW, Wang NL, Du YC, Sheu JC. Laparoscopy vs open surgery for idiopathic intussusception in children. Surg Endosc. 2015;29:668-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Ko HS, Schenk JP, Tröger J, Rohrschneider WK. Current radiological management of intussusception in children. Eur Radiol. 2007;17:2411-2421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Waseem M, Rosenberg HK. Intussusception. Pediatr Emerg Care. 2008;24:793-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 133] [Article Influence: 7.8] [Reference Citation Analysis (1)] |
| 9. | van der Laan M, Bax NM, van der Zee DC, Ure BM. The role of laparoscopy in the management of childhood intussusception. Surg Endosc. 2001;15:373-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Kaiser AD, Applegate KE, Ladd AP. Current success in the treatment of intussusception in children. Surgery. 2007;142:469-75; discussion 475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 101] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. |
Endoscopic Surgery Group; Pediatric Surgery Society, Zhonghua Yixuehui [DOI: 10.
Endoscopic Surgery Group, Pediatric Surgery Society, |
| 12. | Loukas M, Pellerin M, Kimball Z, de la Garza-Jordan J, Tubbs RS, Jordan R. Intussusception: an anatomical perspective with review of the literature. Clin Anat. 2011;24:552-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Edwards EA, Pigg N, Courtier J, Zapala MA, MacKenzie JD, Phelps AS. Intussusception: past, present and future. Pediatr Radiol. 2017;47:1101-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 87] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 14. | Jiang J, Jiang B, Parashar U, Nguyen T, Bines J, Patel MM. Childhood intussusception: a literature review. PLoS One. 2013;8:e68482. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 189] [Article Influence: 15.8] [Reference Citation Analysis (1)] |
| 15. | Jain S, Haydel MJ. Child Intussusception. StatPearls. Treasure Island (FL) 2020. [DOI] [Full Text] |
| 16. | Applegate KE. Intussusception in children: evidence-based diagnosis and treatment. Pediatr Radiol. 2009;39 Suppl 2:S140-S143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 124] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 17. | Tate JE, Simonsen L, Viboud C, Steiner C, Patel MM, Curns AT, Parashar UD. Trends in intussusception hospitalizations among US infants, 1993-2004: implications for monitoring the safety of the new rotavirus vaccination program. Pediatrics. 2008;121:e1125-e1132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 90] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 18. | Buettcher M, Baer G, Bonhoeffer J, Schaad UB, Heininger U. Three-year surveillance of intussusception in children in Switzerland. Pediatrics. 2007;120:473-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 19. | Gluckman S, Karpelowsky J, Webster AC, McGee RG. Management for intussusception in children. Cochrane Database Syst Rev. 2017;6:CD006476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Charles T, Penninga L, Reurings JC, Berry MC. Intussusception in Children: A Clinical Review. Acta Chir Belg. 2015;115:327-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Kelley-Quon LI, Arthur LG, Williams RF, Goldin AB, St Peter SD, Beres AL, Hu YY, Renaud EJ, Ricca R, Slidell MB, Taylor A, Smith CA, Miniati D, Sola JE, Valusek P, Berman L, Raval MV, Gosain A, Dellinger MB, Somme S, Downard CD, McAteer JP, Kawaguchi A. Management of intussusception in children: A systematic review. J Pediatr Surg. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |