Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.811
Peer-review started: June 9, 2021
First decision: June 25, 2021
Revised: September 15, 2021
Accepted: December 22, 2021
Article in press: December 22, 2021
Published online: January 21, 2022
Processing time: 219 Days and 21.9 Hours
Management of retroperitoneal sarcoma (RPS) involving the iliac artery is challenging and requires the concerted efforts of multidisciplinary team (MDT) members during surgical treatment.
To summarize the clinicopathologic features of RPS involving the iliac artery and our retroperitoneal soft tissue tumor MDT surgical experience.
In this retrospective study, 15 patients with RPS involving the iliac artery who underwent surgery at our retroperitoneal soft tissue tumor center from July 2004 to June 2020 were analyzed. Statistical analyses were performed by Student’s t-test with SPSS 16.0.
Complete tumor resection (R0/R1) and iliac artery reconstruction were achieved in all 15 patients. All the operations were successful, with no serious complications or perioperative death. Resection with bilateral iliac artery reconstruction required a higher intraoperative blood transfusion volume than resection with unilateral iliac artery reconstruction. Recurrent cases were more likely to bleed and required a higher blood transfusion volume than primary cases. As of January 2021, 11 patients were alive, and 4 had died. Local recurrence occurred in two patients, one of whom developed liver metastasis.
Resection of RPS involving iliac vessels is feasible and effective when performed by MDT members. Iliac artery oncovascular resection and reconstruction are key to a successful operation. Adequate blood preparation is important for successful completion of surgery.
Core Tip: This is a retrospective study of retroperitoneal sarcoma involving the iliac artery. Fifteen patients underwent tumor resection (R0/R1) and iliac artery reconstruction from July 2004 to June 2020. Eleven patients were alive and four had died as of January 2021. Local recurrence occurred in two patients, one of whom developed liver metastasis. Resection with bilateral iliac artery reconstruction required a higher intraoperative blood transfusion volume than resection with unilateral iliac artery reconstruction. Oncovascular resection of the involved iliac artery and vessel reconstruction are pivotal for complete tumor resection. Adequate blood preparation is important to ensure surgical success.
- Citation: Li WX, Tong HX, Lv CT, Yang H, Zhao G, Lu WQ, Zhang Y. Management of retroperitoneal sarcoma involving the iliac artery: Single-center surgical experience. World J Clin Cases 2022; 10(3): 811-819
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/811.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.811
Retroperitoneal sarcomas (RPSs) are malignant tumors originating from mesenchymal tissue and are exceedingly rare entities, among which liposarcoma is the most common type, followed by leiomyosarcoma[1]. Solitary fibroma and invasive fibroma are uncommon RPS subtypes that may arise in any location, including the retroperitoneum. Surgical excision remains the main treatment for primary tumors and is also recommended for recurrent tumors[2]. Specifically, tumors in the unique anatomic location of the retroperitoneum, which involves important blood vessels and organs, require the concerted efforts of a multidisciplinary team (MDT) during surgical treatment. Studies have shown that the success and radical resection rates were higher and the local relapse rate was lower for patients treated by professional MDTs than for those treated in nonprofessional centers[3]. High-throughput MDT centers are key to ensuring the effectiveness of medical services and the desired patient outcomes.
RPSs, especially recurrent lesions, are more likely to invade blood vessels, and resection of these major vessels is necessary for complete oncological clearance. The most frequently involved vessels for RPS are iliac vessels. Dissociation and re
Since its establishment in 2009, our retroperitoneal soft tissue tumor MDT has been committed to the standardized treatment of RPSs and has accumulated considerable experience in the surgical treatment of major involved vessels. This paper summarizes the treatment of RPSs involving the iliac artery from July 2004 to June 2020 and illustrates the key steps in vascular reconstruction.
From July 2004 to June 2020, a total of 15 patients aged 12 to 73 years underwent RPS resection combined with iliac artery reconstruction. Patient data were retrospectively gathered in a retroperitoneal tumor database and analyzed. Clinical manifestations included abdominal pain (3 cases) and abdominal mass (5 cases). The other seven tumors were found during follow-up examination. Six cases were primary, and nine were recurrent (Table 1).
| Variable | No. of cases | Mean (range) |
| Sex (female vs male) | 8/7 | |
| Age (< 60 yr vs ≥ 60 yr) | 11/4 | 52 (12-73) |
| Histologic subtype | ||
| LPS | 8 | |
| LMS | 2 | |
| UPS | 2 | |
| Other | 3 | |
| Primary/recurrent | 9/6 | |
| Organs resected | 1.3 (0-4) | |
| Artery reconstruction type | ||
| Unilateral iliac artery | 10 | |
| Bilateral iliac artery | 5 | |
| IVC partial resection/transection | 2/1 | |
| Common/internal iliac vein ligation | 3/1 | |
| Volume of blood loss (mL) | 1700 (500-5000) | |
| Volume of transfused blood (mL) | 743 (0-3150) | |
| Postoperative vascular complications | 2 |
All patients underwent preoperative computed tomography (CT), CT angiography (CTA), or magnetic resonance imaging (MRI) to clarify the relationship between the tumor and important vessels in the abdominal or pelvic cavity. Most patients with recurrence underwent PET examination.
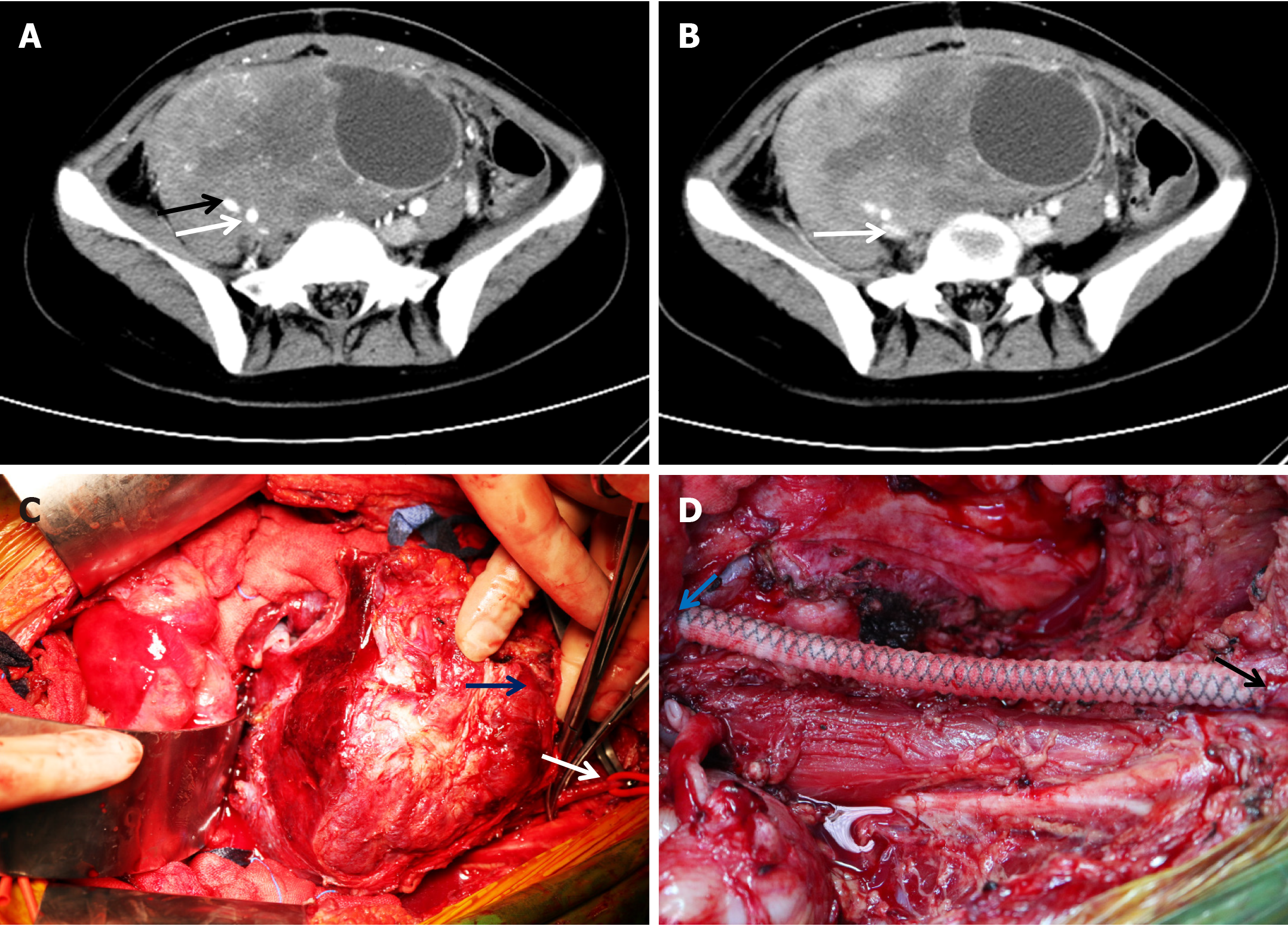
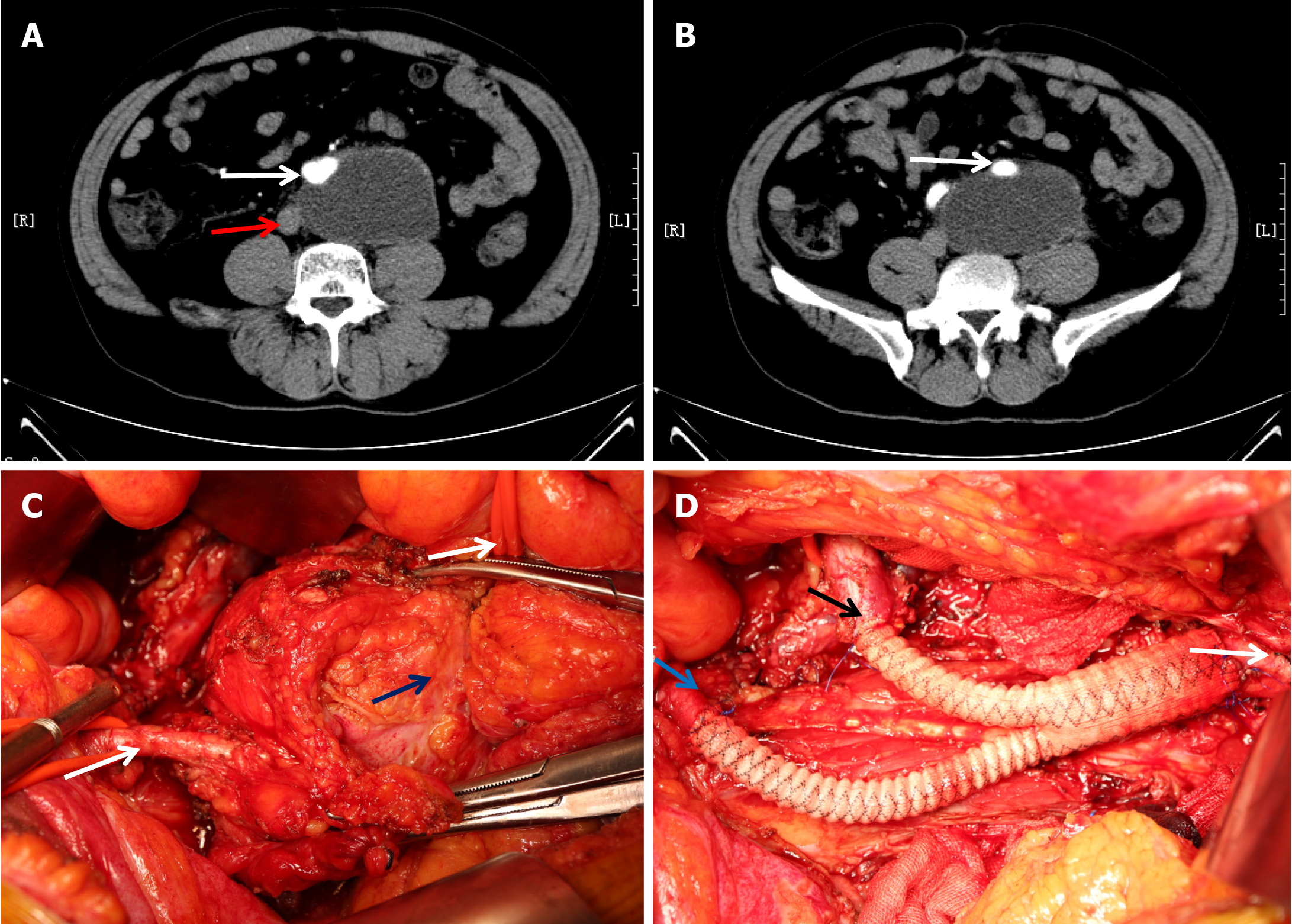
The incisions varied according to the location, size, and extent of the tumor. A median abdominal incision was usually adopted to facilitate exposure and incision extension, which could extend from the xiphoid process to the pubic symphysis. A lateral incision was added when necessary. In cases in which the mass encompassed the unilateral iliac artery and vein (Figure 1A and B), one side of the inguinal ligament was cut off, and the femoral artery was dissociated with a thin catheter to control bleeding during mass exposure (Figure 1C). The femoral and common iliac veins were ligated. The common iliac artery was isolated. Heparin was injected at 0.5 mg/kg body weight before vascular occlusion. After circulatory block, the femoral and common iliac arteries were cut off approximately 1 cm from the edge of the tumor, and the tumor was removed "en bloc" together with involved blood vessels and organs. Vessel reconstruction was completed between the common iliac artery and femoral artery (Figure 1D). In some cases, the mass encompassed the abdominal aorta and bilateral iliac arteries and adhered to the inferior vena cava (IVC) (Figure 2A and B). The abdominal aorta and left external iliac artery were fully exposed during mass exposure (Figure 2C). The right common iliac artery was further dissociated, and the left internal iliac artery was ligated. Resection was completed along with partial resection of the abdominal aorta and right common iliac artery and whole resection of the left common iliac artery. “Y-type” artificial vascular reconstruction was established among the abdominal aorta, right common iliac artery, and left external iliac artery (Figure 2D).
Statistical analyses were performed using SPSS software (v16.0, SPSS Inc., Chicago, IL, United States) and GraphPad Prism software (v5, GraphPad Software, San Diego, CA, United States). The mean and range were used for the analysis of variables. Differences between groups were analyzed using Student’s t-test for comparing means. P values < 0.05 were considered statistically significant.
All the surgeries were "en bloc" compartmental resections (R0/R1). Ten patients received unilateral iliac artery reconstruction, and five received bilateral iliac artery reconstruction (Table 1). A mean of 1.3 organs were excised, and the most commonly excised organ was the kidney. All the patients had good dorsalis pedis pulses postoperatively.
There were no perioperative deaths or infections of artificial vessels. One patient developed postoperative deep vein thrombosis in one leg after IVC transection during surgery, and no invasive treatment was performed. One patient developed external iliac artery occlusion 3 d after reconstruction. The condition improved after enhanced anticoagulant therapy. All the patients were discharged as scheduled. Pathology confirmed that there were eight cases of liposarcoma (LPS), two cases of leiomyosarcoma (LMS), two cases of undifferentiated pleomorphic sarcoma (UPS), and three cases of other types of tumors (solitary fibroma, invasive fibroma, and myxofibro
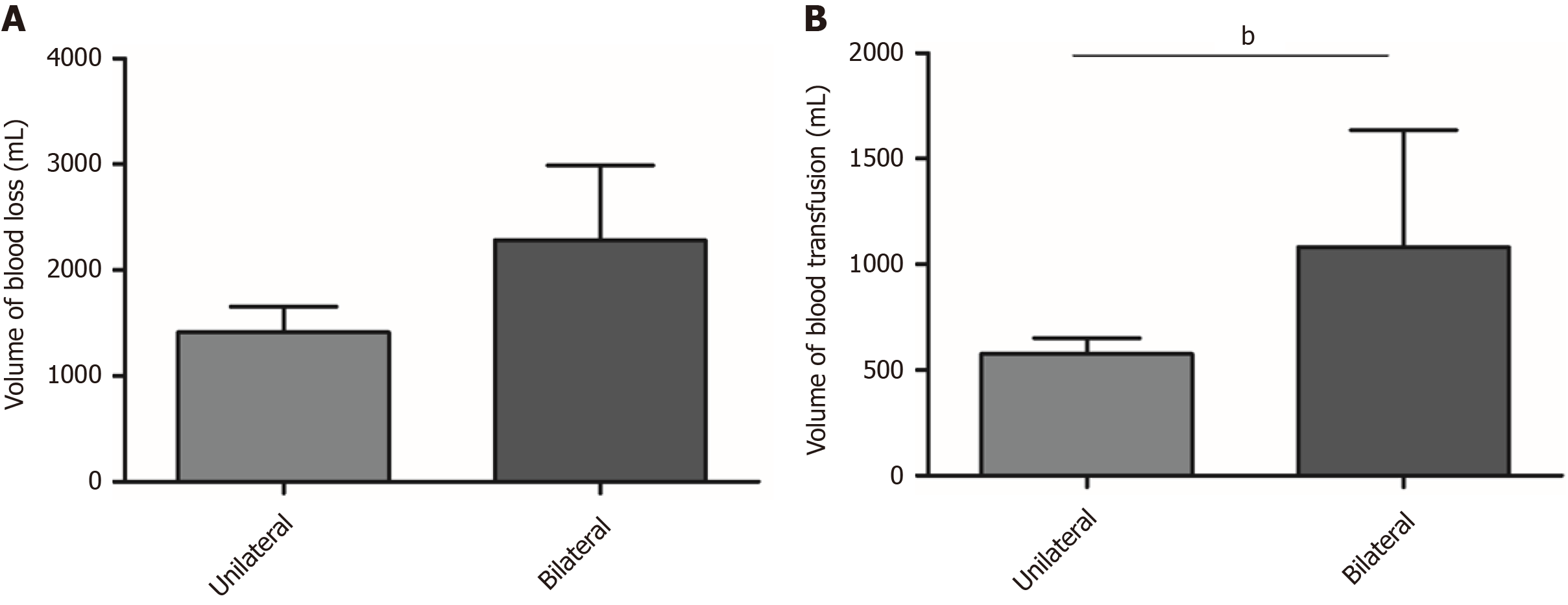
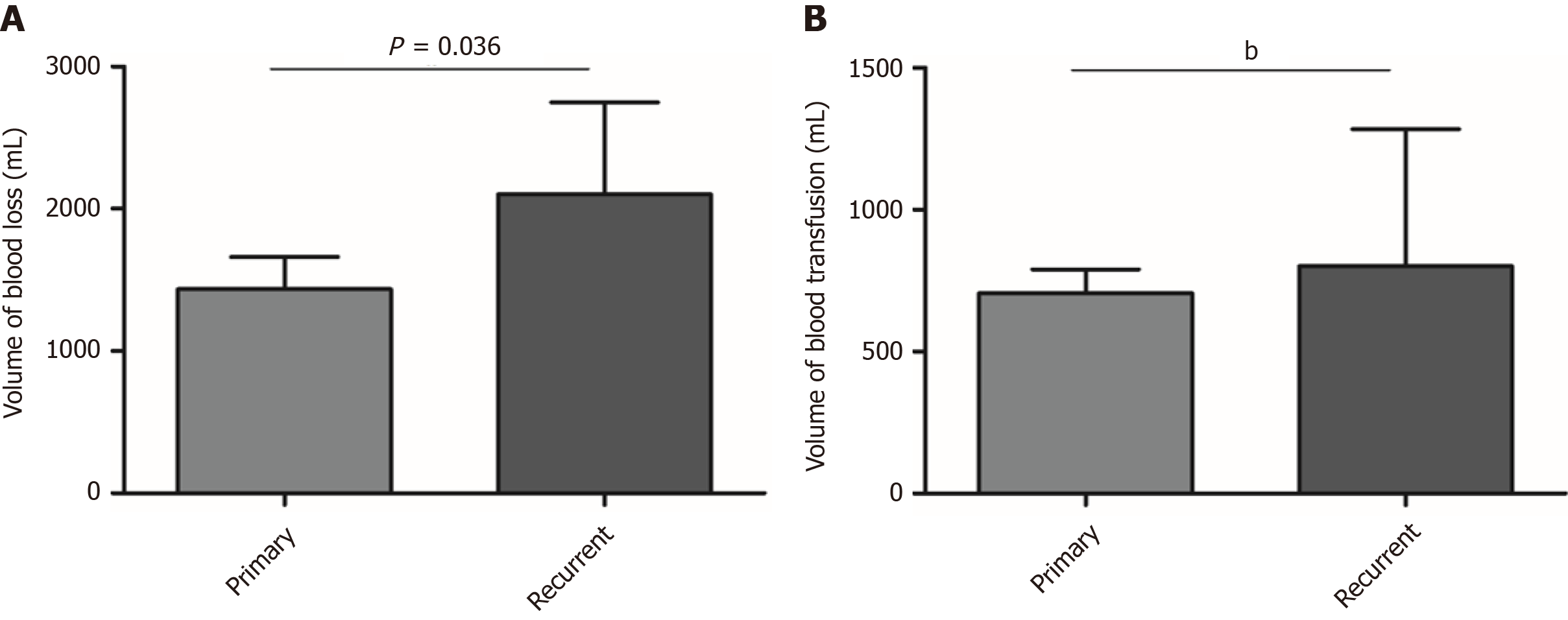
The differences in intraoperative blood loss and transfusion volume were further analyzed. For patients who underwent unilateral or bilateral iliac artery reconstruction, no significant difference in blood loss was found (P = 0.06) (Figure 3A). However, the volume of transfused blood was significantly higher for patients who received bilateral arterial reconstruction than for those who received unilateral arterial reconstruction (P < 0.001) (Figure 3B). For patients with recurrence, the volume of blood loss and transfusion volume were significantly improved compared with primary cases (Figure 4A and B).
All 15 patients were followed routinely, and 11 of them remained alive at the last follow-up. The follow-up duration ranged from 4 mo to 6.4 years, with an average of 20.8 mo. Two patients relapsed during the follow-up (1 case of recurrent UPS and 1 case of recurrent LMS). Four patients died, including two patients with UPS, one with primary LMS, and one with recurrent LPS (Table 2).
| Sex | Age | Tumor type | Pathology | DFS (mo) | |
| Case 1 | Female | 50 | Primary | UPS | 9 |
| Case 2 | Male | 51 | Recurrent | LPS | 4 |
| Case 3 | Male | 71 | Primary | LMS | 19 |
| Case 4 | Male | 54 | Recurrent | UPS | 7 |
Retroperitoneal tumors, especially RPSs, frequently invade major vessels due to their unique anatomical location and growth characteristics[8]. The most commonly involved vessels are iliac vessels, followed by the abdominal aorta, IVC, and renal veins. The most common type of RPS requiring vascular reconstruction is LPS, particularly for multiple recurrent lesions. Retroperitoneal neoplasms involving major blood vessels are not a contraindication for surgical resection. Management of RPS is technically feasible with appropriate planning and requires interdisciplinary cooperation among surgeons in professional MDTs led by sarcoma surgeons, including specialists in general surgery, urology surgery, vascular surgery, and interventional therapy. Multiple imaging modalities, such as CT, CTA, MRI, or 3D imaging, are recommended when necessary to clarify the relationship between the tumor and adjacent vessels. Intraoperative arteriography can not only block the blood flow of the artery to be ligated but also further specify the blood supply of the tumor. Complete surgical resection of RPSs invading vital organs and major vessels requires intraoperative cooperation, especially between vascular and urological surgeons[9].
More often, RPSs invade or surround the unilateral common iliac artery and the internal and external iliac arteries. In most cases, the internal iliac artery is ligated, and part of or all the external iliac arteries are resected. The common iliac artery or external iliac artery is reconstructed with the femoral artery. In our group, one patient underwent artery reconstruction between the external iliac artery and ipsilateral superficial femoral artery because of superficial invasion. Contralateral iliac artery transposition for reconstruction of the common iliac artery has also been studied in other centers and has achieved good clinical results[10].
Resection of major involved vessels such as the IVC or abdominal aorta is sometimes necessary for complete oncological clearance[11]. If the abdominal aorta below the level of the renal artery is involved, the tumor can be removed together with the abdominal aorta and iliac artery. Nephrectomy can be performed in the context of normal renal function of the other kidney. However, when the tumor involves the abdominal aorta above the renal artery level, complete resection is often difficult to achieve because of the affected celiac trunk or superior mesenteric artery. For the treatment of invaded veins, partial resection and angioplasty of the renal vein should be adopted as often as possible. If they are invaded, the common iliac vein and internal iliac vein can be resected, which will not cause severe postoperative lower limb edema due to the presence of an adequate collateral vessel network. In the case of iliac vessel involvement, the close proximity of the vein and artery often requires both venous and arterial resection to gain local control. Only three patients in our group underwent IVC partial resection or transection because most tumors were still arterially invasive. The IVC can be partially excised if it has been invaded or ligated directly if the invasion is below the renal vein. The need for IVC reconstruction should be assessed according to preoperative imaging, intraoperative findings, and the extent of surgery[12].
The most common intraoperative complication of resection of RPS involving iliac vessels is hemorrhage. Increased intraoperative bleeding is associated with a poor prognosis[2]. Herein, no statistically significant difference in blood loss was found between the unilateral and bilateral iliac arterial reconstruction groups. The volume of blood transfusion, however, was significantly higher for cases with bilateral arterial reconstruction than for those with unilateral arterial reconstruction. This result was mainly due to accurate preoperative evaluation of tumor arterial blood supply, individualized selection of surgical approach, and effective blood occlusion. Regarding bilateral artery reconstruction cases, patients with larger tumors were more often affected by severe anemia than those with smaller tumors, and occlusion of the abdominal aorta was more likely to cause unstable blood pressure than occlusion of other vessels, so a higher volume of intraoperative blood transfusion was needed.
The difficulty of resecting recurrent RPS increases over time, especially for lesions involving major blood vessels and organs. Recurrent RPS is usually more aggressive and less differentiated than primary RPS, which results in a worse prognosis. Well-differentiated liposarcoma (WDLPS) may undergo subtype transition and become dedifferentiated liposarcoma (DDLPS). It was found that 47.8% (11/23) of patients with initial WDLPS experienced pathological progression such that their recurrent tumors were of the DDLPS subtype[13]. Recurrent tumors adhere to blood vessels in a dense manner, and the original anatomical location is usually slightly different. Therefore, recurrent tumors are more likely to bleed during surgery than are primary tumors. Here, we found that the amount of bleeding and the transfusion volume were significantly increased for patients with recurrence.
Complete or "en bloc" compartmental resection of RPS with involvement of blood vessels may offer the only chance for cure for those patients who are eligible for surgery. However, for some highly malignant and recurrent RPSs, such as UPS and LMS, survival remains poor despite vascular reconstruction. In this group, four patients died, including one who suffered recurrence, one with primary UPS, and one with primary LMS (Table 2). Therefore, adjuvant therapies that include radiation and immunotherapy need to be explored to further improve patient survival.
Combined excision of the organs or structures involved requires a balance between the expected morbidity and the oncologic benefit. It is debatable whether excision should be extended to include uninvolved organs adjacent to the primary tumor. Challenging structures such as the pancreas or the spine, if clinically involved, may also be removed, but this practice increases morbidity and mortality[14]. If the tumor invades the iliac vessel and penetrates into pelvic muscle or even bone, an overly cautious resection may increase the clinical risk and probability of positive microscopic margins. In such circumstances, a second operation after neoadjuvant chemoradiotherapy is highly recommended[15].
However, there are some limitations to this retrospective clinical analysis. In large-sample studies, arterial reconstruction was found to be accompanied by high postoperative morbidity, such as patency of arteries[16]. Due to the limited sample size, we only reported one patient with artificial vessel occlusion. Given the short mean follow-up time and limited sample size, it was impossible to calculate the overall survival or the local recurrence rate at 3 or 5 years; thus, future studies need to consider these clinical outcomes.
Resection for RPS involving the iliac artery is safe, effective, and practical in a specialized MDT center that is highly experienced in this complex field of surgery. Despite the recurrence rate of RPS remaining high, resection combined with vascular reconstruction improves the R0 or R1 resection rate and results in encouraging survival for patients who were otherwise considered unresectable. Bleeding control and adequate blood transfusion affect patient recovery and surgical outcomes to a certain extent. Members from general surgery, vascular surgery, anesthesiology, blood transfusion, and intensive care teams should cooperate closely for the treatment of RPS.
Management of retroperitoneal sarcoma (RPS) involving the iliac artery is challenging and requires the concerted efforts of MDT members. Complete tumor resection together with iliac artery reconstruction can confer an outcome advantage for patients.
The retroperitoneal soft tissue tumor MDT of our hospital focuses on the standardized treatment of retroperitoneal sarcoma and has accumulated considerable experience in the surgical treatment of major involved vessels. Therefore, many typical cases and surgeries need to be further summarized and shared to improve the standardized treatment of RPS.
To summarize the clinicopathological features of patients who received RPS excision and iliac artery reconstruction and share our surgical experience in the management of the involved iliac artery.
A retrospective analysis of a maintained database consisting of 15 consecutive patients with RPS invading the iliac artery in our center from July 2004 to June 2020 was conducted. Information on baseline characteristics, type of vascular reconstruction, combined number of excised organs, volume of intraoperative blood loss and transfusion, postoperative pathology, and complications was retrieved.
Fifteen patients were enrolled in this study and received complete tumor resection (R0/R1) with iliac artery reconstruction. No serious complications occurred, and there were no perioperative deaths. Resection with bilateral iliac artery reconstruction required more intraoperative blood transfusions than resection with unilateral iliac artery reconstruction. Recurrent cases were more likely to bleed and required more blood transfusion volume than primary cases. As of January 2021, 11 patients were alive, and 4 patients had died. Local recurrence occurred in two patients.
Resection of RPS involving iliac vessels is feasible and effective when performed in collaboration with members of a multidisciplinary team (MDT) to ensure the best survival outcomes. Iliac artery oncovascular resection and reconstruction are key to a successful operation. Adequate blood preparation is important for the successful completion of surgery. However, for some highly malignant RPSs, survival remains poor despite vascular reconstruction.
Additional studies with large samples are needed to calculate survival and recurrence rates and to analyze related risk factors for patients who undergo tumor resection with iliac artery reconstruction.
The authors thank Ma LJ at the Department of General Surgery, Shanghai Public Health Clinical Center, Fudan University for helping with image editing.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Afzal MS S-Editor: Gong ZM L-Editor: Wang TQ P-Editor: Gong ZM
| 1. | Yokoyama Y, Nishida Y, Ikuta K, Nagino M. A case of retroperitoneal dedifferentiated liposarcoma successfully treated by neoadjuvant chemotherapy and subsequent surgery. Surg Case Rep. 2020;6:105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Yan Y, Xia S, Teng D, Hu S, Li S, Wang Y, Du X, Li R. Resection outcomes for primary and local recurrent retroperitoneal liposarcoma patients. Ann Transl Med. 2020;8:1450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Messiou C, Moskovic E, Vanel D, Morosi C, Benchimol R, Strauss D, Miah A, Douis H, van Houdt W, Bonvalot S. Primary retroperitoneal soft tissue sarcoma: Imaging appearances, pitfalls and diagnostic algorithm. Eur J Surg Oncol. 2017;43:1191-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 91] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 4. | Han A, Ahn S, Min SK. Oncovascular Surgery: Essential Roles of Vascular Surgeons in Cancer Surgery. Vasc Specialist Int. 2019;35:60-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Piazza M, Squizzato F, Spolverato G, Milan L, Bonvini S, Menegolo M, Grego F, Antonello M. Outcomes of polytetrafluoroethylene-covered stent versus bare-metal stent in the primary treatment of severe iliac artery obstructive lesions. J Vasc Surg. 2015;62:1210-1218.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Kalluri AG, Jain AK, Rodriguez HE, Eskandari MK. Polytetrafluoroethylene Is a Safe and Effective Interposition Conduit for Caval Reconstruction After Resection of Primary Leiomyosarcoma of the Inferior Vena Cava. Ann Vasc Surg. 2019;58:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Schwarzbach MH, Hormann Y, Hinz U, Leowardi C, Böckler D, Mechtersheimer G, Friess H, Büchler MW, Allenberg JR. Clinical results of surgery for retroperitoneal sarcoma with major blood vessel involvement. J Vasc Surg. 2006;44:46-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 118] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Bagaria SP, Gabriel E, Mann GN. Multiply recurrent retroperitoneal liposarcoma. J Surg Oncol. 2018;117:62-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Ouellette JR, Cossman DV, Sibert KS, Mcandrew NP, Silberman AW. Tumors at the aortoiliac/inferior vena cava bifurcation: preoperative, anesthetic, and intraoperative considerations. Am Surg. 2007;73:440-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Li CP, Liu BN, Wu JH, Hao CY. Contralateral internal iliac artery transposition for retroperitoneal sarcoma involving common iliac artery. Updates Surg. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Teo MC, Chow PK, Soo KC. Surgery for retroperitoneal sarcoma requiring major vascular resection and reconstruction. Asian J Surg. 2005;28:312-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Fiore M, Colombo C, Locati P, Berselli M, Radaelli S, Morosi C, Casali PG, Gronchi A. Surgical technique, morbidity, and outcome of primary retroperitoneal sarcoma involving inferior vena cava. Ann Surg Oncol. 2012;19:511-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 83] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 13. | Masaki N, Onozawa M, Inoue T, Kurobe M, Kawai K, Miyazaki J. Clinical features of multiply recurrent retroperitoneal liposarcoma: A single-center experience. Asian J Surg. 2021;44:380-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Flacs M, Faron M, Mir O, Mihoubi F, Sourouille I, Haddag-Miliani L, Dumont S, Terrier P, Levy A, Dousset B, Boudou-Rouquette P, Le Cesne A, Gaujoux S, Honoré C. Postoperative Outcome of Surgery with Pancreatic Resection for Retroperitoneal Soft Tissue Sarcoma: Results of a Retrospective Bicentric Analysis on 50 Consecutive Patients. J Gastrointest Surg. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Bachmann R, Eckert F, Gelfert D, Strohäker J, Beltzer C, Ladurner R. Perioperative strategy and outcome in giant retroperitoneal dedifferentiated liposarcoma-results of a retrospective cohort study. World J Surg Oncol. 2020;18:296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Wortmann M, Alldinger I, Böckler D, Ulrich A, Hyhlik-Dürr A. Vascular reconstruction after retroperitoneal and lower extremity sarcoma resection. Eur J Surg Oncol. 2017;43:407-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |