Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.1099
Peer-review started: July 7, 2021
First decision: October 22, 2021
Revised: November 1, 2021
Accepted: December 25, 2021
Article in press: December 25, 2021
Published online: January 21, 2022
Processing time: 191 Days and 23.7 Hours
Submucosal tumors (SMTs) refer to elevated lesions that originate from the layers below the mucosa of the digestive tract, including the muscularis, submucosa and muscularis propria. With the development and application of endoscopy and endoscopic ultrasonography (EUS), the detection rate of SMTs has increased significantly in recent years. Various diseases can lead to SMTs. However, a foreign body embedded in the gastric antrum showing clinical manifestations of a SMT is rare.
We report the case of a 47-year-old woman, who presented with upper abdominal discomfort for one year, and was subsequently diagnosed with a gastric submucosal lesion caused by an embedded foreign body by EUS and computed tomography. Considering the size and potential complications of this lesion, endoscopic full-thickness resection was performed to achieve full resection in our endoscopy center. A fish bone was found in the lesion during the operation, and was successfully removed, and the defect was later closed with endoscopic purse-string sutures.
This case report highlights the management strategies of SMTs, the importance of being familiar with diagnostic methods related to submucosal lesions, and being able to conduct effective treatment when this rare condition is highly suspected.
Core Tip: We present a patient who was hospitalized due to upper abdominal discomfort. After careful examination, the patient was diagnosed with a submucosal lesion caused by an embedded fish bone, and the lesion was subsequently removed by endoscopic full-thickness resection. This case highlights the management strategies for submucosal tumors, the importance of being familiar with diagnostic methods and being able to conduct effective treatment when this rare condition is highly suspected.
- Citation: Li J, Wang QQ, Xue S, Zhang YY, Xu QY, Zhang XH, Feng L. Gastric submucosal lesion caused by an embedded fish bone: A case report. World J Clin Cases 2022; 10(3): 1099-1105
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/1099.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.1099
Mistaken ingestion of a foreign body (FB) is common in children and adults. Being at the exploratory stage of development, children tend to put objects in their mouths[1,2]. In adults, ingestion of a FB usually occurs in those who are diagnosed with psychiatric disorders and pica[3], and prisoners who try to escape from law enforcement during access to medical service[4]. An ingested FB can become lodged in any part of the gastrointestinal tract. Depending on the FB and lodged position, FB ingestion can cause serious complications such as obstruction, perforation and bleeding. Therefore, ingestion of a FB should be paid due attention in clinical practice.
The ingestion of a fish bone has been shown to be a common cause of a FB in the digestive tract in the emergency department[5]. In clinical settings, most FBs in the digestive tract can be successfully removed with the assistance of endoscopy. However, a few FBs may lodge in the digestive tract for a long time, which can lead to other diseases or complications. Submucosal lesions are caused by tumors that stem from the muscularis mucosa, submucosa, or muscularis propria. Submucosal lesions are frequently found in the gastrointestinal tract, especially in the stomach, as often as 1 in every 300 endoscopic examinations[6]. Here, we report a patient with a fish bone embedded in the gastric antrum who presented with the manifestations of a submucosal tumor (SMT).
A 47-year-old woman presented with upper abdominal discomfort for one year.
There were no obvious reasons for her abdominal pain and discomfort after meals. Her discomfort was usually relieved after 30 min rest. A fatty diet did not aggravate the development of her discomfort or radiate to her shoulders or back. No acid reflux, belching, hiccups or black stools were reported.
The patient had no previous noteworthy medical history.
Family history was pertinent for her mother who was diagnosed with gastrointestinal stromal tumors aged 70 years.
The abdomen was soft and flat, with no spontaneous pain or tenderness. No positive results were found on physical examination.
Biochemical and hematologic test results such as tumor markers, complete blood count, electrolyte levels and liver function revealed no abnormalities.
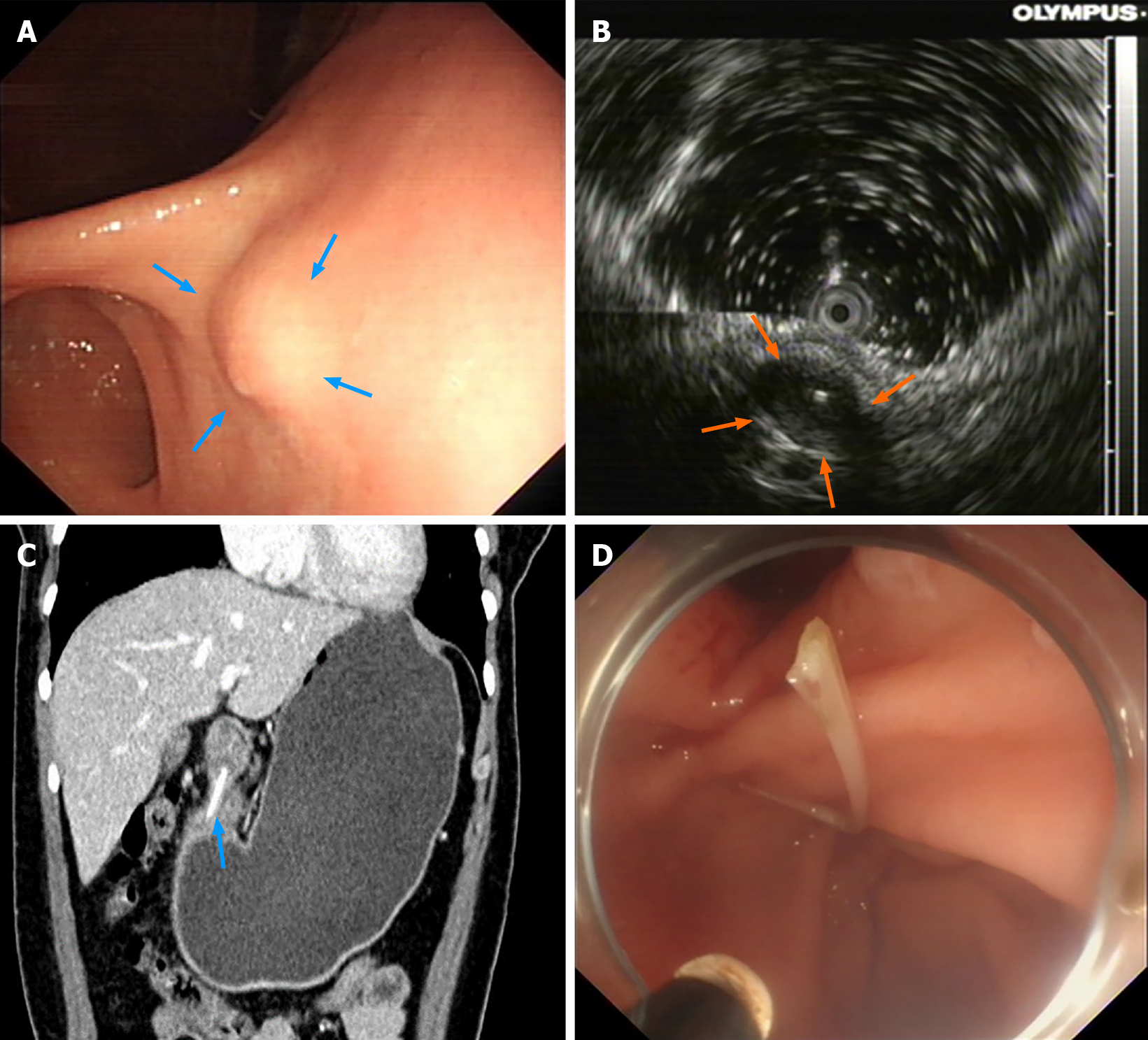
Gastroscopy and colonoscopy were performed in our endoscopy center after hospitalization. A submucosal lesion 11.1 mm in diameter was found in the gastric antrum by gastroscopy (Figure 1A). As this lesion originated from the submucosa layer, endoscopic ultrasonography (EUS) was carried out to further evaluate this lesion. The EUS results revealed a low echo of the submucosal mass-like lesion (7.2 mm × 11.1 mm) in the gastric antrum, which may have originated from the muscularis propria layer. It was also revealed that the mucosal layer of the lesion was mildly thickened; the boundaries and the serosa remained clear and basically continuous. In addition, a point-like hyperechoic image accompanied by a posterior sound shadow was detected by EUS (Figure 1B). An abdominal computed tomography (CT) scan was conducted to further confirm the relationship between the lesion and adjacent abdominal organs. Interestingly, the CT scan revealed a hyperdense linear structure in the gastric antrum wall, suggestive of a FB, which did not penetrate the serosa layer, and tissue edema, enlarged lymph nodes and exudation were not observed (Figure 1C).
Gastric submucosal lesion caused by an embedded fish bone.
Endoscopic full-thickness resection (EFTR) was performed in order to achieve full resection. During the operation, a fish bone was found in the lesion (Figure 1D), and the lesion then was completely resected. The defect was subsequently closed with endoscopic purse-string sutures. An indwelling stomach tube was placed after endoscopic surgery. In order to prevent postoperative complications, intravenous nutrition, proton pump inhibitors and anti-infection drugs were also prescribed in this patient. The stomach tube was removed 48 h later and a liquid diet was prescribed for 72 h.
On the fourth day after surgery, the patient was in a stable condition and no discomfort or abnormalities were reported. She was then discharged from hospital. No discomfort was reported at the 30-d follow-up visit.
Submucosal tumors (SMTs) are elevated lesions which originate from the layers below the mucosa of the digestive tract, including the muscularis, submucosa, and muscularis propria[7]. The mechanism of SMTs involves abnormal hyperplasia in submucosal tissue or the muscle layer and genetic factors also play a critical role in this process. Patients with SMTs are often asymptomatic, and most SMTs are found during routine health screening. In recent years, due to the wide application of endoscopy and EUS in clinical practice, the detection rate of SMTs has increased. Although the exact incidence is unknown, the detection rate of SMTs by gastroscopy is 0.33%-0.76%[8]. According to their malignant potential, SMTs can be classified into those with malignant potential including glomus tumors, carcinoids and gastrointestinal stromal tumors (GISTs), and those without malignant potential, including mesenchymal tumors, lipomas, leiomyomas, schwannomas, desmoid tumors, duplication cysts, pancreatic rests, and giant cell tumors[9]. The histopathological types of SMTs are complicated, but most are benign tumors, and less than 15% of SMTs appear to have malignant potential[10]. Leiomyoma is the most common SMT in the esophagus, accounting for 2/3 of benign esophageal tumors[11]. The stomach is the most common site for SMTs and the pathological types of stomach SMTs are even more complicated. GISTs, leiomyomas and pancreatic rests are also common in the stomach. Lipoma is the most common pathological type in the colon, while neuroendocrine tumors are most commonly found in the rectum[12].
However, the accidental ingestion of a fish bone mimicking a stomach SMT is rare. EUS is currently the most accurate diagnostic tool for evaluating SMTs in the digestive tract. It also plays an essential role in delineating histologic layers and providing key information for doctors when choosing therapeutic methods in patients with SMTs[13,14]. Previous studies have shown that the sensitivity and specificity for distinguishing different types of SMTs are 64% and 80%[15], and for SMTs with a diameter less than 2 cm, EUS is superior to CT and magnetic resonance imaging (MRI)[16]. However, EUS has several technical deficiencies. By contrast, CT is an efficient and convenient tool for diagnosing FBs embedded in the gastrointestinal tract. Data from multiple studies demonstrate that the sensitivity and specificity of CT in identifying impacted fish bones were 90.9%-100% and 100%, respectively[17,18]. The CT images of a fish bone usually appear as a calcified structure[19], and a linear calcified structure was shown on the CT images in our patient (Figure 1C), which is consistent with a previous report[20]. Therefore, EUS combined with other imaging examinations such as CT or MRI are often used to enhance diagnostic accuracy. Furthermore, doctors can also obtain detailed information on the relationship between the tumor and surrounding blood vessels or organs using CT or MRI, which is helpful in planning therapeutic strategies.
Safe treatments to remove submucosal lesions caused by FBs are essential. Data from the European Society of Gastrointestinal Endoscopy clinical guideline indicated that approximately 80%-90% of ingested FBs can pass through the digestive tract spontaneously, and the remaining 10%-20% require endoscopic interventions[21]. A case from Brazil reported that an elevated lesion was found in the gastric antrum and mimicked a GIST. The lesion was immediately removed by exploratory laparotomy and a chicken bone was found in the lesion, which had penetrated the gastric wall and into the left lateral segment of the liver[22]. This suggests that FBs embedded in the digestive tract have the potential for perforation. In a few similar reports, endoscopic submucosal dissection (ESD) was used to remove FBs. As summarized in Table 1, treatment including ESD, surgery and regular follow-up varies depending on the patient’s condition[23-25]. With the development of novel endoscopic techniques, the removal of FBs is no longer restricted to surgery. Endoscopic surgery is a better option due to the advantages of fewer hospitalized days and less invasiveness. According to previous literature, ESD is a commonly used endoscopic intervention for the removal of FBs[26-28], which avoids the need for surgical exploration. However, when choosing endoscopic treatments, the status of patients and location of the FB should also be considered. In the present report, given the chronic abdominal discomfort in this patient and the potential for severe complications, we therefore performed EFTR for complete resection.
| Ref. | Treatment | Chief complaint | Foreign body location | Foreign body |
| Carvalho et al[26], 2021 | ESD | Unclear | Esophagus | Fish bone |
| Shan et al[23], 2019 | Surgery | Abdominal pain | Stomach | Fish bone |
| Li et al[27], 2017 | ESD | Abdominal pain | Stomach | Chicken bone |
| Yip et al[28], 2017 | ESD | Odynophagia | Esophagus | Fish bone |
| Goh et al[22], 2017 | Surgery | Routine examination | Stomach | Fish bone |
| Birk et al[24], 2014 | Surgery | No symptoms | Stomach | Fish bone |
| Watanabe et al[20], 2014 | Surgery | Abdominal pain | Stomach | Fish bone |
| Nagem et al[25], 2011 | Regular follow-up | Throat pain | Esophagus | Fish bone |
In summary, a gastric submucosal lesion caused by an embedded fish bone is uncommon in daily medical practice. Therefore, the possibility of embedded FBs should also be considered when trying to identify the cause of submucosal lesions or unexplained abdominal discomfort. The diagnosis of submucosal lesions mainly depends on EUS or CT. Traditionally, surgery is the main approach for the removal of an embedded fish bone if this FB cannot be observed under endoscopy. However, endoscopic surgery is becoming feasible with the maturity of novel techniques such as ESD and EFTR. During the follow-up period, EUS is superior to endoscopy due to its ability to delineate FB location, size and histologic layers. Moreover, EUS combined with other imaging data or abdominal examinations (CT/MRI) may also be necessary. Effective treatments are needed when this rare disease is highly suspected.
A submucosal lesion caused by an embedded fish bone is an exceptional condition. With the help of endoscopy, EUS and CT, the diagnosis of a FB is not difficult. However, difficulties arise when accurately locating the FB and conducting safe and effective treatment to remove it, especially in an urgent situation. EUS and CT are useful tools in the diagnosis of FBs in the gastrointestinal tract. At present, endoscopic surgery is the first-line treatment in this situation. This study demonstrates that being familiar with diagnostic methods and conducting effective treatment are essential when this rare condition is highly suspected.
We appreciate all the medical staff in our endoscopy center involved in the treatment of this patient.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Esaki M, Panarese A, Sugimoto M, Uesato M S-Editor: Li X L-Editor: Webster JR P-Editor: Li X
| 1. | Oliva S, Romano C, De Angelis P, Isoldi S, Mantegazza C, Felici E, Dabizzi E, Fava G, Renzo S, Strisciuglio C, Quitadamo P, Saccomani MD, Bramuzzo M, Orizio P, Nardo GD, Bortoluzzi F, Pellegrino M, Illiceto MT, Torroni F, Cisarò F, Zullo A, Macchini F, Gaiani F, Raffaele A, Bizzarri B, Arrigo S, De' Angelis GL, Martinelli M, Norsa L; Italian Society of Pediatric Gastroenterology Hepatology and Nutrition (SIGENP), and The Italian Association of Hospital Gastroenterologists and Endoscopists (AIGO). Foreign body and caustic ingestions in children: A clinical practice guideline. Dig Liver Dis. 2020;52:1266-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Khorana J, Tantivit Y, Phiuphong C, Pattapong S, Siripan S. Foreign Body Ingestion in Pediatrics: Distribution, Management and Complications. Medicina (Kaunas). 2019;55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Guinan D, Drvar T, Brubaker D, Ang-Rabanes M, Kupec J, Marshalek P. Intentional Foreign Body Ingestion: A Complex Case of Pica. Case Rep Gastrointest Med. 2019;2019:7026815. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Volpi A, Laforgia R, Lozito C, Panebianco A, Punzo C, Ialongo P, Carbotta G, Sederino MG, Minafra M, Paterno A, Palasciano N. Ingestion of foreign bodies among prisoners: a ten years retrospective study at University Hospital of Southern Italy. G Chir. 2017;38:80-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Sands NB, Richardson K, Mlynarek A. A bone to pick? J Otolaryngol Head Neck Surg. 2012;41:374-380. [PubMed] |
| 6. | Standards of Practice Committee; Faulx AL, Kothari S, Acosta RD, Agrawal D, Bruining DH, Chandrasekhara V, Eloubeidi MA, Fanelli RD, Gurudu SR, Khashab MA, Lightdale JR, Muthusamy VR, Shaukat A, Qumseya BJ, Wang A, Wani SB, Yang J, DeWitt JM. The role of endoscopy in subepithelial lesions of the GI tract. Gastrointest Endosc. 2017;85:1117-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 168] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 7. | Chen H, Li B, Li L, Vachaparambil CT, Lamm V, Chu Y, Xu M, Cai Q. Current Status of Endoscopic Resection of Gastric Subepithelial Tumors. Am J Gastroenterol. 2019;114:718-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 8. | Papanikolaou IS, Triantafyllou K, Kourikou A, Rösch T. Endoscopic ultrasonography for gastric submucosal lesions. World J Gastrointest Endosc. 2011;3:86-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 51] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 9. | Longcroft-Wheaton G, Bhandari P. Endoscopic resection of submucosal tumors. Expert Rev Gastroenterol Hepatol. 2015;9:659-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Polkowski M. Endoscopic ultrasound and endoscopic ultrasound-guided fine-needle biopsy for the diagnosis of malignant submucosal tumors. Endoscopy. 2005;37:635-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 135] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Lee LS, Singhal S, Brinster CJ, Marshall B, Kochman ML, Kaiser LR, Kucharczuk JC. Current management of esophageal leiomyoma. J Am Coll Surg. 2004;198:136-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 92] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97:934-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1848] [Cited by in RCA: 1852] [Article Influence: 84.2] [Reference Citation Analysis (1)] |
| 13. | Hwang JH, Saunders MD, Rulyak SJ, Shaw S, Nietsch H, Kimmey MB. A prospective study comparing endoscopy and EUS in the evaluation of GI subepithelial masses. Gastrointest Endosc. 2005;62:202-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 144] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 14. | Hurlstone DP, Cross SS, Adam I, Shorthouse AJ, Brown S, Sanders DS, Lobo AJ. Endoscopic morphological anticipation of submucosal invasion in flat and depressed colorectal lesions: clinical implications and subtype analysis of the kudo type V pit pattern using high-magnification-chromoscopic colonoscopy. Colorectal Dis. 2004;6:369-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 48] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Yahagi N, Fujishiro M, Kakushima N, Imagawa A, Kobayashi K, Hashimoto T, Oka M, Omata M. Endoscopic submucosal dissection for lesions of the esophago-gastric junction and gastric cardia. Gastrointestinal Endosc. 2004;59:Ab171. [DOI] [Full Text] |
| 16. | Rösch T, Kapfer B, Will U, Baronius W, Strobel M, Lorenz R, Ulm K; German EUS Club. Endoscopic ultrasonography. Accuracy of endoscopic ultrasonography in upper gastrointestinal submucosal lesions: a prospective multicenter study. Scand J Gastroenterol. 2002;37:856-862. [PubMed] |
| 17. | Brand B, Oesterhelweg L, Binmoeller KF, Sriram PV, Bohnacker S, Seewald S, De Weerth A, Soehendra N. Impact of endoscopic ultrasound for evaluation of submucosal lesions in gastrointestinal tract. Dig Liver Dis. 2002;34:290-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 66] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Okten RS, Kacar S, Kucukay F, Sasmaz N, Cumhur T. Gastric subepithelial masses: evaluation of multidetector CT (multiplanar reconstruction and virtual gastroscopy) vs endoscopic ultrasonography. Abdom Imaging. 2012;37:519-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Eliashar R, Dano I, Dangoor E, Braverman I, Sichel JY. Computed tomography diagnosis of esophageal bone impaction: a prospective study. Ann Otol Rhinol Laryngol. 1999;108:708-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Watanabe K, Kikuchi T, Katori Y, Fujiwara H, Sugita R, Takasaka T, Hashimoto S. The usefulness of computed tomography in the diagnosis of impacted fish bones in the oesophagus. J Laryngol Otol. 1998;112:360-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Akazawa Y, Watanabe S, Nobukiyo S, Iwatake H, Seki Y, Umehara T, Tsutsumi K, Koizuka I. The management of possible fishbone ingestion. Auris Nasus Larynx. 2004;31:413-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Goh BK, Tan YM, Lin SE, Chow PK, Cheah FK, Ooi LL, Wong WK. CT in the preoperative diagnosis of fish bone perforation of the gastrointestinal tract. AJR Am J Roentgenol. 2006;187:710-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 137] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 23. | Shan GD, Chen ZP, Xu YS, Liu XQ, Gao Y, Hu FL, Fang Y, Xu CF, Xu GQ. Gastric foreign body granuloma caused by an embedded fishbone: a case report. World J Gastroenterol. 2014;20:3388-3390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Birk M, Bauerfeind P, Deprez PH, Häfner M, Hartmann D, Hassan C, Hucl T, Lesur G, Aabakken L, Meining A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 388] [Article Influence: 43.1] [Reference Citation Analysis (0)] |
| 25. | Nagem RG. An unexpected cause of gastric submucosal lesion. Einstein (Sao Paulo). 2017;15:112-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Carvalho AC, Pires F, Araújo R. Removal of an embedded foreign body in the stomach by a technique of endoscopic submucosal dissection. Dig Endosc. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 27. | Li Y, Zhang L, Nie YQ. Embedded fish bone in the stomach mimicking a submucosal tumor. Gastrointest Endosc. 2017;85:262-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Yip HC, Chiu PW, Chan SM, Teoh AY, Ng EK. Removal of submucosal embedded fish bone in the esophagus with endoscopic submucosal dissection. VideoGIE. 2017;2:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |