Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.1050
Peer-review started: June 21, 2021
First decision: July 15, 2021
Revised: July 24, 2021
Accepted: December 22, 2021
Article in press: December 22, 2021
Published online: January 21, 2022
Processing time: 208 Days and 8.9 Hours
A male urethral disruption injury is a urological emergency. Primary endoscopic realignment (PER) refers to reestablishment of urethral alignment via indwelling urethral catheter by cystoscope, which is recommended as the optimal emergent treatment approach for reducing the likelihood of complications following injury. However, the prior literature suggests the success rate of PER to be relatively low due to complicated urethral disruption. We report a modified PER approach that serves to improve both the success rate and safety of the treatment.
A 19-year-old male patient presented with multiple pelvic fractures and complete urethral disruption following a high-velocity traffic accident. The patient’s abdominal computed tomography and retrograde urethrography results revealed complete urethral disruption at the bulbar urethra, with hematoma and contrast medium extravasation that extended into the extraperitoneal space. The conventional retrograde PER by cystoscope failed due to severe disruption and considerable hematoma. Modified simultaneous antegrade and retrograde PER was performed by means of semi-rigid ureteroscopy via a suprapubic Foley catheter and cystoscopy via the external urethra. An antegrade guidewire was passed through the bladder neck and then pulled out through the external urethral meatus with a cystoscope. Urethral continuity was achieved after a 16-Fr silicone Foley catheter was indwelled into the bladder along the guidewire. The patient recovered well, achieving voiding continence and avoiding further operation for urethral stricture.
Modified PER via suprapubic Foley catheter represents a promising and safe treatment approach in patients with posterior urethral injuries.
Core Tip: We report a modified primary endoscopic realignment to improve both the success rate and intraoperative safety of a patient with high-grade urethral disruption injury. The surgery was performed with simultaneous antegrade and retrograde endoscopes. We used a suprapubic Foley catheter to serve as an access route of the antegrade cystoscope. The antegrade guidewire was passed through the bladder neck and pulled out through the external urethra, with assistance of the retrograde cystoscope. For the 19-year-old male who presented with high-grade complete urethral disruption after traffic accident, modified endoscope realignment was achieved, and the patient recovered well.
- Citation: Ho CJ, Yang MH. Novel method of primary endoscopic realignment for high-grade posterior urethral injuries: A case report. World J Clin Cases 2022; 10(3): 1050-1055
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/1050.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.1050
Although traumatic posterior urethral injuries (PUIs) remain uncommon, they have been reported to co-occur with pelvic fractures[1]. Indeed, prior studies have estimated the incidence of PUIs following pelvic fractures to be as high as 25%[2]. While a PUI does not represent a life-threatening injury, it may profoundly compromise a patient’s quality of life due to being associated with morbidities such as urethral stricture, erectile dysfunction, and urinary incontinence[1,3]. The European Association of Urology guidelines on urological trauma recommend primary endoscopic realignment (PER) as the preferred technique for the treatment of PUIs[4]. Several studies have shown that when treated with PER, patients exhibit a lower rate of urethral stricture as well as a reduced need for subsequent urethroplasty[3]. Retrograde cystoscopy has traditionally been the most commonly used method for performing PER. However, a previous study reported that the success rate when using retrograde cystoscopy was only 21%[5]. The high failure rate is likely due to several reasons, including the fact that high-grade PUIs are usually associated with a significant gap between disruption-ends of the urethra. In addition, the peripheral hematoma typically seen following a PUI can limit the surgeon’s vision when using a scope, which can make performing the realignment more difficult.
In an effort to increase the success rate of PER, one retrospective study suggested performing antegrade realignment via the suprapubic tract using semi-rigid ureteroscopy[6]. However, this technique requires the use of a unique peel-away sheath to establish a suprapubic tract, which is not currently widely accessible.
In the present study, we report a modified approach involving simultaneous antegrade and retrograde PER performed by means of semi-rigid ureteroscopy in a case of total disruption PUI. More specifically, the antegrade PER was performed via a suprapubic tract established with a Foley catheter, which could serve as a safer and more efficient method.
A 19-year-old male patient was brought to our emergency room after suffering multiple pelvic fractures complicated by urethral injury following a high-velocity motorcycle accident.
The patient developed acute urinary retention after the initial injury, followed by lower abdomen distention without urethral meatus bleeding.
The patient had no relevant prior medical history.
The patient had no personal and family history.
The patient’s physical examination revealed no obvious ecchymosis on the penis, scrotum, or perineum.
The patient had no specific laboratory abnormalities.
Due to the suspicion of urethral trauma, abdominal computed tomography with retrograde urethrography was performed in the emergency room. Contrast medium extravasation at the bulbar urethra was noted, with a massive hematoma surrounding and extending into the extraperitoneal space. A so-called “pie in the sky” sign was also observed, indicating that the urethra was totally disrupted, causing the prostate to be displaced upward (Figure 1).
The patient was diagnosed with American Association for the Surgery of Trauma grade IV-V complete urethral disruption. Further, Tile type-A2 stable pelvic ring fractures were also identified over the bilateral pubic ramus.
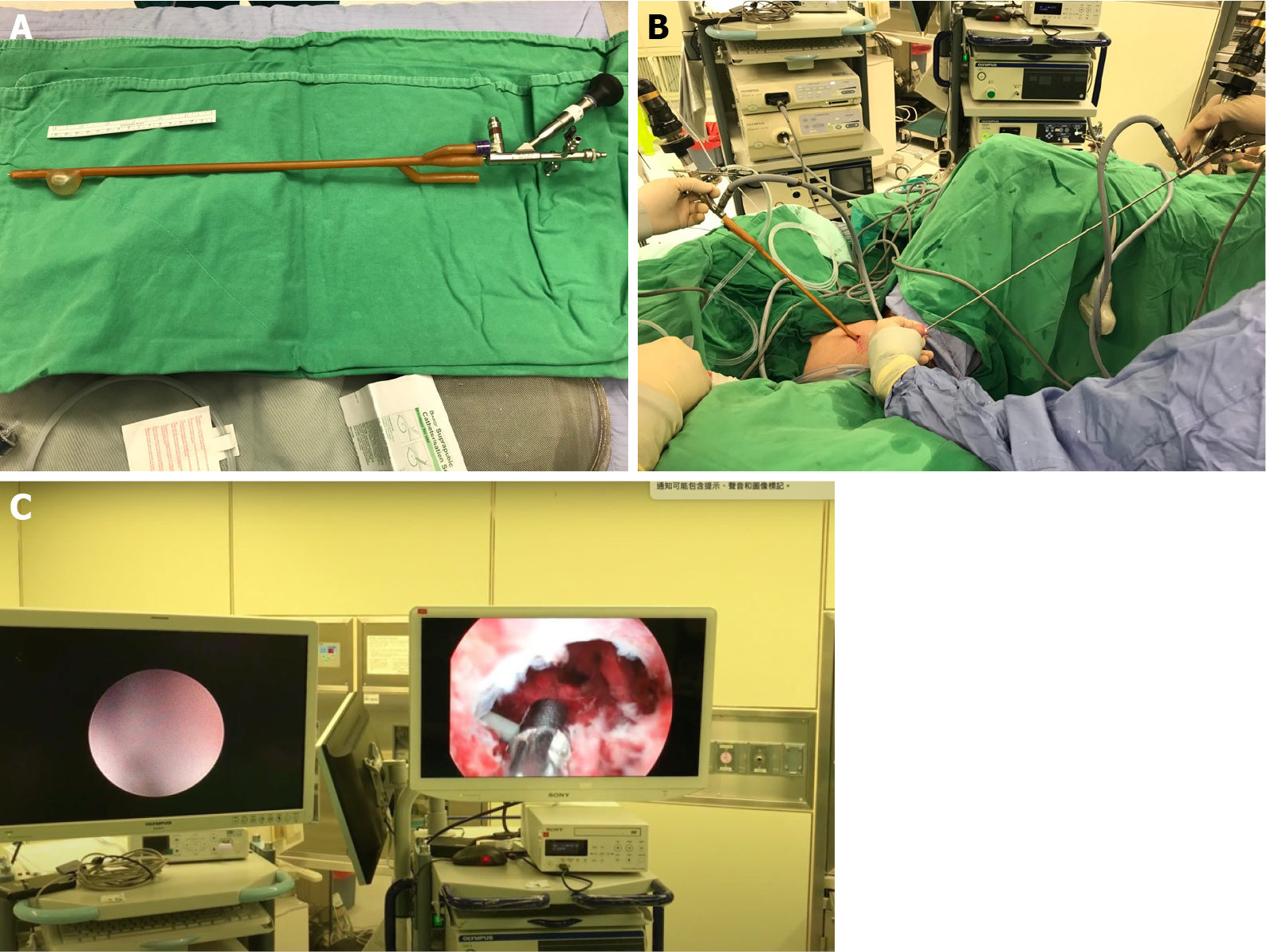
The patient underwent an emergency operation involving PER. First, a 22.5-Fr cystoscope was inserted into the patient’s urethra; although, this attempt at retrograde realignment failed. Next, simultaneous antegrade and retrograde endoscopic examinations were performed. The procedure is illustrated in Figure 2. A suprapubic cystostomy puncture under ultrasound guidance was performed using a cystostomy trocar and a side-slit cannula. Once the trocar was engaged in the intravesical space, a 22-Fr three-way Foley catheter was placed through the cystostomy tunnel and then fixed by means of balloon inflation. The tip of the Foley catheter was incised before it was inserted to perform the subsequent procedure (Figure 2A). Following the removal of the cystostomy side-slit cannula, a semi-rigid 4.5/6.5-Fr ureteroscope was inserted into the bladder via the cystostomy Foley catheter in order to examine the bladder and bladder neck (Figure 2B). A hydrophilic guidewire (ZIPwire™; Boston Scientific, Boston, MA, United States) was passed through the bladder neck and then pulled out through the external urethral meatus using grasping forceps designed for use with a cystoscope (Figure 2C). The retrograde cystoscope was indwelled along the guidewire, which was then replaced with a rigid guidewire (Fixed Core Wire Guide; Cook Medical, Bloomington, IN, United States). Urethral continuity was achieved after a 16-Fr silicone Foley catheter was indwelled into the bladder along the guidewire. Finally, both the suprapubic cystostomy and the urethral Foley catheter were left in place.
The patient recovered well and did not experience any complications. He was discharged on the seventh postoperative day. The urethral Foley catheter was removed on the 28th postoperative day, and the patient exhibited voiding continence and complete voiding. The cystourethroscopy results revealed that the patient’s injuries had healed well without bulbomembranous urethra stricture (Figure 3). Moreover, the patient reported nocturnal penile tumescence and erection following sexual stimulation.
The classic presentation of high-grade urethral injury involves bloody discharge over the urethral meatus and difficulty in relation to urination. Clinicians should perform retrograde urethrography for diagnostic purposes following pelvic trauma. Immediate suprapubic tube (SPT) placement used to be the standard treatment approach in the case of PUI. However, patients who were treated with only SPTs were found to always develop complete stenosis, which necessitated further treatment by means of posterior urethroplasty[7]. Thus, PER was suggested as a more promising treatment approach for a number of reasons, including the fact that PER of urethral distraction defects may allow for any subsequent strictures to be managed endoscopically or via easier posterior urethroplasty due to realigning the distracted urethra and shortening the stricture length[8]. Hadjizacharia et al[9] reviewed the outcomes of 21 patients, including 14 treated with PER and 7 with SPT. The patients treated with PER were found to have a shorter time to self-voiding as well as a lower stricture rate when compared with the SPT group. Johnsen et al[3] found that PER could serve as the definitive therapy in more than a third of all treated patients. It could also prevent the need for formal urethroplasty, even in cases in which the PER failed.
As endoscopic equipment and techniques have developed, PER with simultaneous antegrade and retrograde flexible cystoscopy has become increasingly common. However, the high intraoperative irrigation flow and crude scope diameter could exacerbate any soft tissue injury and increase the risk of the pelvic hematoma becoming infected. Tausch et al[10] reviewed a sample of patients with PUI. They concluded that while PER may result in the restoration of urethral continuity without the need for further intervention, PER patients may require multiple interventions and experience more adverse events than SPT patients. Zhang et al[6] reported a modified procedure involving the use of standard semi-rigid ureteroscopy to reduce manipulation-related trauma, which resulted in a good success rate and a low subsequent comorbidity rate. However, the suprapubic route was established by means of serial sheath dilatations and then completed using a 16-Fr peel-away sheath. Unfortunately, this equipment is not readily available, especially in rural regions.
In our case, we used 4.5/6.5-Fr semi-rigid ureteroscopy to perform the antegrade cystoscopy in order to achieve realignment. In contrast to the above-mentioned studies, the access route was established using a 22-Fr Foley catheter, which is a common piece of medical equipment found in every hospital. Furthermore, endoscopic realignment using a Foley catheter offers several advantages. First, the Foley balloon can serve as a seal between the Foley catheter and the bladder wall, which should prevent further fluid extravasation into the extraperitoneal space during a prolonged procedure. Thus, the postoperative infection rate, ileus rate, and abdominal discomfort level should be minimized. Second, the urinary bladder is a flexible organ, meaning that the established access route when using a non-fixable sheath could be dislocated when the bladder deflates. The use of a Foley balloon can ensure more secure access and a lower risk of dislocation during the procedure. Third, most urologists are familiar with the ultrasound-guided percutaneous cystostomy procedure, which could help to reduce the operative time without the requirement for a steep learning curve when compared with other innovative procedures. Fourth, due to the likelihood of multi-traumatic and complex comorbidities, a patient with a PUI usually carries a high risk when undergoing anesthesia. With the use of an established suprapubic Foley catheter, the operation could be terminated at any time with a sufficient outflow tract available for urinary diversion.
Pelvic fractures accompanied by posterior urethral disruption can be encountered during emergency medical practice. To avoid further morbidity and reduce the need for urethroplasty, PER could serve as a promising initial management approach. This case report presented a modified PER procedure with a high success rate and an easy-to-learn method that involves the insertion of a ureteroscope into a suprapubic Foley catheter. Because the Foley catheter is available in most hospitals and the cystostomy procedure is familiar to most urologists and physicians, the described procedure could be widely adopted by general emergency facilities.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Joalsen I, Setiawan E, Velikova TV S-Editor: Chang KL L-Editor: A P-Editor: Chang KL
| 1. | Latini JM, McAninch JW, Brandes SB, Chung JY, Rosenstein D. SIU/ICUD Consultation On Urethral Strictures: Epidemiology, etiology, anatomy, and nomenclature of urethral stenoses, strictures, and pelvic fracture urethral disruption injuries. Urology. 2014;83:S1-S7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 118] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 2. | Light A, Gupta T, Dadabhoy M, Daniel A, Nandakumar M, Burrows A, Karthikeyan S. Outcomes Following Primary Realignment Versus Suprapubic Cystostomy with Delayed Urethroplasty for Pelvic Fracture-Associated Posterior Urethral Injury: A Systematic Review with Meta-Analysis. Curr Urol. 2019;13:113-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 3. | Johnsen NV, Dmochowski RR, Mock S, Reynolds WS, Milam DF, Kaufman MR. Primary Endoscopic Realignment of Urethral Disruption Injuries--A Double-Edged Sword? J Urol. 2015;194:1022-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Lynch TH, Martínez-Piñeiro L, Plas E, Serafetinides E, Türkeri L, Santucci RA, Hohenfellner M; European Association of Urology. EAU guidelines on urological trauma. Eur Urol. 2005;47:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 182] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 5. | Leddy LS, Vanni AJ, Wessells H, Voelzke BB. Outcomes of endoscopic realignment of pelvic fracture associated urethral injuries at a level 1 trauma center. J Urol. 2012;188:174-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Zhang Z, Fang L, Chen D, Li W, Peng N, Thakker PU, Zhang Y, Wang X. A Modified Endoscopic Primary Realignment of Severe Bulbar Urethral Injury. J Endourol. 2021;35:335-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | McDougal WS, Wein AJ, Kavoussi LR, Partin AW, Peters CA. Campbell-Walsh Urology 11th Edition Review. New York: Elsevier Health Sciences, 2015. |
| 8. | Elshout PJ, Veskimae E, MacLennan S, Yuan Y, Lumen N, Gonsalves M, Kitrey ND, Sharma DM, Summerton DJ, Kuehhas FE. Outcomes of Early Endoscopic Realignment Versus Suprapubic Cystostomy and Delayed Urethroplasty for Pelvic Fracture-related Posterior Urethral Injuries: A Systematic Review. Eur Urol Focus. 2017;3:545-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Hadjizacharia P, Inaba K, Teixeira PG, Kokorowski P, Demetriades D, Best C. Evaluation of immediate endoscopic realignment as a treatment modality for traumatic urethral injuries. J Trauma. 2008;64:1443-1449; discussion 1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Tausch TJ, Morey AF. The case against primary endoscopic realignment of pelvic fracture urethral injuries. Arab J Urol. 2015;13:13-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |