Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.1008
Peer-review started: April 1, 2021
First decision: May 11, 2021
Revised: June 20, 2021
Accepted: December 25, 2021
Article in press: December 25, 2021
Published online: January 21, 2022
Processing time: 290 Days and 0.2 Hours
Meningiomas are benign tumors that originate from the meningothelial arachnoid cells, but they rarely develop extracranially. There is no specific surgical guideline for resecting them in the maxillary sinus, and little is known about their biological behavior and operative management.
We present a 54-year-old female patient referred to our department with a primary extracranial meningioma that presented as buccal swelling associated with headache. On clinical examination the mass was non-tender, fixed, sessile and non-pulsatile situating in the right maxillary sinus. Computed tomography scan showed a well-defined mass of 7 cm × 6 cm × 6 cm compressing the surrounding structures. Magnetic resonance imaging revealed a well circumscribed heterogenous lesion with necrotic center and relatively hypointense on T2-weighted imaging. Imaging studies revealed no evidence of intracranial extension and metastatic nests. Biopsy showed grade I primary extracranial with low mitotic activity. Total maxillectomy with excision of tumor and adjacent paranasal structures following reconstruction of the orbit and maxilla with tissue patch was done by the maxillofacial surgeon. The biopsy reported fibrous meningioma based on the hematoxylin and eosin section. On immunohistochemistry the tumor cells were positive for vimentin, focally positive for epithelial membrane antigen and CD99 and negative for signal transducer and activator of transcription 6. The mass was removed surgically with reconstruction, and the pathological studies confirmed the diagnosis to be an extracranial meningioma. The present study briefly reviews the current knowledge concerning the diagnosis and treatment of extracranial meningiomas in the head and neck area and offers suggestions for managing extracranial meningiomas in the paranasal sinuses.
To conclude, extracranial meningiomas in the paranasal sinuses may be successfully managed by surgical treatment without evident post-surgery complications.
Core Tip: Meningiomas are rare benign tumors originating from the meningothelial arachnoid cells that rarely occur in an extracranial location. So herein we present a rare case of extracranial meningioma in the maxillary sinus of a 54-year-old female presenting with right buccal swelling. Headache was the only symptom. This case mainly focuses on the diagnosis and surgical management with reduced post-surgical complication and provides an insight and surgical guideline in treatment planning.
- Citation: Sigdel K, Ding ZF, Xie HX. Case of primary extracranial meningioma of the maxillary sinus presenting as buccal swelling associated with headache: A case report. World J Clin Cases 2022; 10(3): 1008-1015
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/1008.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.1008
Meningiomas are one of the largest groups of brain tumors. They come in two forms: intracranial and extracranial. The extracranial location is very rare. Approximately 6%-17% of all meningiomas can be found in extracranial regions[1]. Male patients are more likely to have extracranial meningiomas[2]. We describe a rare case of primary extracranial meningioma of the maxillary sinus in a 54-year-old female patient presenting as buccal swelling and headache. Regardless of the grade, the recommended treatment is complete surgical excision if possible; we used a combined surgical approach to achieve complete excision of the lesion. The clinical, histological and immunohistochemical features are described. The possible histogenesis and the differential diagnosis are also discussed. Subsequently, we reviewed the literature on this respect.
A 54-year-old female patient presented with right buccal swelling for 2 years and headache for 2 mo to the Department of Head and Neck Oncology Surgery, West China College of Stomatology, Sichuan University.
The patient visited a local hospital and started anti-inflammatory and analgesic drugs as they considered the symptoms to be caused by cold and toothache, but the pain did not improve significantly. The patient again visited Guangyuan People’s Hospital seeking further treatment. The biopsy taken showed the spindle cell tumor in the right maxillary sinus, which was further examined by immunohistochemistry. The patient denied any shortness of breath, nausea, dysphagia, hoarseness, loss of consciousness and any neurological or constitutional symptoms at any time.
The patient had no previous medical history.
She was a non-smoker with no specific family history.
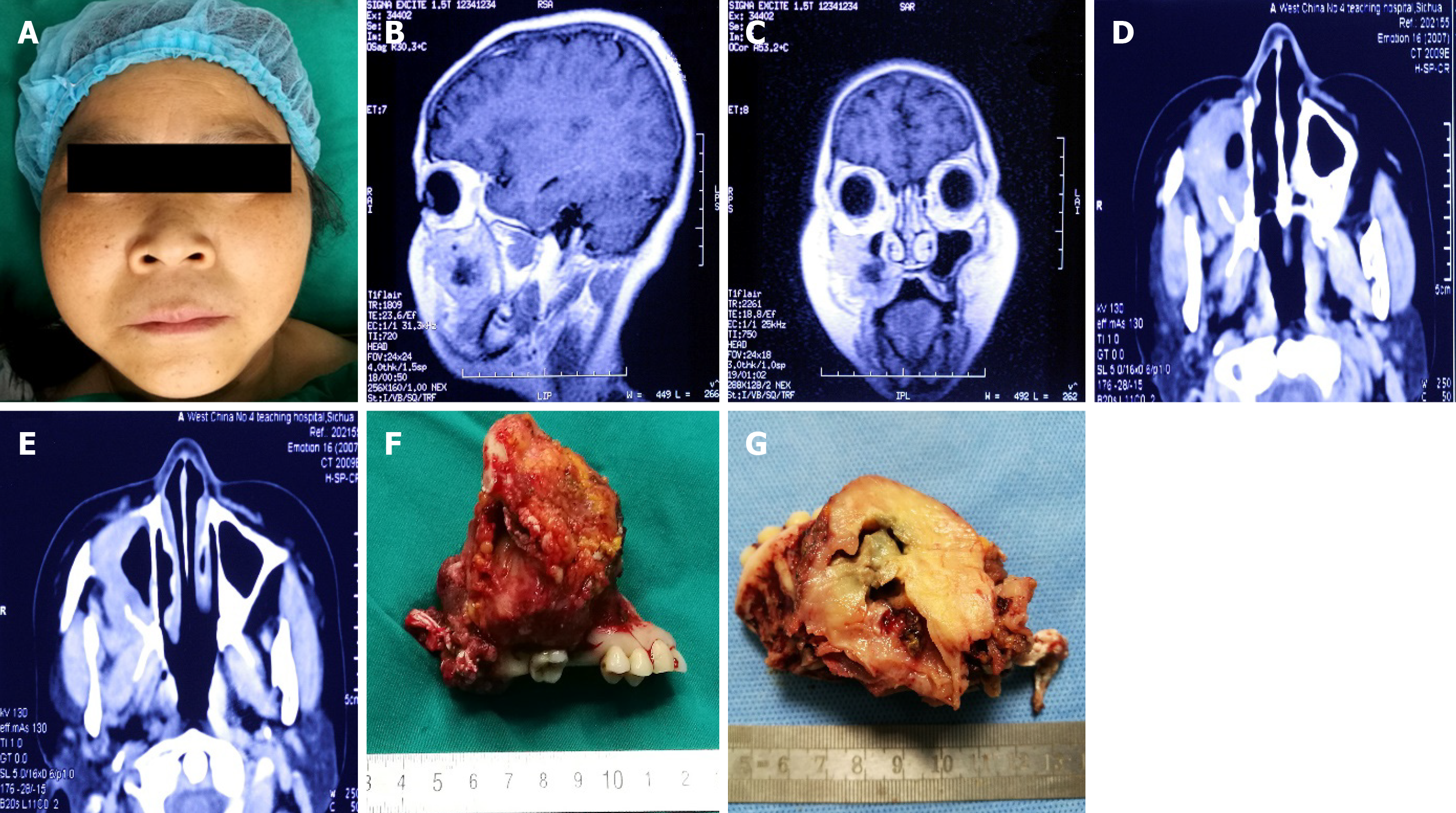
On extra-oral examination the mass located in the right face was non-tender, fixed and non-pulsatile and sessile (Figure 1A). The patient did not have any palpable lymph nodes or associated neck masses. Upon intra-oral examination, an obvious buccal swelling covered with slightly red oral mucosa was present. The majority of the mass was located in the right maxillary sinus and involved the base of the maxilla.
The patient underwent biopsy of the mass using gingival incision extending as far as the upper first molar teeth under local anesthesia. Biopsy reported a grade I primary extracranial meningioma with low mitotic activity. Hematological examinations were within normal limits.
Magnetic resonance imaging revealed a well-circumscribed heterogenous lesion with a necrotic center and was relatively hypointense on T2-weighted imaging (Figure 1B and C).
Computed tomography (CT) demonstrated the presence of a large, well-defined soft tissue mass measuring about 7 cm × 6 cm × 6 cm occupying the entirety of the right maxillary sinus, affecting nearby sphenoid and ethmoid sinuses, without affecting the dura mater or endocrinal structures. The surrounding structures were compressed by the mass, and the mass extended from the roof of the oral cavity into the skull base. CT on bone window setting showed an expansive mass with a high density area in the right maxillary sinus. The anterior and lateral walls of the maxillary sinus were thinned and destructed by the expanding mass, with erosion of the wall of the right maxillary sinus as well as orbital floor. (Figure 1D and E). Imaging study based on comprehensive detection of the lesion revealed that there was no evidence of intracranial extension and metastatic nests.
Right maxillary meningioma.
As intracranial invasive meningioma was excluded, the surgery was decided to be performed by the Oral and Maxillofacial Surgeons. Total maxillectomy together with the excision of the tumor and the adjacent paranasal structures, following reconstruction of the orbit and maxilla with tissue patch was performed.
On June 6, 2016, under general anesthesia “extended resection of right maxillary meningioma; right maxillary extended resection; inferior turbinate partial resection; middle turbinate partial resection; right-sided canal neurotomy; right trigeminal peripheral branch transection; A1 extraction; A1-A7 gingival flap; and free skin patch repair” was performed.
Frozen pathology showed spindle cell tumor with extensive necrosis in the right maxilla, which was confirmed by extensive biopsy and immunohistochemical staining. The operation lasted for 2 h and 5 min. The blood loss was 650 mL, and the fluid infused was 2600 mL during the operation. After the operation, the patient returned to the intensive care unit. The vital signs of the patient were observed. Ceftriaxone 2.0g IV BD for 4 d was used to treat infection and prevent intracranial infection. Postoperative nutritional support and antitumor therapy were used.
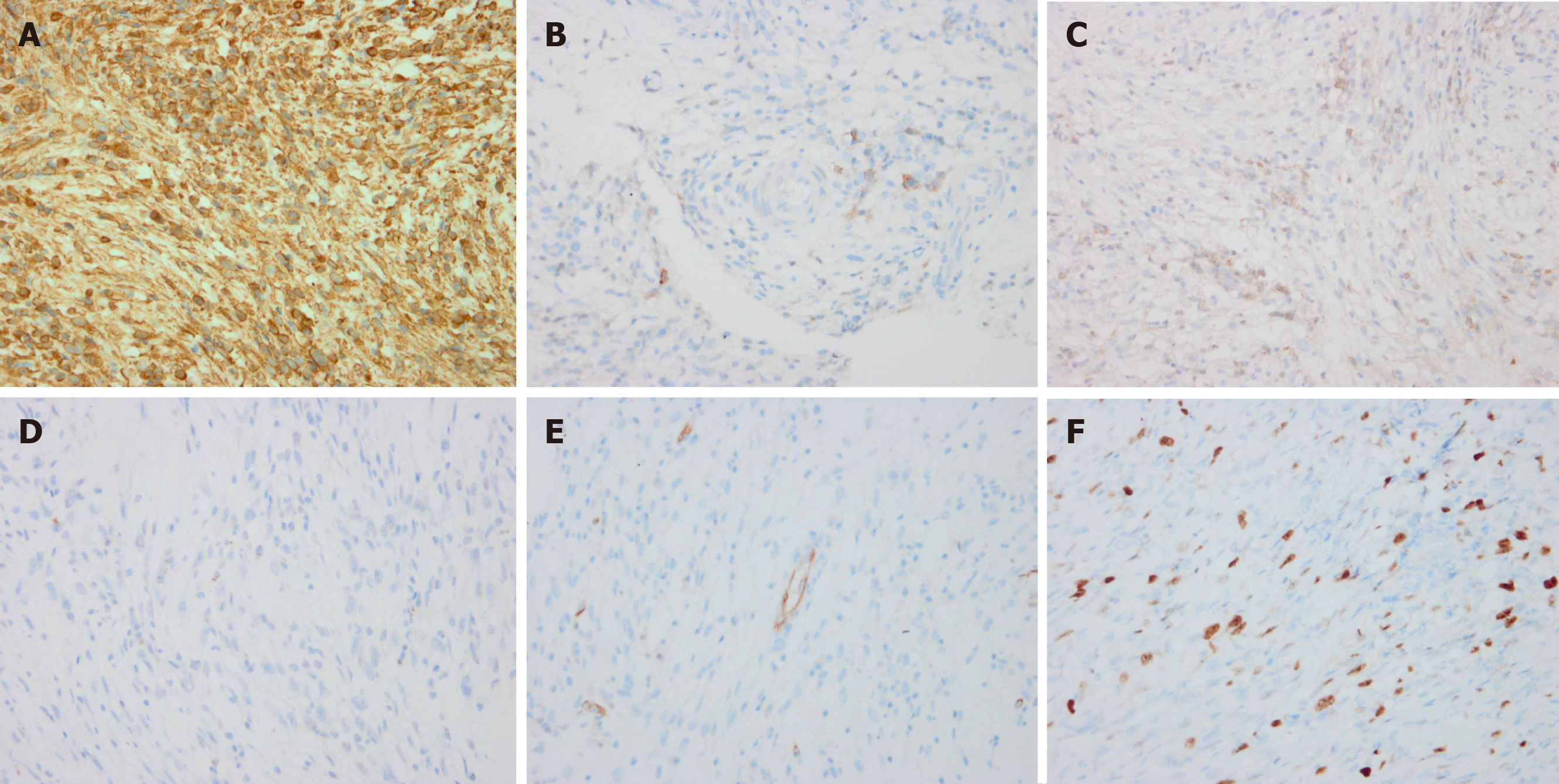
The entire tumor specimen was submitted for histology, and fresh tissue was fixed in formaldehyde solution for ultrastructural analysis. Histologically, the specimen consisted of epithelioid lobulated tissue, separated by abundant collagen fibers (Figure 2A and B). Image analysis at high magnification showed a thick fibrous capsule and was composed of interwoven fascicles of spindle-shaped meningiocytes and collagen fibers that were arranged into lobules. The tumor cells had abundant cytoplasm and indistinct cytoplasmic borders, arranged in whorled and lobulated patterns. There was osteoid formation in the tumor. No cytologic atypia or necrosis were discovered, but some mitoses were present. The specimen showed abundant cytoplasm and indistinct cytoplasmic borders, arranged in whorled and lobulated patterns (Figure 2C and D). Based on the hematoxylin and eosin sections, the lesion was diagnosed as a fibrous meningioma.
Immunohistochemically, the tumor cells were strongly positive for vimentin (Figure 3A), focally positive for epithelial membrane antigen (Figure 3B) and CD99 (Figure 3C). The cells showed negative staining for signal transducer and activator of transcription 6 (Figure 3D) and CD34 (Figure 3E). The MIB-1 (Ki-67) labeling index was 15% (Figure 3F), i.e. focally positive.
The patient was discharged with the following advice: perform mouth opening exercises; fabricate lumbar appendage in Prosthodontic Department a month later; radiotherapy should be done; proper nutritional support, proper oral hygiene and proper wound care; avoid spicy, acidic and irritating foods; and review after discharge for 1 mo and follow-up for discomfort.
Meningiomas can exist as intracranial or extracranial brain tumors and are benign, slow-growing tumors. The extracranial location accounts for 2% of all these tumors[3] and found most often in male patients and in young individuals[4]. Due to their unusual symptoms and lack of prevalence, primary extracranial meningiomas are often misdiagnosed[5]. Fortunately, 80% of extracranial tumors are benign[6]. Cases of extracranial meningioma of the sinonasal tract[7], retromolar area[8], eyebrows[9], pelvis[10], etc. have also been reported. Some of the published reports of extracranial meningiomas are listed in Table 1. Histologically, primary extracranial meningiomas do not differ from intracranial, and most of these tumors are sporadic with unclear etiology[11]. Primary extracranial meningiomas have been considered as arising independently from cranial nerve sheaths or from extracranial embryonic rests of arachnoid cells and as extracranial metastases of a primary intracranial meningioma, but their origin has not been completely established[12].
| Ref. | Year of publication | Site of primary extracranial meningioma | Diagnostic tests | Histology | Treatment performed |
| Maharjan et al[15] | 2018 | Nasal cavity | Contrast-enhanced CT of the nose and paranasal sinuses | WHO grade II atypical transitional meningioma | Endoscopic excision of the mass |
| Kim et al[18] | 2018 | Forehead | CT scan | Lobular architecture composed of tumor cells with eosinophilic cytoplasm and indistinct cell border | Excisional biopsy under local anesthesia |
| El-Daly et al[1] | 1997 | Maxillary antrum | CT scan | Interlacing bundles of bland-appearing spindle cells associated with calcific deposit | Medial maxillectomy with complete removal of the tumor |
| Ho et al[5] | 1980 | Right nasal cavity | Sinus x-ray and CT | Clearly demarcated meningioma with fibrous capsule and well-preserved pseudostratified respiratory epithelium | Ablation of the right frontal sinus, external ethmoidectomy and excision of the right middle turbinate |
| Nur et al[12] | 2006 | Right pelvic cavity | Pelvic sonogram | Lobulated pattern composed of solid sheets of tumor cells separated by connective tissue septae | Exploratory laparotomy with optimal debulking of the pelvic tumor |
| Albsoul et al[11] | 2015 | Right side neck mass | CT and MRI | Meningothelial cells with intranuclear inclusion and multiple psammoma bodies | Partial excision of the mass |
| Takeshima et al[9] | 2004 | Right ovary | Abdominal CT | Mature cerebral tissue was also noted. Melanocytes with black pigment were scattered in the peripheral region of the brain tissue | Right salpingo-oophorectomy |
| Lingen et al[8] | 1995 | Right maxillary sinus | CT | Bundles of ovoid and spindle-shaped cells arranged in broad bands | Total maxillectomy |
| Rege et al[16] | 2017 | Right retromolar area | CBCT | Spindle cell neoplasm, without evidence of atypia, whorls suggesting meningothelial origin | Partial resection of the mandible and reconstruction with autogenous iliac tricortical bone |
| Lee et al[17] | 2017 | Left eyebrow | CT | Tumor cells arranged in sheets or whorls, with occasional psammomabodies | Surgical excision |
| This Study | (Present case) | Maxillary sinus | CT and MRI | Epithelioid lobulated tissue, separated by abundant collagen fibers | Total maxillectomy with excision of tumor |
The present case shows the clinical and imaging aspects of extracranial meningioma of the maxillary sinus in an elderly lady. Primary extracranial meningioma of the paranasal sinuses is rare[13]. In general, the most common signs and symptoms of paranasal sinus meningiomas may mimic cases of sinusitis with nasal obstruction, anosmia, facial pressure or pain, epistaxis and rhinorrhea[14,15]. Meningiomas in the extracranial space often present with nonspecific symptoms until the tumor has reached a significant size. This was the case with our patient who had buccal swelling for 2 years, which has been neglected by the patient until the headache started. Clinical examination should be comprehensive because more than 10% of cases may remain asymptomatic even in advanced stages[15]. Imaging studies, especially CT and magnetic resonance imaging scans, have proved to be useful in the diagnosis and management of meningiomas. The differential diagnosis should include a variety of benign and malignant neoplasms such as melanoma, olfactory neuroblastoma, carcinoma, hemangioma, sarcoma and aggressive psammomatoid ossifying fibroma[10,14]. Histology is therefore essential, and the general histologic features and immunohistochemically findings can usually differentiate between these tumors, as extracranial meningioma presents with solid nests of meningothelial cells arranged in sheets or whorls with a fibroadipose background[5,13]. Immunohistochemistry is helpful in confirming the diagnosis; extracranial meningiomas tend to show strong positivity towards vimentin and epithelial membrane antigen, as indeed occurred in our patient, and are focally positive for CD99 and Ki-67.
Both CT and magnetic resonance imaging are essential in preoperative surgical planning. Surgery is the only curative treatment, and surgical excision of the mass should be performed if possible. External beam radiation therapy has been shown to be effective and therefore reserved as a palliative approach[16,17]. In the present study, surgical therapy was determined to be the optimal treatment approach for several reasons. The various treatment previously performed on the current patient did not result in an evident recession of the mass. Without surgical intervention, a firm mass and unbearable headache would remain.
The present study reports successful surgical treatment of a patient with a rare primary extracranial meningioma in the maxillary sinus. The present study demonstrated that imaging studies can aid in the diagnosis and biopsy and is useful to specify diagnosis. Surgical treatment is a viable option for the successful management of extracranial meningiomas in the maxillary sinus, and complete postoperative care often requires a multidisciplinary approach.
The authors thank Dr. Aladimi MT from the West China school of Stomatology, Sichuan University (Chengdu, China) for his kind help in the manuscript preparation and for certain important suggestions for the present manuscript.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rizzi A S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
| 1. | El-Daly A, Pitman KT, Ferguson BJ, Snyderman CH. Primary extracranial meningioma of the maxillary antrum. Skull Base Surg. 1997;7:211-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Claus EB, Bondy ML, Schildkraut JM, Wiemels JL, Wrensch M, Black PM. Epidemiology of intracranial meningioma. Neurosurgery. 2005;57:1088-95; discussion 1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 382] [Cited by in RCA: 369] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 3. | Arias Marzán F, de Lucas Carmona G, Alvarez Flórez M, Febles García P. [Extracranial meningiomas of the paranasal sinuses]. Acta Otorrinolaringol Esp. 2010;61:238-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Friedman CD, Costantino PD, Teitelbaum B, Berktold RE, Sisson GA Sr. Primary extracranial meningiomas of the head and neck. Laryngoscope. 1990;100:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 55] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Ho KL. Primary meningioma of the nasal cavity and paranasal sinuses. Cancer. 1980;46:1442-1447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Nager GT, Heroy J, Hoeplinger M. Meningiomas invading the temporal bone with extension to the neck. Am J Otolaryngol. 1983;4:297-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Suárez-Fente V, Llorente-Pendás JL, Gómez-Martínez J, García-González LA, López-Alvarez F, Suárez-Nieto C. Primary tumours of the parapharyngeal space. Our experience in 51 patients. Acta Otorrinolaringol Esp. 2009;60:19-24. [PubMed] |
| 8. | Lingen MW, Rao SM, Hutten MC, Pelzer HJ. Primary ectopic meningioma of the maxillary sinus: case report and review of the literature. Head Neck. 1995;17:258-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Takeshima Y, Kaneko M, Furonaka O, Jeet AV, Inai K. Meningioma in mature cystic teratoma of the ovary. Pathol Int. 2004;54:543-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Nozaki S, Yamazaki M, Koyama T. Primary extracranial meningioma of the maxillary sinus presenting as buccal swelling. Asian J Oral Maxillofac Surg. 2011;23:134-137. [DOI] [Full Text] |
| 11. | Albsoul N, Rawashdeh B, Albsoul A, Abdullah M, Golestani S, Rawshdeh A, Mohammad M, Alzoubi M. A rare case of extracranial meningioma in parapharyngeal space presented as a neck mass. Int J Surg Case Rep. 2015;11:40-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Nur S, Chuang L, Ramaswamy G. Primary extracranial meningioma of the pelvis: a light microscopic, immunohistochemical, and ultrastructural study. Gynecol Oncol. 2006;103:745-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Ouazzani A, de Fontaine S, Berthe JV. Extracranial meningioma and pregnancy: a rare diagnosis. J Plast Reconstr Aesthet Surg. 2007;60:622-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Swain RE Jr, Kingdom TT, DelGaudio JM, Muller S, Grist WJ. Meningiomas of the paranasal sinuses. Am J Rhinol. 2001;15:27-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Maharjan L, Neupane Y, Pradhan B. Primary Atypical Meningioma of the Nasal Cavity: A Case Report and Review of the Literature. Case Rep Otolaryngol. 2018;2018:7541892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Rege ICC, Garcia RR, Mendonça EF. Primary Extracranial Meningioma: A Rare Location. Head Neck Pathol. 2017;11:561-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Lee DH, Sim HS, Hwang JH, Kim KS, Lee SY. Extracranial Meningioma Presenting as an Eyebrow Mass. J Craniofac Surg. 2017;28:e305-e307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Kim CM, Jeon YR, Kim YJ, Chung S. Primary Extracranial Meningioma Presenting as Forehead Mass. Arch Craniofac Surg. 2018;19 (1):55-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |