Published online Oct 6, 2022. doi: 10.12998/wjcc.v10.i28.10332
Peer-review started: June 7, 2022
First decision: June 16, 2022
Revised: July 28, 2022
Accepted: August 25, 2022
Article in press: August 25, 2022
Published online: October 6, 2022
Processing time: 112 Days and 9.3 Hours
Postpartum posterior reversible encephalopathy syndrome (PRES) is not uncommon. Its mechanisms and risk factors are not clear.
A 28-year-old woman underwent cesarean section but had inadvertent dural puncture during epidural anesthesia. To manage the symptoms of intracranial hypotension, crystalloid fluid was infused. However, the patient developed postpartum preeclampsia and PRES. The patient was treated with diazepam and dehydration therapy. The signs of cerebral lesions on magnetic resonance imaging disappeared on postpartum day 7.
Postpartum preeclampsia and PRES can develop concomitantly. Treating postdural puncture headaches with infusion of crystalloid fluid may precipitate the development of PRES.
Core Tip: Posterior reversible encephalopathy syndrome (PRES) is often associated with hypertension and eclampsia. Here, we report a case of postpartum PRES secondary to preeclampsia and intracranial hypotension caused by dural puncture and cerebrospinal fluid leakage. This case highlights the risk of PRES in laboring women with intracranial hypotension secondary to cerebrospinal fluid leakage and hypertension caused by intraspinal anesthesia.
- Citation: Wang Y, Zhang Q. Postpartum posterior reversible encephalopathy syndrome secondary to preeclampsia and cerebrospinal fluid leakage: A case report and literature review. World J Clin Cases 2022; 10(28): 10332-10338
- URL: https://www.wjgnet.com/2307-8960/full/v10/i28/10332.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i28.10332
Posterior reversible encephalopathy syndrome (PRES), also known as reversible posterior leukoencephalopathy syndrome, is characterized by headaches, disturbance of consciousness, epilepsy and visual impairment[1]. Imaging examination may show subcortex edema of the parietooccipital lobe in PRES. It is often associated with hypertension, eclampsia, use of immunosuppressants and systemic lupus erythematosus. PRES is usually reversible with good prognosis, but in some cases it may leave permanent neurological sequelae and even cause death[2].
Here, we report a case of postpartum PRES secondary to preeclampsia and intracranial hypotension caused by dural puncture and cerebrospinal fluid leakage.
A 28-year-old woman suddenly lost consciousness and had general convulsions lasting about 1 min on the second day after cesarean section.
The patient was scheduled for cesarean section under epidural anesthesia using the combined spinal-epidural technique, with an American Society of Anesthesiologists physical status Ⅱ, 69 kg, 159 cm, 40 wk in gestation, and G2P0. The cesarean section was chosen due to social factors. Her prenatal examination and central nervous system examination were unremarkable. No gestational hypertension was noted during pregnancy. Blood routine, coagulation function, and electrocardiography were normal before the operation.
It should be noted that the parturient was very nervous after admission, and often cried and shouted in the ward. The patient fasted on the day of operation. Epidural anesthesia was performed using a one-time lumbar hard joint puncture bag, an internal needle type, a 16 G epidural puncture needle, and a 25 G lumbar anesthesia needle. The L3-L4 gap was selected to perform the combined lumbar and peridural puncture.
When puncturing the lumbar spine, the patient suddenly cried and struggled. We tried to comfort the patient and ease her nervousness. During this chaos, the epidural puncture needle inadvertently entered the subarachnoid cavity at 13:55, although it was withdrawn immediately. Then, lumbar anesthesia was successfully performed at the L2-L3 gap, with 7.5 mg bupivacaine injected into the subarachnoid cavity. The block plane at the beginning of operation was T8-S5. A baby girl was delivered with a weight of 3305 g and an Apgar score of 9 points at one minute after birth. The operation was completed at 14:48. The total volume of bleeding during the operation and on the first postoperative day was estimated to be 50 mL.
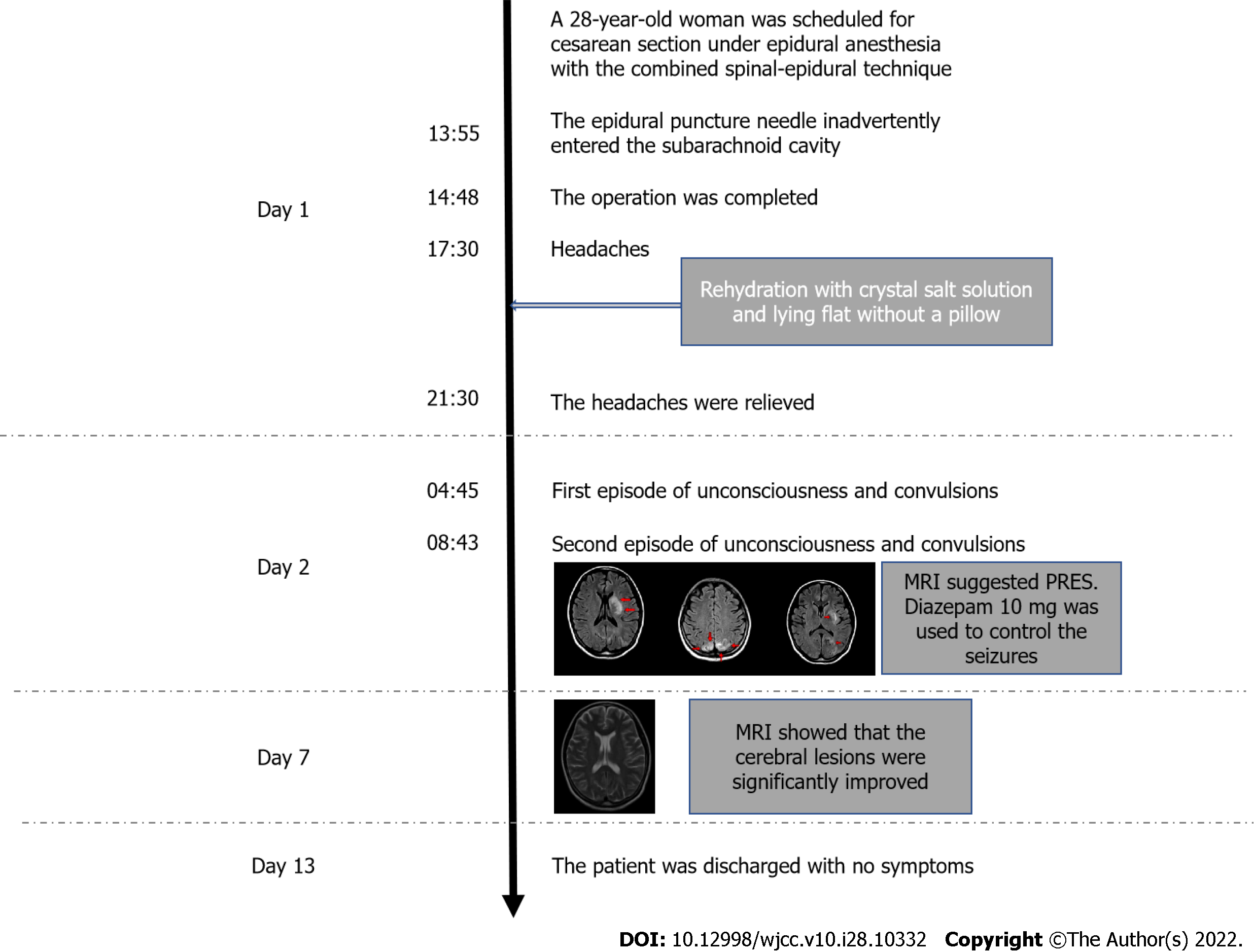
Two and half hours after the delivery at 17:30, the patient complained of headaches. Postdural puncture headaches and intracranial hypotension were suspected. The patient was treated with rehydration with crystal salt solution and lying flat without a pillow. The total volume of intravenous rehydration on the day of operation was 4000 mL, including 500 mL of colloidal solution. The headache was relieved at 21:30. However, several hours later at 04:45 of the next day, the patient suddenly lost consciousness and had general convulsions lasting about 1 min, which occurred again at 08:43 (Figure 1). No symptoms such as nausea, vomiting, or visual disturbances were noticed. Emergent blood biochemistry test showed slightly decreased serum levels of electrolytes, including sodium (135 mmol/L), potassium (3.40 mmol/L), magnesium (0.56 mmol/L), calcium (1.96 mmol/L), and phosphorus (0.63 mmol/L).
The patient has no history of systemic disease.
Her personal and family history was unremarkable.
The patient had newly developed hypertension (160/104 mmHg) and fundus artery spasm. Fundus examination showed fundus artery spasm of Grade I.
She had proteinuria with a level of 103 mg/L and 618 mg/24 h. Considering the evidence of hypertension and proteinuria, a diagnosis of preeclampsia was soon established.
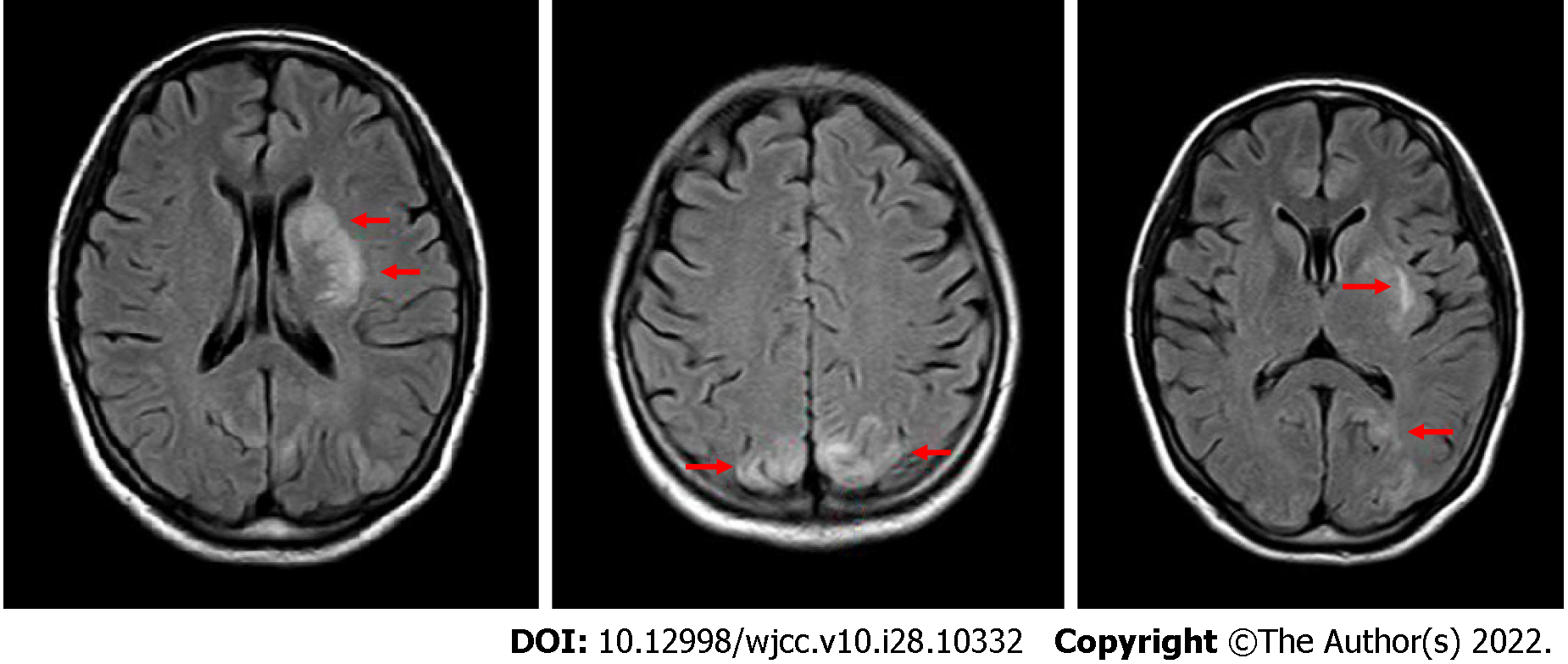
T2-weighted magnetic resonance imaging (MRI) using a fluid-attenuated inversion recovery sequence showed several hyperintensity lesions in the left basal ganglia and the bilateral occipital lobes, suggesting reversible ischemia (Figure 2). The hyaline mesentery and the fifth ventricle were formed. PRES was diagnosed by a neurologist.
The final diagnosis was postpartum PRES resulted from preeclampsia and intracranial hypotension caused by dural puncture and cerebrospinal fluid leakage.
The blood pressure was controlled with oral amlodipine (5 mg daily) at 140-100/90-60 mmHg. The patient ward was dimmed to avoid strong light. To control the seizures, a single dose of diazepam 10 mg was administered intravenously. Dehydration therapy was used to lower the intracerebral pressure. Nutritional neurotherapy was also used.
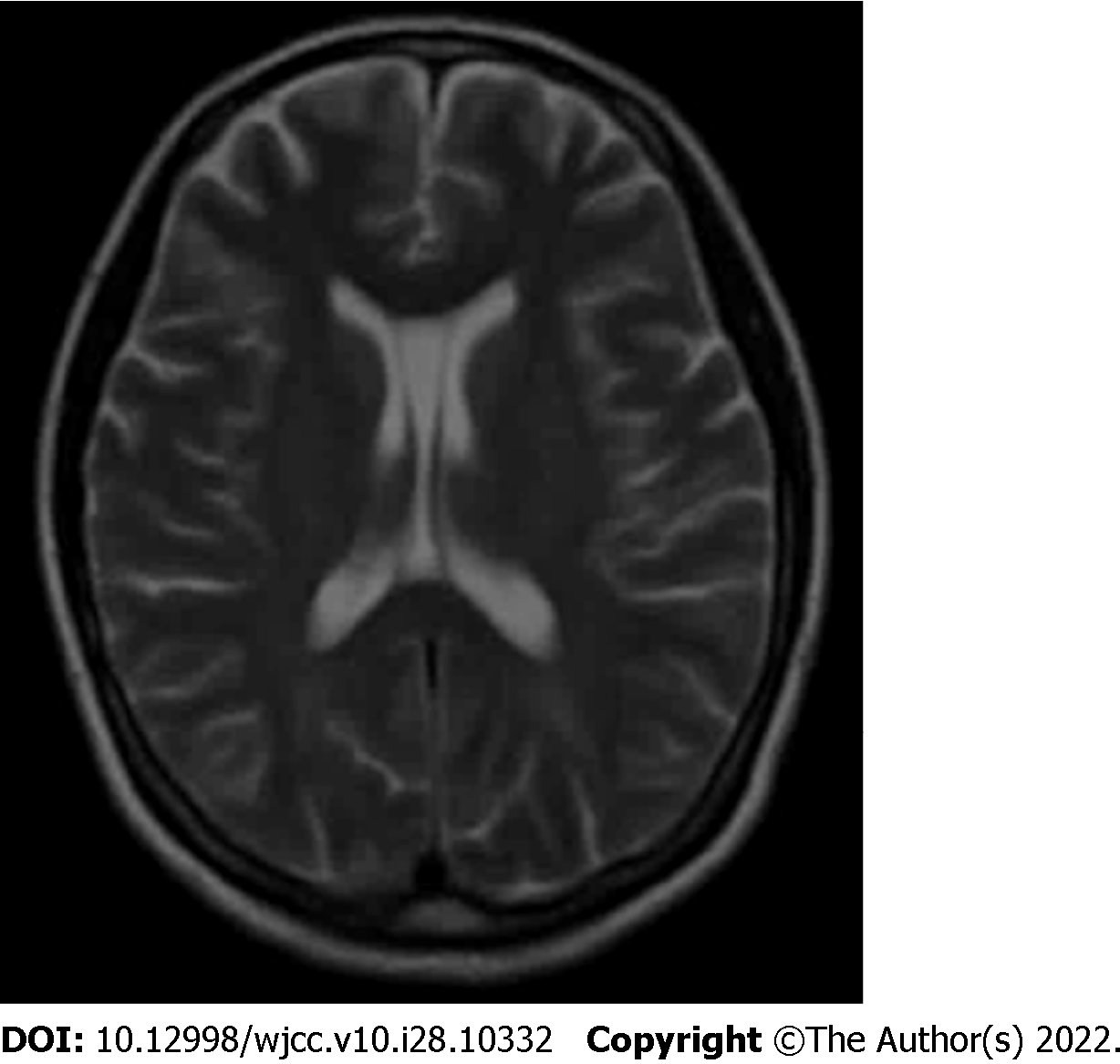
The patient’s blood pressure and urine protein levels gradually returned to normal, and no more seizures had ever occurred. MRI at postpartum day 7 showed that the cerebral lesions in the left basal ganglia and the bilateral occipital lobes were significantly improved (Figure 3). The treatment continued for 12 d. The patient was discharged on postpartum day 13 with no symptoms.
The pathogenesis of PRES is still not clear, and the theory of high perfusion is generally accepted. Blood pressure rises sharply, exceeding the limit of self-regulation mechanism of the small cerebral arteries. The arterioles located in the vascular area of the vertebrobasilar artery were forced to dilate due to hypertension, resulting in high cerebral perfusion. This can break through the blood brain barrier, and the blood protein and liquid penetrate the brain matrix, leading to angiogenic edema. The change of vascular permeability is reversible. Once the disease subsides, it will return to normal within a few weeks. Preeclampsia and cytotoxic drugs can directly lead to endothelial degeneration and dysfunction of the cerebral arterioles, resulting in the above manifestations[3].
PRES is closely related to eclampsia, with similar symptoms of headache and convulsion. Both disorders interact with the changes of cerebrovascular permeability. Wernet et al[4] showed that PRES and eclampsia have a common pathophysiological pathway. PRES may be a part of the pathogenesis of eclampsia[5] and the main damage of the central nervous system in patients with eclampsia. Treatment that prevents or reverses PRES can prevent eclampsia or promote its recovery. It is generally considered that the postpartum period is associated with increased risk of various cerebral disorders, such as reversible cerebral vasoconstriction syndrome (RCVS). PRES and RCVS share similar and even overlapping risk factors, symptoms, and imaging features, and sometimes coexist in the same patient[6].
Our patient was initially diagnosed with postdural puncture headache by an obstetrician and managed accordingly. The diagnosis was made based on the inadvertent epidural puncture and the resultant headache 3 h postoperatively. However, this diagnosis was proven to be wrong because the patient soon developed unconsciousness and convulsions. Although the patient had no gestational hypertension during the prenatal examination, she was diagnosed with preeclampsia based non postpartum proteinuria and fundus examination. The final diagnosis was PRES according to the brain MRI results. However, the blood pressure in this case increased moderately after labor and was soon controlled with medications.
We speculate the mechanism of PRES in our patient was the combination of preeclampsia and intracranial hypotension caused by cerebrospinal fluid (CSF) leakage, which resulted from inadvertent epidural puncture and patient irritation. Mild intracranial hypotension is usually asymptomatic and only causes positional headache. However, persistent intracranial hypotension can lead to vasodilation, damage of the deep vein system[7,8], and eventually brain edema and PRES[9]. In addition, reduced CSF volume in the ventricle can lead to ventricular collapse[10] and traction forces, which may produce mechanical stimulation on the arterial wall and vasospasm[11]. Previous studies have shown vasospasm in the acute phase of PRES[12,13]. All of these changes are associated with expansion of the venous system and the small cerebral arteries, leading to protein and fluid exosmosis, mainly in the vertebrobasilar artery vascular area, which is the typical MRI signs of PRES[8].
To summarize the previous literatures on PRES caused by epidural puncture, we searched PubMed/MEDLINE using the terms "epidural puncture" or "lumbar puncture" or "cerebrospinal fluid leakage" and "PRES" or "RPLS" and found 41 articles. After reviewing these articles, 16 case reports were identified[9,14-28]. These case reports indicate there is a risk of PRES, although very low, in perinatal women, especially those with gestational hypertension and CSF leakage. Despite that PRES is usually reversible, improper treatment may lead to permanent nerve injury or even death[2].
The epidural blood patch is very effective in relieving CSF leakage and should be considered for inadvertent dural puncture in patients with gestational hypertension or primary hypertension. However, our case suggests that infusion of crystalloid fluid for postdural puncture headache in hypertensive patients may carry a risk of brain edema, although that it is often used to increase the production of CSF. In addition, epidural injection of saline and caffeine is also effective in treating postdural puncture headache[29]. If the headache in these patients is not related to the body position, then it may not be caused by CSF leakage. Brain MRI should be performed promptly to exclude PRES for its superiority to CT in imaging soft tissues.
Nicardipine and rabetalol are the first-line drugs for lowing blood pressure in PRES patients[30]. Nimodipine can reduce the infarction rate caused by cerebral vasospasm[31]. Nitroglycerin is not recommended as it can aggravate brain edema[14]. Epilepsy requires immediate treatment to prevent permanent neuronal damage or death[32]. In pregnant women with preeclampsia, magnesium sulfate and barbiturates can effectively prevent and manage seizures.
PRES should be considered in laboring women with intracranial hypotension secondary to cerebrospinal fluid leakage and hypertension caused by intraspinal anesthesia. When treating postdural puncture headaches in patients at risk of PRES, infusion of crystalloid fluid may precipitate the development of PRES.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shiraishi W, Japan; Suh JI, South Korea S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, Pessin MS, Lamy C, Mas JL, Caplan LR. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2250] [Cited by in RCA: 2153] [Article Influence: 74.2] [Reference Citation Analysis (0)] |
| 2. | Stott VL, Hurrell MA, Anderson TJ. Reversible posterior leukoencephalopathy syndrome: a misnomer reviewed. Intern Med J. 2005;35:83-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 195] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 3. | Covarrubias DJ, Luetmer PH, Campeau NG. Posterior reversible encephalopathy syndrome: prognostic utility of quantitative diffusion-weighted MR images. AJNR Am J Neuroradiol. 2002;23:1038-1048. [PubMed] |
| 4. | Wernet A, Benayoun L, Yver C, Bruno O, Mantz J. [Isolated severe neurologic disorders in post-partum: posterior reversible encephalopathy syndrome]. Ann Fr Anesth Reanim. 2007;26:670-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Martin JN Jr, Brewer JM, Blake PG, Owens MY, LaMarca B. PP137. Posterior reversible encephalopathy syndrome (PRES) is a constant component of eclampsia. Pregnancy Hypertens. 2012;2:314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Jeanneret V, Jillella DV, Rangaraju S, Groover O, Peterson R, Koneru S, Nahab F, Kase CS. PRES and RCVS: Two Distinct Entities or a Spectrum of the Same Disease? J Stroke Cerebrovasc Dis. 2022;31:106472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Mokri B. The Monro-Kellie hypothesis: applications in CSF volume depletion. Neurology. 2001;56:1746-1748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 592] [Cited by in RCA: 619] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 8. | Savoiardo M, Minati L, Farina L, De Simone T, Aquino D, Mea E, Filippini G, Bussone G, Chiapparini L. Spontaneous intracranial hypotension with deep brain swelling. Brain. 2007;130:1884-1893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 88] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 9. | Pugliese S, Finocchi V, Borgia ML, Nania C, Della Vella B, Pierallini A, Bozzao A. Intracranial hypotension and PRES: case report. J Headache Pain. 2010;11:437-440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Mercieri M, Mercieri A, Paolini S, Arcioni R, Lupoi D, Passarelli F, Pinto G, Celleno D. Postpartum cerebral ischaemia after accidental dural puncture and epidural blood patch. Br J Anaesth. 2003;90:98-100. [PubMed] |
| 11. | Arutiunov AI, Baron MA, Majorova NA. The role of mechanical factors in the pathogenesis of short-term and prolonged spasm of the cerebral arteries. J Neurosurg. 1974;40:459-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 74] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Henderson RD, Rajah T, Nicol AJ, Read SJ. Posterior leukoencephalopathy following intrathecal chemotherapy with MRA-documented vasospasm. Neurology. 2003;60:326-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 68] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 13. | Dodick DW, Eross EJ, Drazkowski JF, Ingall TJ. Thunderclap headache associated with reversible vasospasm and posterior leukoencephalopathy syndrome. Cephalalgia. 2003;23:994-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Rajan S, Puthenveettil N, Paul J, Kumar L. Posterior reversible encephalopathy syndrome following caesarean section under spinal anaesthesia. Indian J Anaesth. 2014;58:762-765. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Torrillo TM, Bronster DJ, Beilin Y. Delayed diagnosis of posterior reversible encephalopathy syndrome (PRES) in a parturient with preeclampsia after inadvertent dural puncture. Int J Obstet Anesth. 2007;16:171-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Karakis I, Nuccio AH, Amadio JP, Fountain AJ Jr. The Monro-Kellie Doctrine in Action: Posterior Reversible Leukoencephalopathy Syndrome Caused by Intracranial Hypotension from Lumboperitoneal Shunt Placement. World Neurosurg. 2017;98:868.e11-868.e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Doherty H, Hameed S, Ahmed I, Russell IF. Post-dural puncture headache and posterior reversible encephalopathy syndrome: a misdiagnosis or co-presentation? Int J Obstet Anesth. 2014;23:279-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Grelat M, Debaux JB, Sautreaux JL. Posterior reversible encephalopathy syndrome after depletive lumbar puncture: a case report. J Med Case Rep. 2014;8:261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Yoon JE, Lee CY, Kim HW. Posterior Reversible Encephalopathy Syndrome after Head Trauma Surgery in Pediatric Patient without Any Underlying Disease. Korean J Neurotrauma. 2017;13:167-170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Shields LB, Johnson JR, Shields CB. Posterior reversible encephalopathy syndrome following a thoracic discectomy-induced dural leak: case report. J Neurosurg Spine. 2016;25:586-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Shah R, Kubisz-Pudelko A, Reid J. Posterior reversible encephalopathy syndrome following an inadvertent dural puncture during an emergency laparotomy for ischemic colitis - a case report. Local Reg Anesth. 2014;7:1-4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Pradhan A, Jairam A, Kumar RS, Srivastava A, Sreevastava D, Dutta A, Arora S, Bairaria AK, Bhargava A. Posterior reversible encephalopathy syndrome posttransplantation: a case report of possible association with cerebrospinal fluid leak after epidural catheterization. Transplant Proc. 2009;41:1957-1960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Hammad T, DeDent A, Algahtani R, Alastal Y, Elmer L, Medhkour A, Safi F, Assaly R. Posterior Reversible Encephalopathy Syndrome Secondary to CSF Leak and Intracranial Hypotension: A Case Report and Literature Review. Case Rep Neurol Med. 2015;2015:538523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Delgado-López PD, Garcés-Pérez G, García-Carrasco J, Alonso-García E, Gómez-Menéndez AI, Martín-Alonso J. Posterior Reversible Encephalopathy Syndrome with Status Epilepticus Following Surgery for Lumbar Stenosis and Spondylolisthesis. World Neurosurg. 2018;116:309-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Ho CM, Chan KH. Posterior reversible encephalopathy syndrome with vasospasm in a postpartum woman after postdural puncture headache following spinal anesthesia. Anesth Analg. 2007;105:770-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Orehek EK, Burns JD, Koyfman F, Azocar RJ, Holsapple JW, Green DM. Postpartum trifecta: simultaneous eclamptic intracerebral hemorrhage, PRES, and herniation due to intracranial hypotension. Neurocrit Care. 2012;17:434-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Niwa R, Oya S, Nakamura T, Hana T, Matsui T. Rapid intracranial pressure drop as a cause for posterior reversible encephalopathy syndrome: Two case reports. Surg Neurol Int. 2017;8:103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Feil K, Forbrig R, Thaler FS, Conrad J, Heck S, Dorn F, Pfister HW, Straube A. Reversible cerebral vasoconstriction syndrome and posterior reversible encephalopathy syndrome associated with intracranial hypotension. Neurocrit Care. 2017;26:103-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 29. | Katz D, Beilin Y. Review of the Alternatives to Epidural Blood Patch for Treatment of Postdural Puncture Headache in the Parturient. Anesth Analg. 2017;124:1219-1228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 30. | Servillo G, Bifulco F, De Robertis E, Piazza O, Striano P, Tortora F, Striano S, Tufano R. Posterior reversible encephalopathy syndrome in intensive care medicine. Intensive Care Med. 2007;33:230-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 116] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 31. | Euser AG, Cipolla MJ. Magnesium sulfate for the treatment of eclampsia: a brief review. Stroke. 2009;40:1169-1175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 230] [Cited by in RCA: 188] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 32. | Knake S, Hamer HM, Rosenow F. Status epilepticus: a critical review. Epilepsy Behav. 2009;15:10-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |