Published online Oct 6, 2022. doi: 10.12998/wjcc.v10.i28.10326
Peer-review started: May 29, 2022
First decision: June 27, 2022
Revised: July 10, 2022
Accepted: August 25, 2022
Article in press: August 25, 2022
Published online: October 6, 2022
Processing time: 120 Days and 22 Hours
Sinusitis-derived subperiosteal orbital collection is uncommon and is usually diagnosed as subperiosteal orbital abscess or, rarely, as hematoma. We report a unique and even rarer case of subperiosteal orbital collection, which is actually a complication of hematoma and abscess.
A 26-year-old female presented with left eyeball pain and ipsilateral chemosis. She had no history of head trauma or upper respiratory infection. Her blood cell count showed an increase in leukocytes. Fiberoptic rhinolaryngoscopy revealed only mucosal edema of the left olfactory crest without apparent discharge. The computed tomography scan results showed an opaque left posterior ethmoid cell with a thickened bony shell and fusiform changes in the periosteal elevation of the medial wall of the left orbit. Emergent surgery revealed an ethmoid mucocele complicated with subperiosteal orbital hematoma and abscess. The pathology of the lamina papyracea between the mucocele and subperiosteal collection was necrotic, and the overlying mucosa was de-epithelialized.
Subperiosteal orbital hematoma with abscess in a patient with sinusitis adds to the current knowledge of orbital complications of sinusitis.
Core Tip: As a differential diagnosis of subperiosteal orbital collection, subperiosteal orbital hematoma concomitant with abscess needs to be taken into consideration. Surgery is advocated for the diagnosis and treatment of such pathology. This report adds to current knowledge regarding the orbital complications of sinusitis.
- Citation: Hu XH, Zhang C, Dong YK, Cong TC. Subperiosteal orbital hematoma concomitant with abscess in a patient with sinusitis: A case report. World J Clin Cases 2022; 10(28): 10326-10331
- URL: https://www.wjgnet.com/2307-8960/full/v10/i28/10326.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i28.10326
Subperiosteal orbital collection caused by sinus infection is usually diagnosed with subperiosteal orbital abscess (SPOA). In recent years, another diagnostic entity of subperiosteal orbital hematoma that shows clinical manifestations similar to those of SPOA has been sporadically reported in patients with sinusitis or sinus mucocele, and it is believed that the disease could be misdiagnosed as an SPOA if only medically treated[1,2]. Additionally, subperiosteal orbital hematoma mixed with abscess is logically possible when infection spreads to the subperiosteal hematoma. Here, we report a rare condition that was identified in a patient with ethmoid mucocele and subperiosteal orbital collection.
A 26-year-old female presented with left eyeball pain for 2 d (the timeline is shown in Table 1).
| Event | Timeline |
| Presented with left eyeball pain | -2 d |
| Computed tomography showed an opaque left posterior ethmoid cell with thickened bony shell | -1 d |
| Admitted to our department and received endoscopic endonasal sinus surgery | 0 d |
| Free of symptoms | 1 d |
| Patient was discharged | 5 d |
| Surgical cavity was completely epithelialized | 2 mo |
The patient had a left-sided headache two days before the eyeball pain. She was afebrile and did not display diplopia, visual loss, or any discomfort related to her nose.
The patient was otherwise healthy and had no history of head trauma, upper respiratory infection, vascular disease, or coagulation disorder.
The patient had no relevant personal or family history.
Ophthalmologic examination showed periorbital edema and conjunctival chemosis in the left eye. Ocular movements of the same eye were normal in all directions. Funduscopic examination yielded results within the normal range. Fiberoptic rhinolaryngoscopy revealed congestion of the left olfactory mucosa without purulent discharge.
The patient’s white blood cell count was 10400/mm3, and her C-reactive protein level was within the normal range.
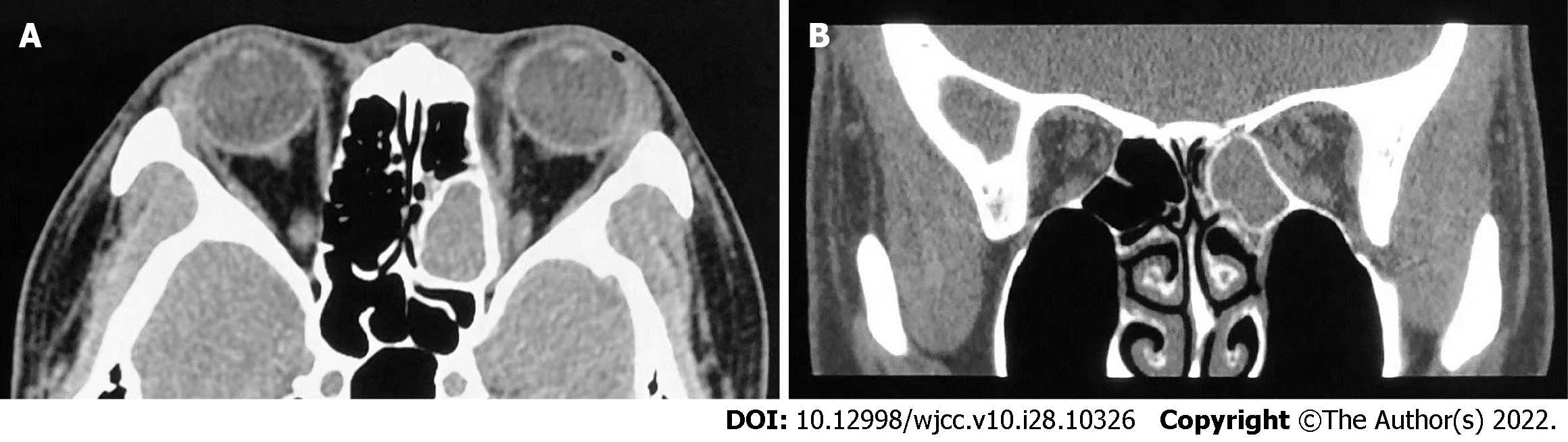
Computed tomography with a soft window showed an opaque left posterior ethmoid cell with a thickened bony shell (Figure 1). In contrast to the cell, the orbital periosteum of the lamina papyracea exhibited fusiform changes with isodensity. The lamina papyracea per se showed no sign of erosion. The medial rectus was oppressed and shifted outwards (Figure 1B).
The final diagnosis of the case was infection of the ethmoid mucocele complicated with subperiosteal orbital collection.
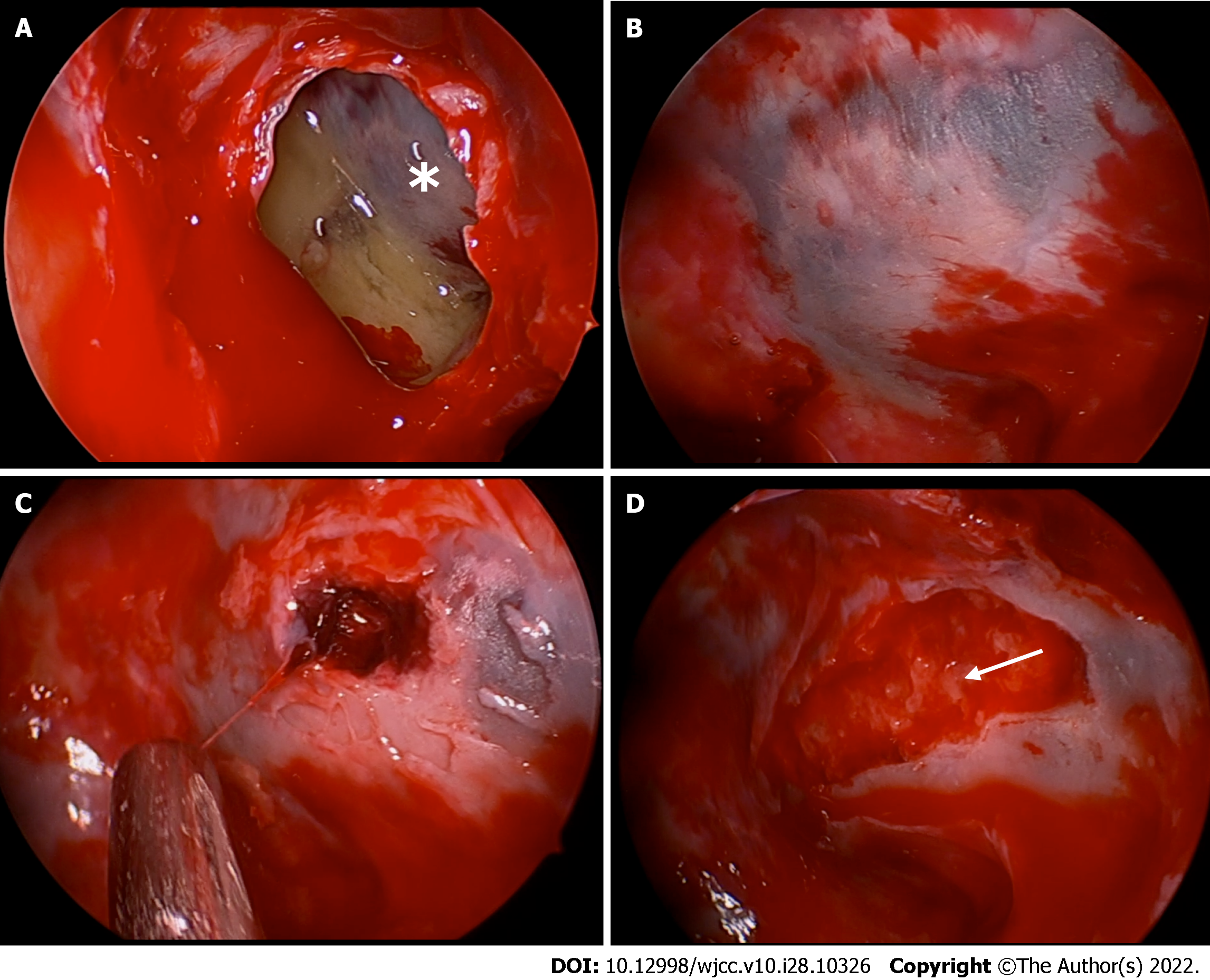
Ceftriaxone was administered intravenously followed by endoscopic endonasal sinus surgery. Mucocele was ascertained, and purulent discharge with some caseous material was aspirated after marsupialization of the opacified posterior ethmoid sinus (Figure 2). The lamina papyracea exposed in the mucocele cavity, surprisingly, showed an altered blue and white area in which the mucosal lining was devascularized (Figure 2A and B). Medial orbital wall decompression was then performed, and a dark blood clot surrounded and even partially covered by pus appeared inside the exposed subperiosteal space, causing the papyracea to take on the specific blue and white hue. The clot appeared to be partially lysed, and it was easily shaped into threads when aspirated (Figure 2C). During the process of decompression, pus mixed with blood subsequently oozed into the ethmoid cavity from around the blood clot (Figure 2D). Complete drainage of the collection was ensured by applying external pressure to the orbit.
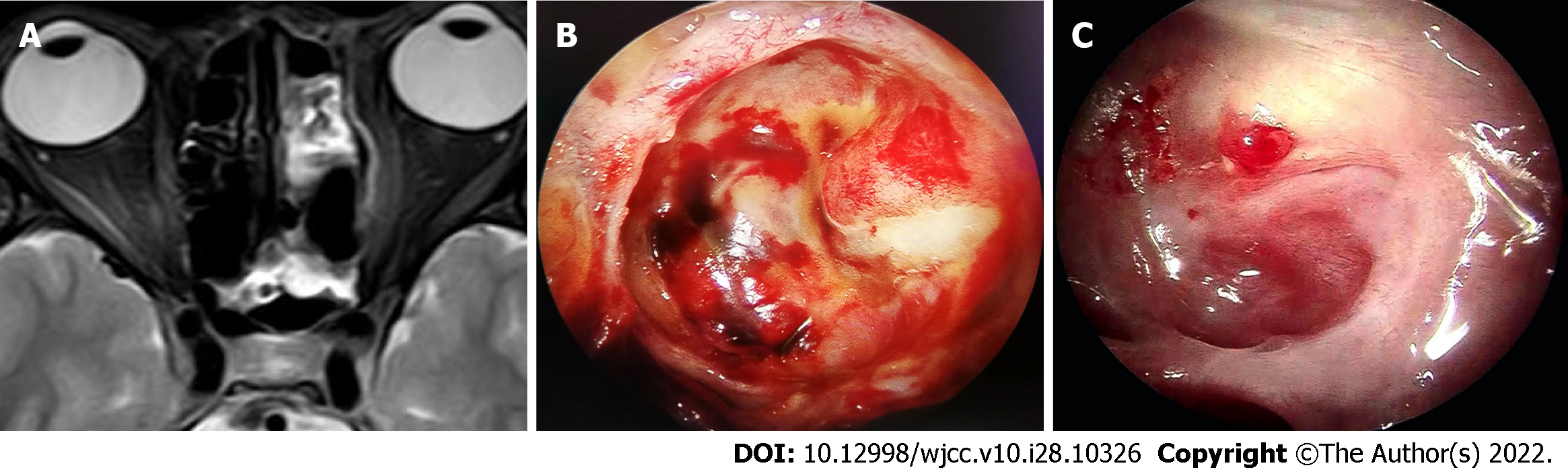
The patient was free of symptoms within 24 h after surgery. Magnetic resonance imaging on postoperative day 5 showed no sign of liquid accumulation in the medial wall of the left orbit (Figure 3A), and the patient was discharged on the same day. Histopathological examination demonstrated de-epithelialized mucosa with bone necrosis of the lamina papyracea. No microorganisms grew from either the subperiosteal orbital or ethmoidal discharges. At two-month follow-up, the surgical cavity was completely epithelialized, and the patient recovered fully (Figure 3B and C).
Orbital complications of sinusitis, according to Chandler’s modified classification, are divided into five groups: preseptal cellulitis, orbital cellulitis, subperiosteal abscess, orbital abscess, and cavernous sinus thrombosis. The most common sinogenic orbital complications appear to originate in the ethmoid sinuses[3-5] and are mainly related to rhinosinusitis or, uncommonly, a mucocele. If not treated in a timely manner, mucocele of the paranasal sinus can induce cranial and/or orbital complications. In addition to direct expansion and compression to the orbit, orbital complications of complicated mucocele can also be caused by infection directly through congenital or acquired bony dehiscence or via the neurovascular foramina or through the local valveless veins of the thin lamina papyracea resulting from thrombophlebitic or embolic conditions[6]. Subperiosteal abscess develops between the orbital bone and periorbita, and up to 90% of SPOA cases are caused by complicated sinusitis[7]. The diagnosis of subperiosteal abscess is mainly based on clinical manifestation and radiographic imaging and is generally confirmed by surgical drainage.
SPOA, however, is only one form of subperiosteal orbital fluid collection that can also present as subperiosteal orbital hematoma. Subperiosteal orbital hematoma is mostly caused by trauma. Nontraumatic subperiosteal orbital hematoma, mostly associated with increased intracranial pressure and bleeding disorders that cause rupture and bleeding of subperiosteal venules[8], is occasionally described in the literature. Sinus infection-related subperiosteal hematoma occurs even more rarely. To date, just over 20 cases of subperiosteal hematoma associated with sinusitis have been surgically identified in the literature, including 4 cases of sinus mucocele[1,2,8,9]. Some authors believed subperiosteal hematoma was an unusual complication of sinusitis. In patients with subperiosteal hematoma associated with sinusitis, no pus was detected, and the results of the hematoma culture were mainly negative.
To the best of our knowledge, this is the first report of subperiosteal orbital hematoma concomitant with abscess occurring in the same potential anatomical space in an adult patient with complicated sinus infection. We postulate that the pathogenesis of this condition probably involves the rupture of small veins crossing between the orbital bony wall and the periorbita due to adjacent sinus inflammation and the subsequent formation of hematoma, the early spread of pathogenic microorganisms directly through the lamina papyracea to involve the subperiosteal orbital space, and the formation of a localized abscess surrounding the blood clot prior to its complete lysis. Concomitant hematoma and abscess in the same area are probably transitory conditions and show the process through which the hematoma evolves completely into an abscess. In our case, the de-epithelialized mucosa of the mucocele and the necrotic change in the lamina papyracea involved might indicate a role of direct extension in the development of a subperiosteal abscess.
Several studies have shown that the age of the patient is an independent risk factor with respect to the choice of treatment for SPOA. Harris found that for patients less than 9 years old without visual impairment, emergent or even urgent surgery was not mandatory as the first-line treatment. Conversely, these patients could be initially administered medical treatment concomitantly with watchful observation. However, in cases of mixed infection with aerobes and anaerobes, which are common in patients more than 9 years old, operative intervention should be initially performed[10,11]. For adult patients with SPOA, endoscopic endonasal sinus surgery is currently advocated as the first choice of treatment due to its advantages of minimal invasion, no facial scarring, and shortened hospital course compared with the external orbital approach. Ethmoidectomy usually suffices when obvious dehiscence of the lamina papyracea is apparent[12]. If dehiscence is not detected during the surgery, the lamina papyracea should be opened for drainage. However, there is controversy regarding the extent of removal of the lamina papyracea. In the early days of endoscopic sinus surgical practice, the lamina papyracea was cracked but not removed[12], or swang back and then medialized in a “swing door” pattern[13], or partially resected[14]. Recently, wide removal of the lamina papyracea with complete ethmoidectomy was performed with satisfactory results[15]. The rationale for wide resection was supported by a report by Ragab et al[6]. In their report, bone sequestrum was identified in all eight cases with the presence of cocci in half; this explained the failure of medical treatment and the necessity for surgery.
In the case reported here, sequestrum was observed histologically with no pathogens identified, in concordance with the cases reported by Eviatar et al[5], who observed bone destruction and resorption in the lamina papyracea in five of nine children with acute rhinosinusitis and SPOA. These pathological findings strengthen the theory of direct spread for the pathogenesis of SPOA.
As an approach to diagnosing and treating subperiosteal abscess in patients with sinus mucocele, surgical intervention is advocated, consistent with the treatment modality recommended for cases of subperiosteal orbital hematoma caused by sinus infection. The recovery from subperiosteal hematoma and abscess in the case reported here was uneventful after the surgery.
Subperiosteal orbital hematoma concomitant with abscess in patients with sinusitis has not been reported previously. It can cause necrotic bony changes, indicating a need for timely surgical intervention.
We thank the patient for participating in the report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Otorhinolaryngology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cerwenka H, Austria; Lim SC, South Korea S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Park HW, Lee BJ, Chung YS. Orbital subperiosteal hematoma associated with sinus infection. Rhinology. 2010;48:117-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Mozaffari M, Boyd E, Whiteside O. Subperiosteal haematoma of the orbit secondary to frontal sinusitis. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Sciarretta V, Demattè M, Farneti P, Fornaciari M, Corsini I, Piccin O, Saggese D, Fernandez IJ. Management of orbital cellulitis and subperiosteal orbital abscess in pediatric patients: A ten-year review. Int J Pediatr Otorhinolaryngol. 2017;96:72-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 4. | Schulte DL, Kasperbauer JL. Safety of paranasal sinus surgery in patients with cystic fibrosis. Laryngoscope. 1998;108:1813-1815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Eviatar E, Sandbank J, Kleid S, Gavriel H. The role of osteitis of the lamina papyracea in the formation of subperiosteal orbital abscess in young children. Int J Pediatr Otorhinolaryngol. 2014;78:2267-2270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Ragab A, Samaka RM. Is pyogenic ethmoidal osteitis the cause of complicated rhinosinusitis with subperiosteal orbital abscess? Eur Arch Otorhinolaryngol. 2010;267:1231-1237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Erickson BP, Lee WW. Orbital Cellulitis and Subperiosteal Abscess: A 5-year Outcomes Analysis. Orbit. 2015;34:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | McNab AA. Nontraumatic orbital hemorrhage. Surv Ophthalmol. 2014;59:166-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Woo KI, Kim YD. Subperiosteal hematoma of the orbit associated with sinusitis. Korean J Ophthalmol. 1997;11:118-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Liao JC, Harris GJ. Subperiosteal abscess of the orbit: evolving pathogens and the therapeutic protocol. Ophthalmology. 2015;122:639-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Garcia GH, Harris GJ. Criteria for nonsurgical management of subperiosteal abscess of the orbit: analysis of outcomes 1988-1998. Ophthalmology. 2000;107:1454-6; discussion 1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 148] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 12. | Manning SC. Endoscopic management of medial subperiosteal orbital abscess. Arch Otolaryngol Head Neck Surg. 1993;119:789-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 46] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Malik V, Khwaja S, De Carpentier J. Immediate lamina papyracea reconstruction during endoscopic sinus surgery for surgically managed subperiosteal abscess in children. Laryngoscope. 2006;116:835-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Froehlich P, Pransky SM, Fontaine P, Stearns G, Morgon A. Minimal endoscopic approach to subperiosteal orbital abscess. Arch Otolaryngol Head Neck Surg. 1997;123:280-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Gavriel H, Jabarin B, Israel O, Eviatar E. Conservative Management for Subperiosteal Orbital Abscess in Adults: A 20-Year Experience. Ann Otol Rhinol Laryngol. 2018;127:162-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |