Published online Oct 6, 2022. doi: 10.12998/wjcc.v10.i28.10279
Peer-review started: May 15, 2022
First decision: June 8, 2022
Revised: June 21, 2022
Accepted: August 25, 2022
Article in press: August 25, 2022
Published online: October 6, 2022
Processing time: 134 Days and 22.8 Hours
Schwannoma is a benign tumor originating from the peripheral nerve sheath. The clinical symptoms of tracheal schwannoma depend on the location of the tumor, and the most common clinical symptoms are cough and hemoptysis. The most effective treatment for benign tumors is complete resection of the primary lesion at an early stage. Our experience has demonstrated that primary tracheal schwannoma can be safely excised with a high-frequency electric knife in a minimally invasive manner.
We report a 61-year-old asymptomatic woman who underwent chest computed tomography (CT), which accidentally found an intraluminal tracheal mass without enlarged lymph nodes. Then, the patient underwent bronchoscopy, which found that the tracheal mass originated from the left wall of the upper trachea, was less than 1.5 cm in size, immovable, smooth and 4 cm away from the vocal cord, resulting in partial upper respiratory tract obstruction. Treatment was performed using an endoscopic resection for en bloc removal of the tracheal mass. The diagnosis was primary tracheal schwannoma. A follow-up was performed after endoscopic surgery, and bronchoscopy and thoracic CT were used to monitor whether there was a recurrence. At present, there is no evidence of recurrence, and the patient had a good quality of life. Endoscopic resection may be effective and safe in the treatment of primary tracheal schwannoma.
Primary tracheal schwannoma is a very rare benign tumor. In this case, we cured it by complete endoscopic resection.
Core Tip: We report a case diagnosed with primary tracheal schwannoma using endoscopic resection. Primary tracheal schwannoma is an extremely rare benign tumor of trachea. To the best of our knowledge, only a few cases have previously been reported. Cough and hemoptysis are common in this disease, but many patients are misdiagnosed as having asthma. Our experience shows that primary tracheal schwannoma can be safely and completely resected by a high-frequency electric knife in a minimally invasive manner.
- Citation: Shen YS, Tian XD, Pan Y, Li H. Treatment of primary tracheal schwannoma with endoscopic resection: A case report. World J Clin Cases 2022; 10(28): 10279-10285
- URL: https://www.wjgnet.com/2307-8960/full/v10/i28/10279.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i28.10279
Primary tracheal tumors are uncommon[1,2]. It is estimated that approximately 0.2% of the entire respiratory system is occupied by primary tracheal tumors in the United States, and most of them are malignant[3]. Among them, primary tracheal schwannoma accounts for less than 0.5% of primary tracheal tumors[4,5]. There are two distinct types of primary tracheal schwannomas, schwannomas and neurofibromas, which arise from nerves located inside the trachea. As an extremely rare tumor with nonspecific symptoms and is sometimes misdiagnosed as asthma[6,7]. Less invasive endoscopic procedures can now be used to resect tumors that previously required surgery[8,9]. We herein present a rare case of a primary tracheal schwannoma with a high-frequency electric knife in a minimally invasive manner. In addition, we retrieved related literature found four primary tracheal schwannoma cases treated by endoscopic therapy that are reported in the literature in Table 1[7,9-11].
| Characters | Ge etal[7] | Gibb etal[10] | Sharma etal[9] | Horovitz etal[11] |
| Population | China | China | United States | NA |
| Age | 53 | 16 | 63 | 38 |
| Sex | M | F | M | F |
| Clinical presentation | Cough, expectoration | Cough, asthma | Dyspnea | NA |
| Location | Distal trachea | Distal trachea | Proximal trachea | NA |
| Size | 2.0 cm | NA | 2.0 cm | NA |
| Treatment | APC/electrocautery | APC/electrocautery | APC/electrocautery | Endoscopic excision |
| Prognosis | Recurrence, 2 wk after endoscopic resection | Uneventful for 18 mo | Uneventful for 8 mo | Recurrence, 12 yr after endoscopic resection |
There were no complaints from the patient.
A 61-year-old woman with no history of chronic pulmonary disease was referred from the department of chest surgery for diagnosis and treatment of an accidental pulmonary nodule. She was a nonsmoker. No abnormal results were found in physical examinations or biochemical tests.
There was no relevant medical history for the patient.
The patient has no noteworthy family history. There was no family history of cancer in the patient's family. The patient's family members had no smoking history.
A physical examination revealed no clinically significant changes.
No abnormalities were noted on laboratory examinations.
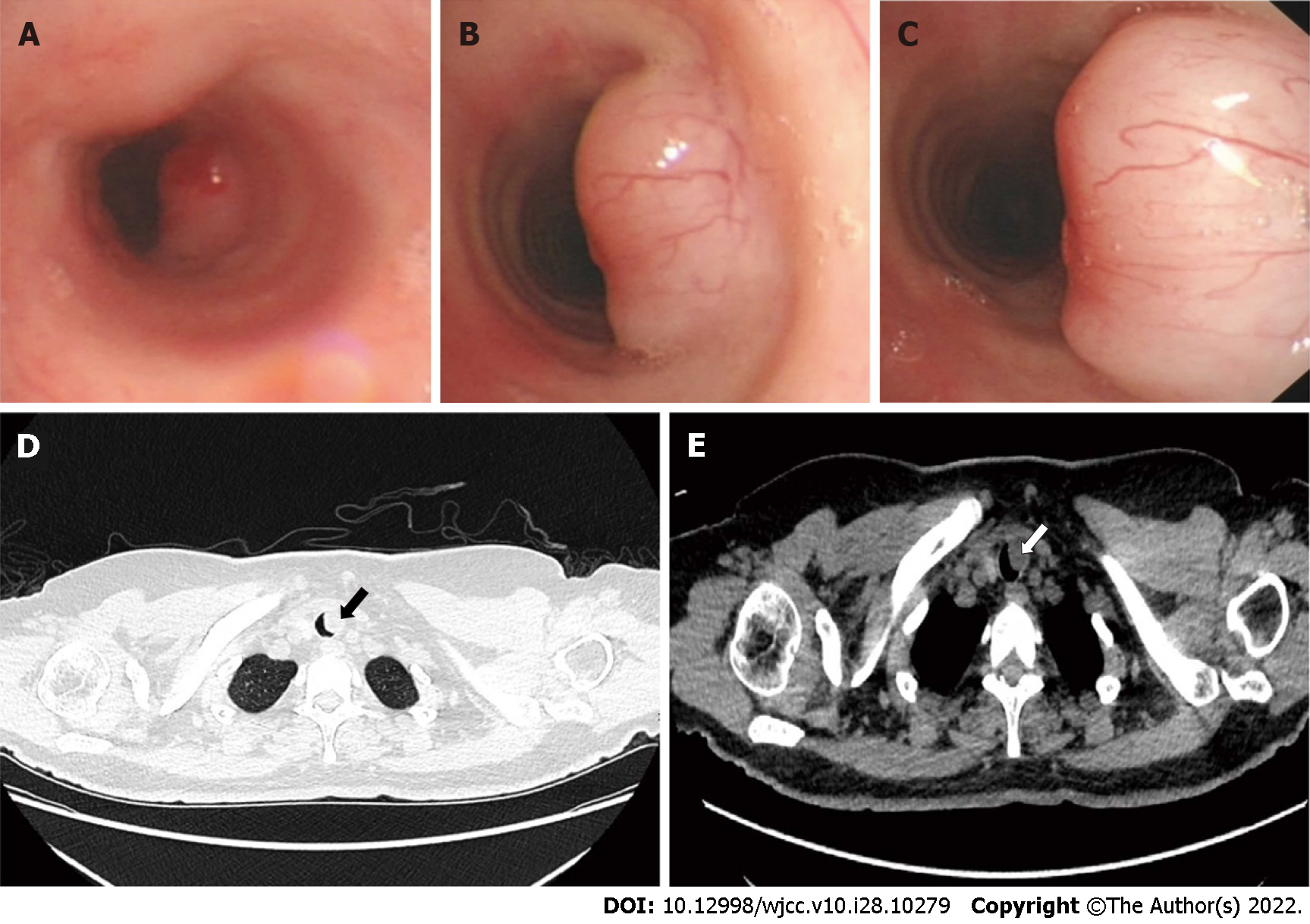
A bronchoscopy was performed, which confirmed that the lesion originated from the left wall of the upper trachea. The mass was less than 1.5 centimeters in size, immobile, smooth and 4 centimeters distal to the vocal cords, leading to partial upper airway obstruction (Figure 1A-C). A computed tomography (CT) scan of the chest revealed an intraluminal tracheal mass without enlarged lymph nodes (Figure 1D and E). Chest CT was performed and suggested the existence of a nodule on the left wall of the trachea at the entrance to the thoracic cavity, considering benign lesions.
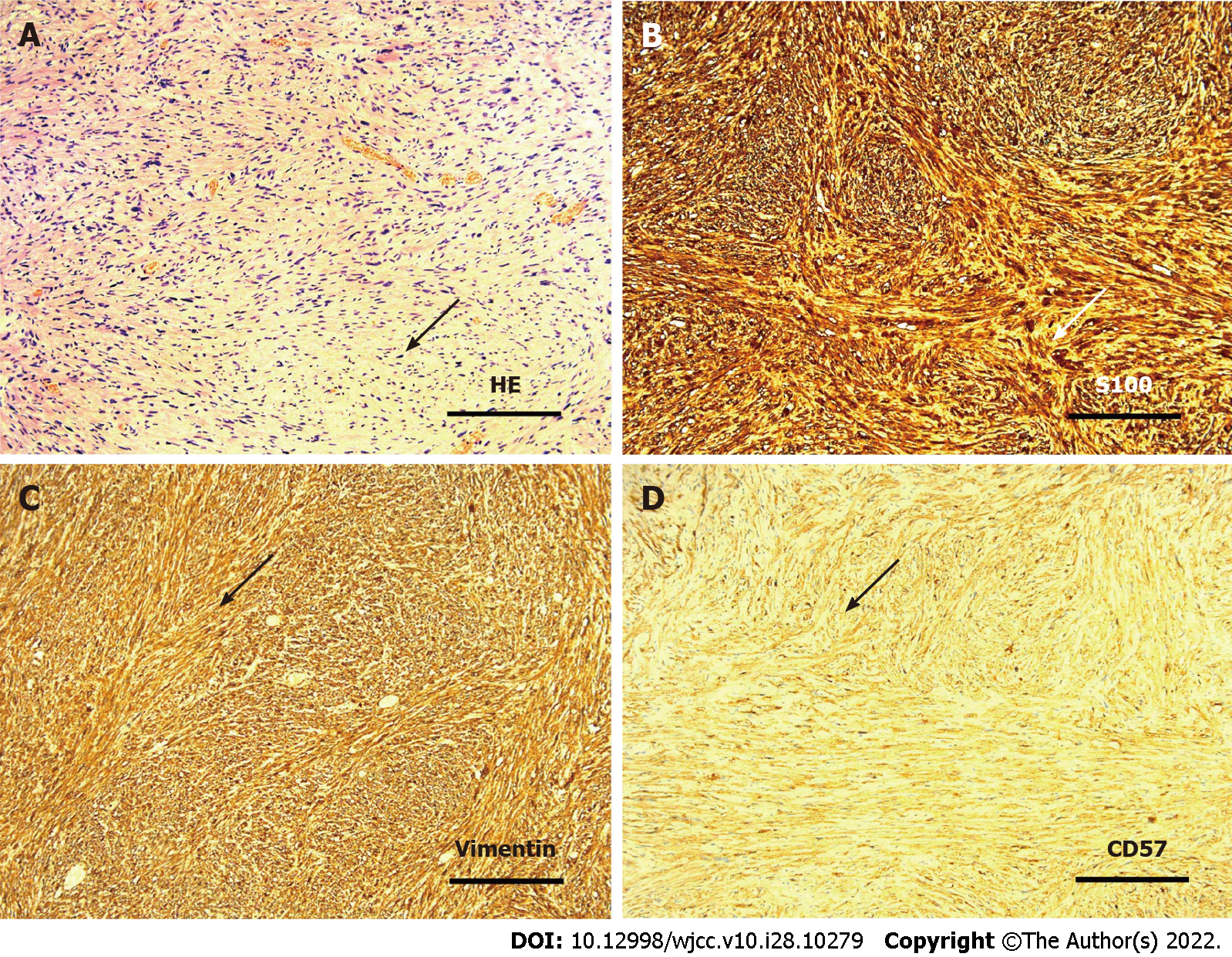
Pathological examination confirmed a spindle cell neoplasm with schwannoma features (Figure 2).
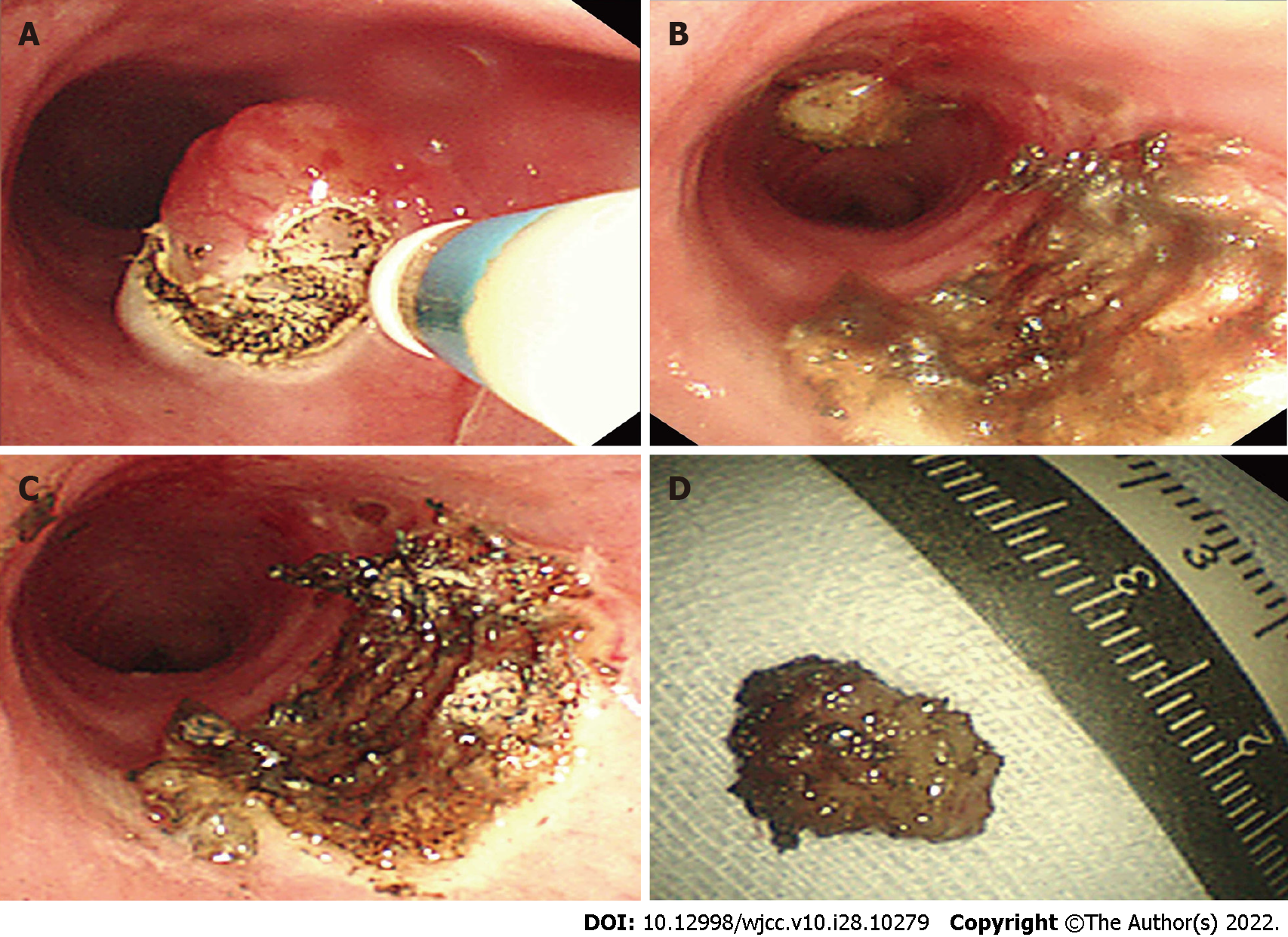
The patient underwent endoscopic excision within 25 min. A BF TYPE 1T260 bronchoscope (Olympus, Tokyo, Japan) was used for the operation, and VIO200D (ERBE, Germany) was selected as the electrosurgical generator, with cutting set to the endo-cut mode (effect 3, duration 1, interval 5) and electrocoagulation set to the forced-coagulation mode (effect 3, 30 W).
The patient was positioned in a supine posture under intravenous anesthesia (propofol and fentanyl). Based on the measurement of blood oxygen saturation, intermittent mask oxygen inhalation was administered with an oxygen flow rate of 0-10 L/min, and the density of oxygen was controlled within a safe range. The mass was approximately 1.0 cm in diameter and involved the left side of the tracheal wall. Incision, stripping and hemostasis through the basal part of the tumor was conducted with a disposable high-frequency cutting tool (Olympus, KD-650U) rather than an endoloop. No obvious hemorrhage or edema existed (Figure 3).
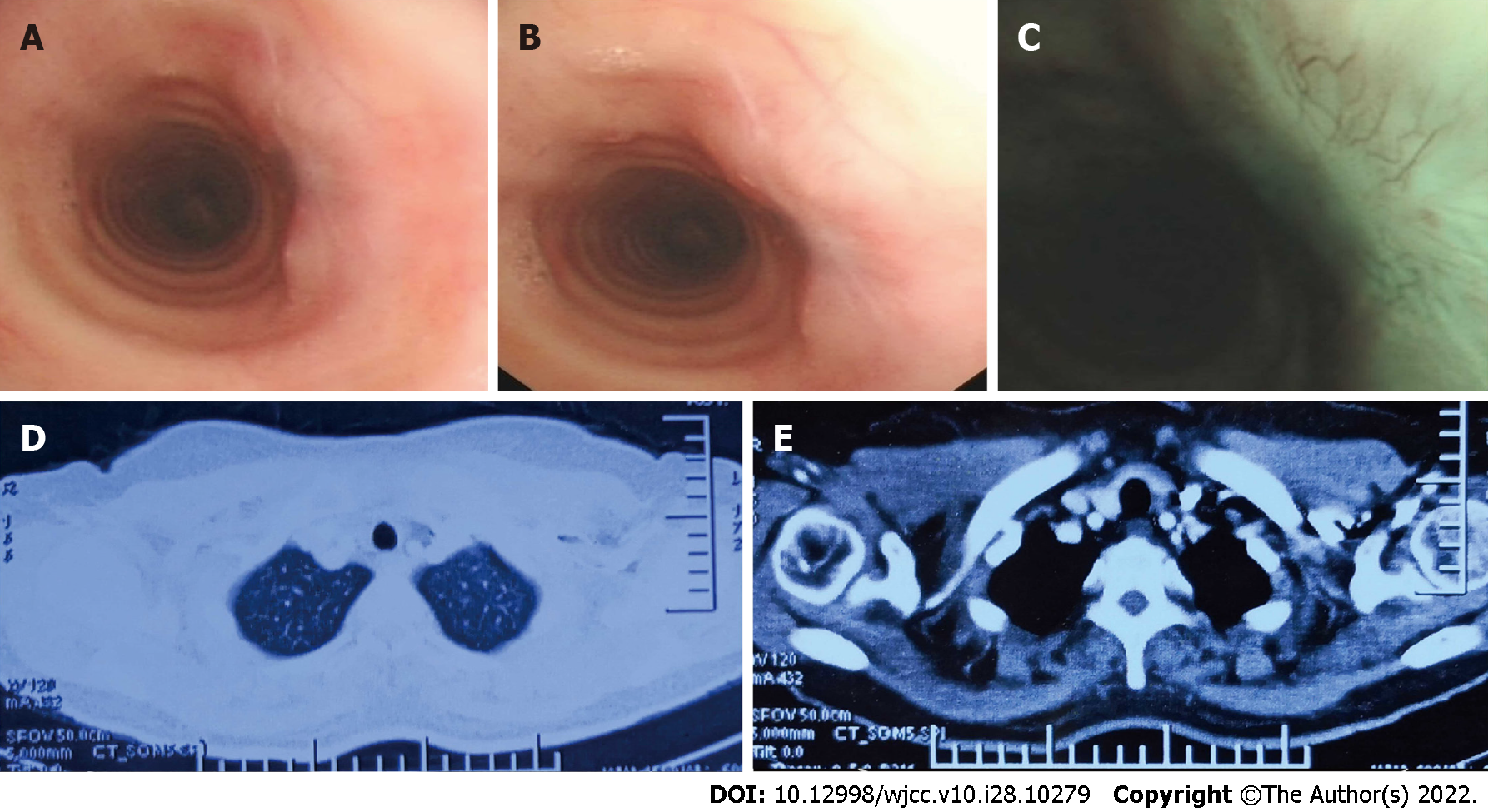
Bronchoscopy and CT were reviewed two months later, and a scar had formed without recurrence (Figure 4). The patient has recovered well and remains free of disease.
Tracheal schwannoma was first reported in 1951 and originates from Schwann cells of the intraluminal sheath; it commonly occurs in the distal trachea with a female sex predilection and excellent prognosis[4]. There are no pathogenic factors known to cause primary tracheal schwannoma, and how it develops is unclear. Fortunately, a previous study on the genomic landscape of schwannoma showed that the common genomic aberrations in sporadic schwannoma are NF2, ARID1A, ARID1B, and DDR1. The fusion expression of SH3PXD2A-HTRA1 leads to an increase in phosphorylated ERK, increasing proliferation, invasion, and tumorigenesis in vivo[12]. This study could provide a potential therapeutic strategy for the treatment of schwannoma.
The clinical presentation of schwannoma is determined by the site of tumor origin, disease extent, degree of airway obstruction, and lung function damage. Patients with this disease can be asymptomatic, with the disease being diagnosed by chance after a routine medical examination. Cough and hemoptysis are often observed in the disease[13]. Unfortunately, many patients are misdiagnosed as having asthma[7].
Chest CT or magnetic resonance imaging (MRI) plays an important role in the accurate diagnosis of tracheal tumors[5]. On radiographic examination, the lesion often shows well-defined boundaries, and the tumor surface is usually smooth, without surrounding structure invasion[14]. Flexible bronchoscopy is employed not only for direct tumor visualization but also for biopsy and resection[2]. Immunohistochemical analysis reveals positivity for S-100 protein and Vimentin, confirming the diagnosis of schwannoma[13,15].
Complete resection of a tracheal schwannoma is the gold standard of treatment. There are a variety of treatment methods, including tracheal resection and minimally invasive treatment[13,16]. In the present case, considering the sessile tumor without extraluminal lesions and the low risk of tracheal fistula, we preferred endoscopic excision. A high-frequency electric knife is commonly used in the treatment of early esophageal and gastroenteric tumors in endoscopic resection[17]; however, there are no available data regarding its use, or its effectiveness and safety in the management of tracheal masses. In our case, we first reported a novel method of en bloc removal of a tracheal mass, complying with oncological requirements. This method is safe since the two major security elements of the resection are under control, including the density of oxygen and the operation depth. In addition, shorter operation time and less bleeding volume are two other advantages compared with traditional primary tracheal resection. Potential complications of tracheal resection would be avoided, thus benefitting the clinical outcome.
However, this study has some limitations. One limitation is the short follow-up time. Although no significant difference exists in the quality of life pre- and postoperation, local recurrence in endoscopic excision has been previously reported, suggesting that bronchoscopic surveillance is necessary[11]. Another limitation is the limited number of cases. As a result, the long-term effects require further patient follow-up.
Primary tracheal schwannoma is an extremely rare benign tumor that can be cured with complete endoscopic excision.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Faraji N, Iran; Li Y, China; Vyshka G, Albania; Yeh CY, Taiwan S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Urdaneta AI, Yu JB, Wilson LD. Population based cancer registry analysis of primary tracheal carcinoma. Am J Clin Oncol. 2011;34:32-37. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in Crossref: 93] [Cited by in RCA: 111] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 2. | Hao ZR, Yao ZH, Zhao JQ, Li DZ, Wan YY, Kang YM, Lin DJ. Clinical efficacy of treatment for primary tracheal tumors by flexible bronchoscopy: Airway stenosis recanalization and quality of life. Exp Ther Med. 2020;20:2099-2105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited in This Article: 2] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Gaissert HA, Mark EJ. Tracheobronchial gland tumors. Cancer Control. 2006;13:286-294. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in Crossref: 86] [Cited by in RCA: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 4. | Righini CA, Lequeux T, Laverierre MH, Reyt E. Primary tracheal schwannoma: one case report and a literature review. Eur Arch Otorhinolaryngol. 2005;262:157-160. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Hamdan AL, Moukarbel RV, Tawil A, El-Khatib M, Hadi U. Tracheal schwannoma: a misleading entity. Middle East J Anaesthesiol. 2010;20:611-613. [PubMed] [Cited in This Article: 2] |
| 6. | Afsin E, Yaksi O, Önal A, Bacaksiz E. Tracheal schwannoma mimicking asthma. Int J Neurosci. 2022;1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Ge X, Han F, Guan W, Sun J, Guo X. Optimal treatment for primary benign intratracheal schwannoma: A case report and review of the literature. Oncol Lett. 2015;10:2273-2276. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 4] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Xia C, Liu M, Niu X, Li X, Chen J. Molecular Features of a Primary Transmural Tracheal Schwannoma: Clinical Experience and Review of the Literature. Cancer Manag Res. 2022;14:1125-1129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited in This Article: 1] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Sharma PV, Jobanputra YB, Perdomo Miquel T, Schroeder JR, Wellikoff A. Primary intratracheal schwannoma resected during bronchoscopy using argon plasma coagulation. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 3] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Gibb AP, Sivaraman B. A second case of foul smelling urine in a boy caused by Aerococcus urinae. Pediatr Infect Dis J. 2013;32:1300-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Horovitz AG, Khalil KG, Verani RR, Guthrie AM, Cowan DF. Primary intratracheal neurilemoma. J Thorac Cardiovasc Surg. 1983;85:313-317. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 3] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Agnihotri S, Jalali S, Wilson MR, Danesh A, Li M, Klironomos G, Krieger JR, Mansouri A, Khan O, Mamatjan Y, Landon-Brace N, Tung T, Dowar M, Li T, Bruce JP, Burrell KE, Tonge PD, Alamsahebpour A, Krischek B, Agarwalla PK, Bi WL, Dunn IF, Beroukhim R, Fehlings MG, Bril V, Pagnotta SM, Iavarone A, Pugh TJ, Aldape KD, Zadeh G. The genomic landscape of schwannoma. Nat Genet. 2016;48:1339-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in Crossref: 99] [Cited by in RCA: 95] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 13. | Han DP, Xiang J, Ye ZQ, He DN, Fei XC, Wang CF, Che JM, Hang JB, Li HC. Primary tracheal schwannoma treated by surgical resection: a case report. J Thorac Dis. 2017;9:E249-E252. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 3] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Parsons RB, Milestone BN, Adler LP. Radiographic assessment of airway tumors. Chest Surg Clin N Am. 2003;13:63-77, v. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Jung YY, Hong ME, Han J, Kim TS, Kim J, Shim YM, Kim H. Bronchial schwannomas: clinicopathologic analysis of 7 cases. Korean J Pathol. 2013;47:326-331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited in This Article: 1] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Hamouri S, Novotny NM. Primary tracheal schwannoma a review of a rare entity: current understanding of management and followup. J Cardiothorac Surg. 2017;12:105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited in This Article: 1] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Gambitta P, Iannuzzi F, Ballerini A, D'Alessandro A, Vertemati M, Bareggi E, Pallotta S, Fontana P, Aseni P. Endoscopic submucosal dissection versus endoscopic mucosal resection for type 0-II superficial gastric lesions larger than 20 mm. Ann Gastroenterol. 2018;31:338-343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited in This Article: 1] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |