Published online Oct 6, 2022. doi: 10.12998/wjcc.v10.i28.10220
Peer-review started: April 23, 2022
First decision: June 8, 2022
Revised: June 21, 2022
Accepted: August 15, 2022
Article in press: August 15, 2022
Published online: October 6, 2022
Processing time: 156 Days and 20.2 Hours
Otogenic brain abscess caused by middle ear cholesteatoma is a potentially serious and life-threatening complication in the ear, nose, and throat clinic. The mortality rate associated with otogenic brain abscesses is 8%–26.3%. Recently, in China, the incidence of brain abscess secondary to middle ear cholesteatoma has started to increase due to antibiotic resistance.
A 55-year-old male presented hearing loss in the right ear and headache for 1 mo in 2018. Computed tomography (CT) showed an area of low density in the right middle ear and mastoid and auditory ossicle defects and a small amount of soft tissue density in the left middle ear. The parietal wall of the right tympanic cavity and the posterior wall of the mastoid sinus were thin and less continuous. Cranial magnetic resonance imaging revealed an area of low intensity encapsulated by an area of high intensity in the right temporal lobe. We diagnosed him with a brain abscess secondary to middle ear cholesteatoma. He received surgery to drain the abscess followed by a modified radical mastoidectomy. The patient visited our department 3 years later because of intermittent otorrhea in the left ear. CT revealed that the area of the soft tissue density in the left middle ear and mastoid was significantly increased. The posterior wall of the mastoid sinus was destroyed, leaving the left middle ear connecting with the brain. The patient underwent a modified radical mastoidectomy in the left ear
Regular follow-up and timely treatment of contralateral ear disease are vital for the prevention of otogenic complications in patients with otogenic abscesses secondary to middle ear cholesteatoma in the unilateral ear.
Core Tip: There are few studies about the occurrence of a cholesteatoma in the contralateral ear in patients with otogenic brain abscess secondary to cholesteatoma in the unilateral ear. Here, we report a case of cholesteatoma in the contralateral ear with the destruction of the posterior wall of the mastoid sinus three years after curing middle ear cholesteatoma complicated with an otogenic intracranial abscess in the unilateral ear, reminding us of the importance of the detailed examination in regular follow-up and timely treatment.
- Citation: Zhang L, Niu X, Zhang K, He T, Sun Y. Potential otogenic complications caused by cholesteatoma of the contralateral ear in patients with otogenic abscess secondary to middle ear cholesteatoma of one ear: A case report. World J Clin Cases 2022; 10(28): 10220-10226
- URL: https://www.wjgnet.com/2307-8960/full/v10/i28/10220.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i28.10220
Middle ear cholesteatoma is a benign collection of keratinized epithelium within the middle ear, most of which results from under aeration of the middle ear cleft. It is the most severe middle ear disease and may lead to intra- and extracranial complications. Cholesteatoma in the middle ear can erode and destroy the temporal bone; thus, the infection may spread to the cranial cavity. Brain abscess is a life-threatening complication, and otogenic intracranial abscesses are most commonly caused by a chronic ear infection with cholesteatoma[1]. Recently, in China, the incidence of brain abscess secondary to middle ear cholesteatoma has started to increase due to antibiotic resistance. The main treatment for brain abscesses is surgical intervention combined with anti-infection medication and supportive treatment. The surgical procedure is based on the patient’s general condition, the location of the brain abscess, and the efficacy of antibiotics. However, the ideal sequence of surgical intervention is still debated, for example, performing surgery on the brain abscess first or performing otological surgery and neurosurgery at the same time. To our knowledge, most patients underwent surgery for brain abscesses first. This article reports a case in which the patient had a middle ear cholesteatoma with the posterior wall of the mastoid sinus defect in the left ear 3 years after curing a middle ear cholesteatoma complicated with a brain abscess in the right ear.
In October 2021, a 55-year-old male presented with intermittent otorrhea in the left ear.
The patient’s symptoms started a month ago with intermittent otorrhea in the left ear. His hearing in the left ear was poor. He had no complaints of the right ear.
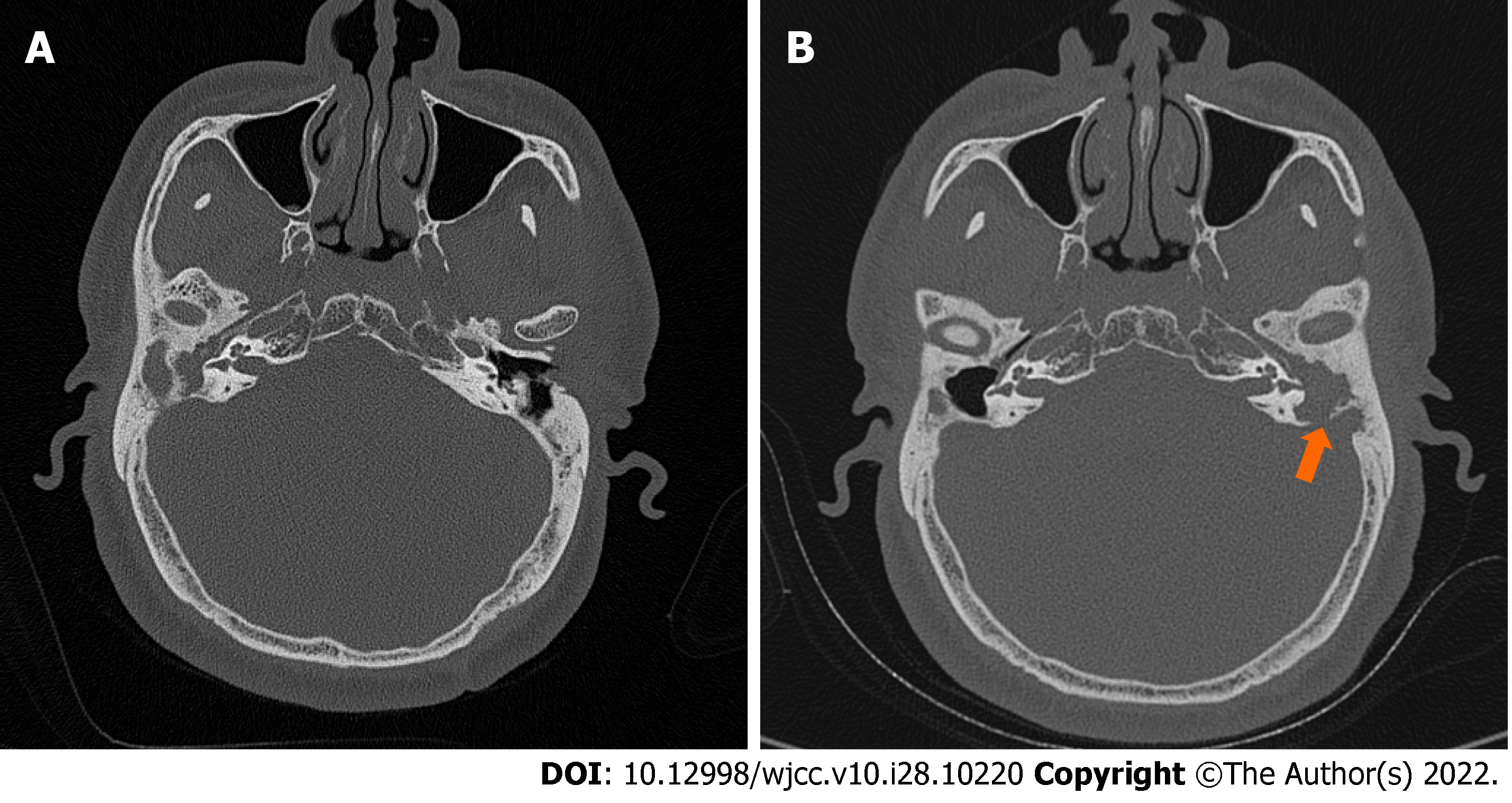
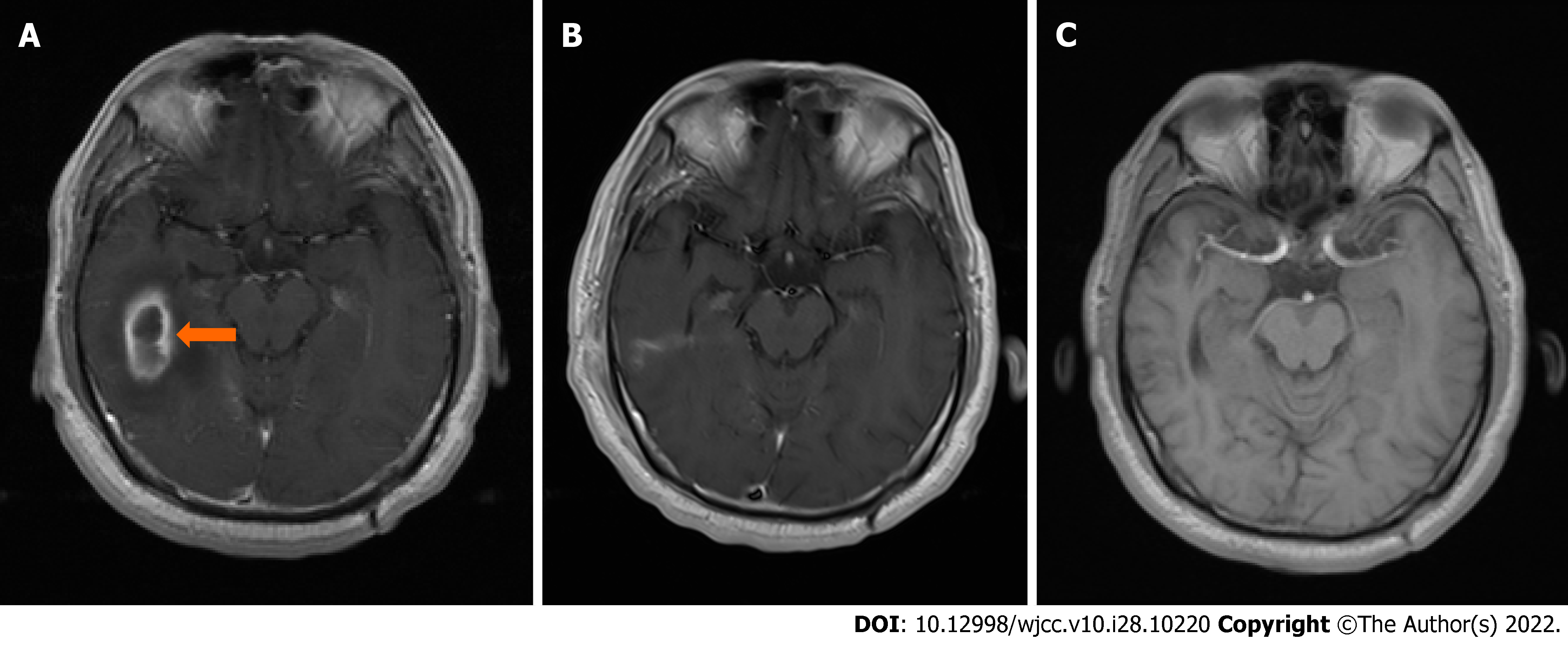
The patient developed right ear otorrhea without hearing loss, tinnitus, vertigo, or headache in 2012. He visited our hospital because of hearing loss in the right ear and headache for 1 mo in 2018. Physical examination showed congestion of the right external auditory canal and a large amount of purulent discharge near the tympanic membrane. Pure tone audiometry showed mixed hearing loss in both ears, and the pure tone averages of air conduction were 70 dB in the right ear and 97 dB in the left ear. Computed tomography (CT) showed an area of low density in the right middle ear and mastoid and auditory ossicle defects. The parietal wall of the right tympanic cavity and the posterior wall of the mastoid sinus were thin and less continuous. There was a small amount of soft tissue flocculent shadow in the left ear tympanum and the mastoid sinus (Figure 1A). Cranial magnetic resonance imaging (MRI) revealed an area of low intensity encapsulated by an area of high intensity in the right temporal lobe (Figure 2A). We diagnosed him with a brain abscess secondary to middle ear cholesteatoma. After consultation with a neurologist, the patient was transferred to the Department of Neurology and received surgery to drain the abscess after one week of systemic antibiotic treatment. The patient received a modified radical mastoidectomy in our department 3 wk later. After 1 mo, an MRI reexamination showed that there was no abscess in the brain (Figure 2B).
The patient’s family history was unremarkable.
Physical examination showed that pus and debris filled the left middle ear cavity. The pure tone averages of air conduction were 55 dB in the right ear and totally deafness in the left ear.
The patient had no meaningful laboratory results throughout the examinations.
CT showed that the area of the soft tissue density in the left middle ear and mastoid was significantly increased compared to the CT in 2018. The posterior wall of the mastoid sinus and auditory ossicles in the left ear wasdestroyed, leaving the left middle ear connecting with the brain (Figure 1B). There was no cholesteatoma in the right ear. An MRI showed no recurrence of brain abscess (Figure 2C).
We diagnosed the patient with left middle ear cholesteatoma.
The patient underwent a modified radical mastoidectomy in the left ear.
A follow-up examination showed that the patient had recovered well.
Otogenic brain abscess is the second most frequent intracranial complication of chronic otitis media[2] and remains a life-threatening complication with an 8%–26.3% mortality rate[3]. The incidence of otogenic brain abscess was once reported to have decreased from 2.3% to approximately 0.1% after the discovery of antibiotics and the development of diagnostic methods[4,5]. However, the incidence has been on the rise[6] in developing countries since 2006, probably due to the resistance caused by the extensive use of antibiotics. We summarized previous studies about otogenic brain abscesses (Table 1) [1,7-18], which showed that males were more commonly affected than females. The cerebellum and temporal lobe were the most frequently affected. In our study, the patient was male and the abscess was in the temporal lobe, which is consistent with previous studies. A bacterial infection usually spreads to the brain via the temporal bone and the dura, as cholesteatomas are known to destroy the bone. For this patient, the infection was suspected to spread via the mastoid to the brain as the temporal bone was destroyed. For treatment, the general agreement is that surgical removal of the brain abscess with systemic antibiotic administration is the preferred treatment, although some studies have shown that nonsurgical conservative treatment is effective for specific types of brain abscesses[12,19-20]. However, the appropriate treatment remains controversial regarding whether, when, and what type of surgery is needed in individual patients[14], as cases of a brain abscess caused by middle ear cholesteatoma are sporadic. The treatment strategy is usually based on the particular institution’s level of experience. It is generally believed that surgery for the middle ear should be performed as soon as possible[3,21]. Nevertheless, there is an opinion that emergency surgery within 24 h is no longer recommended because of antibiotic use[19,22]. The blood supply to the bone may be affected by mastoid surgery, thus affecting the effect of antibiotics[14,23]. In the past, it was believed that neurosurgery should precede ear surgery, as mastoid surgery alone cannot prevent the development of the abscess[24]. A medical record of all patients treated for otogenic intracranial abscesses between 1970 and 2012 at a tertiary referral center in Finland showed that 69% of neurosurgeries were performed before ear surgery[1]. Currently, some clinicians advocate performing otological surgery and neurosurgery at the same time to prevent reinfection[10,25]. In this case, the patient was treated with antibiotics until he was neurologically stable, followed by neurosurgery for the abscess. Surgery for middle ear cholesteatoma was performed until the abscess almost disappeared.
| Date | Country | Number | Children/Adult | M/F | L/R/Both | Localization | Treatment | Ref. |
| 1990-1996 | India | 36 | 21/16 | 26/10 | 19/11/6 | Cerebellum 17 Temporal lobe 9 subdural 10 | Concurrent craniotomy and mastoidectomy | Kurien et al[7] |
| 1968-1999 | Turkey | 41 | 26/15 | 27/14 | 19/22/0 | Cerebellum 17 Temporal lobe 23 both 1 | RM + drainage through the cavity: 28 RM + Burr hole: 7RM + craniotomy: 6 | Sennaroglu et al[8] |
| 1984-2002 | India | 10 | N | N | N | Cerebellum 4 Temporal lobe 6 | RM + drainage through the cavity | Syal et al[9] |
| 1985-2004 | India | 73 | N | 45/28 | N | Cerebellum 5 Temporal lobe 13 Subdural 2 Multiple 1 Perisinus 11 Extradural 29 | RM + drainage through the cavity | Morwani et al[10] |
| 2000-2008 | United States | 30 | 30/0 | 18/12 | 14/16 | Cerebellum 2 Temporal lobe 5 epidural 16 Petrous apicitis 3 | Craniotomy with mastoid 6 Craniotomy without mastoid 3 Mastoidectomy with PE tube 21 PE tube 2 Antibiotics alone 2 | Isaacson et al[12] |
| 2003-2009 | UK | 6 | 5/1 | 3/3 | 3/3 | Subdural 4 Cerebellum 2 | mastoidectomy with needle drainage 5 With burr hole 1 | Alaani et al[11] |
| 1999-2010 | Danmark | 7 | 2/5 | 6/1 | N | Temporal lobe 6 Cerebellum 1 | Craniotomy 1;Aspiration, Mastoidectomy 3 Aspiration & Mastoidectomy 1 | Lildal et al[13] |
| 2009-2014 | India | 22 | 9/131 | 17/5 | N | Temporal lobe 7; Cerebellum 15 | Single-stage transmastoid drainage along with meticulous mastoid clearance | Mukherjee et al[14] |
| 1970-2012 | Finland | 18 | 2/16 | 16/2 | N | Temporal lobe 14 Cerebellum 2 Other 2 | Punction 14; craniotomy 3; ventriculostomy 1; radical mastoid 14; mastoid revision 1 | Laulajainen Hongisto et al[1] |
| 2004-20212 | Italy, Japan, United States, Indonesia | 5 | 1/4 | 4/1 | 2/3 | Temporal lobe 3 Cerebellum 1 Other 1 | Craniotomy+RM 2Drain abscess+RM 1Drain abscess +Canal down procedure 2 | Darmawan et al[18], Majmundar et al[17], Watanabe et al[16], Paolini et al[15] |
There are limited studies of the contralateral ear in patients with cholesteatoma. In patients with cholesteatoma in the middle ear, 46%-65% of the contralateral ears had abnormalities, such as tympanic membrane retraction and cholesteatoma, cholesteatoma was identified in 7%-16.9% of patients[26-29]. The study of da Costa et al[27] suggested that the contralateral ear is cruising in the same direction only one or two steps behind the most affected ear. Studies showed that the degree of temporal bone pneumatization, eustachian tube function, and development of the anterior epitympanic space are significantly decreased in the contralateral ears of patients with unilateral cholesteatoma[30]. These studies indicated that there is a high chance of developing a brain abscess secondary to contralateral ear cholesteatoma if there has been a brain abscess secondary to cholesteatoma in the most affected ear. Gupta et al[31] reported a case of a patient with a bilateral otogenic brain abscess. In this case, the patient had cholesteatoma in the bilateral ears at the initial cholesteatoma diagnosis. The cholesteatoma in the patient’s left ear was very mild 3 years ago. However, cholesteatoma of the left ear developed rapidly. The patient’s CT showed that the posterior wall of the mastoid sinus was destroyed and the cholesteatoma attached to the skull 3 years later. An otogenic abscess is likely to recur if not treated in time.
We experienced a case of cholesteatoma in the contralateral middle ear 3 years after an otogenic abscess caused by middle ear cholesteatoma was cured. The cholesteatoma proliferated quickly in 3 years, destroyed the temporal bones, and was likely to form an intracranial abscess again if the patient was not treated in time. The detailed examination and regular follow-up of the contralateral ear to detect early abnormalities and initiate timely treatment are vital for the prevention of otogenic complications in patients with otogenic abscesses secondary to middle ear cholesteatoma of one ear.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Otorhinolaryngology
Country/Territory of origin: Chile
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Alsawy MF, Egypt; Yang XY, China S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Laulajainen Hongisto A, Aarnisalo AA, Lempinen L, Saat R, Markkola A, Leskinen K, Blomstedt G, Jero J. Otogenic Intracranial Abscesses, Our Experience Over the Last Four Decades. J Int Adv Otol. 2017;13:40-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Osma U, Cureoglu S, Hosoglu S. The complications of chronic otitis media: report of 93 cases. J Laryngol Otol. 2000;114:97-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 125] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Sun J, Sun J. Intracranial complications of chronic otitis media. Eur Arch Otorhinolaryngol. 2014;271:2923-2926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Delbrouck C, Mansbach AL, Blondiau P. Otogenic thrombosis of the lateral sinus: report of a case in a child. Acta Otorhinolaryngol Belg. 1996;50:221-226. [PubMed] |
| 5. | Go C, Bernstein JM, de Jong AL, Sulek M, Friedman EM. Intracranial complications of acute mastoiditis. Int J Pediatr Otorhinolaryngol. 2000;52:143-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 92] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Yorgancılar E, Yildirim M, Gun R, Bakir S, Tekin R, Gocmez C, Meric F, Topcu I. Complications of chronic suppurative otitis media: a retrospective review. Eur Arch Otorhinolaryngol. 2013;270:69-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 83] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 7. | Kurien M, Job A, Mathew J, Chandy M. Otogenic intracranial abscess: concurrent craniotomy and mastoidectomy--changing trends in a developing country. Arch Otolaryngol Head Neck Surg. 1998;124:1353-1356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 49] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Sennaroglu L, Sozeri B. Otogenic brain abscess: review of 41 cases. Otolaryngol Head Neck Surg. 2000;123:751-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Syal R, Singh H, Duggal KK. Otogenic brain abscess: management by otologist. J Laryngol Otol. 2006;120:837-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Morwani KP, Jayashankar N. Single stage, transmastoid approach for otogenic intracranial abscess. J Laryngol Otol. 2009;123:1216-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Alaani A, Coulson C, McDermott AL, Irving RM. Transtemporal approach to otogenic brain abscesses. Acta Otolaryngol. 2010;130:1214-1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Isaacson B, Mirabal C, Kutz JW Jr, Lee KH, Roland PS. Pediatric otogenic intracranial abscesses. Otolaryngol Head Neck Surg. 2010;142:434-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Lildal TK, Korsholm J, Ovesen T. Diagnostic challenges in otogenic brain abscesses. Dan Med J. 2014;61:A4849. [PubMed] |
| 14. | Mukherjee D, Das C, Paul D. Single-Stage Trans-mastoid Drainage of Otogenic Brain Abscess: A Single-Institution Experience. Indian J Otolaryngol Head Neck Surg. 2016;68:179-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Paolini S, Ralli G, Ciappetta P, Raco A. Gas-containing otogenic brain abscess. Surg Neurol. 2002;58:271-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Watanabe K, Hatano GY, Fukada N, Kawasaki T, Aoki H, Yagi T. Brain abscess secondary to the middle ear cholesteatoma: a report of two cases. Auris Nasus Larynx. 2004;31:433-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Majmundar K, Shaw T, Sismanis A. Traumatic cholesteatoma presenting as a brain abscess: a case report. Otol Neurotol. 2005;26:65-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Darmawan AB, Azkia ES. Right hemiparesis caused by massive otogenic brain abscess in children: Unusual case report and review of the literature. Int J Surg Case Rep. 2021;83:105987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Wanna GB, Dharamsi LM, Moss JR, Bennett ML, Thompson RC, Haynes DS. Contemporary management of intracranial complications of otitis media. Otol Neurotol. 2010;31:111-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Tandon S, Beasley N, Swift AC. Changing trends in intracranial abscesses secondary to ear and sinus disease. J Laryngol Otol. 2009;123:283-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Yang H, Chen XW, Gao ZQ, Ni DF, Jiang H, Xu CX, Liu ZY, Zhou BT, Yang DH. [Clinical analysis of otogenic intracranial complications]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2008;43:801-805. [PubMed] |
| 22. | Prasad SC, Shin SH, Russo A, Di Trapani G, Sanna M. Current trends in the management of the complications of chronic otitis media with cholesteatoma. Curr Opin Otolaryngol Head Neck Surg. 2013;21:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 23. | Sharma N, Jaiswal AA, Banerjee PK, Garg AK. Complications of Chronic Suppurative Otitis Media and Their Management: A Single Institution 12 Years Experience. Indian J Otolaryngol Head Neck Surg. 2015;67:353-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 24. | Szyfter W, Kruk-Zagajewska A, Borucki L, Bartochowska A. Evolution in management of otogenic brain abscess. Otol Neurotol. 2012;33:393-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Hafidh MA, Keogh I, Walsh RM, Walsh M, Rawluk D. Otogenic intracranial complications. a 7-year retrospective review. Am J Otolaryngol. 2006;27:390-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 26. | Chalton RA, Stearns MP. The incidence of bilateral chronic otitis media. J Laryngol Otol. 1984;98:337-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | da Costa SS, Teixeira AR, Rosito LP. The contralateral ear in cholesteatoma. Eur Arch Otorhinolaryngol. 2016;273:1717-1721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Kurzyna A, Trzpis K, Hassmann-Poznańska E. [The status of contralateral ear in children with cholesteatoma]. Otolaryngol Pol. 2010;64:152-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Hassman-Poznańska E, Kurzyna A, Trzpis K, Poznańska M. The status of the contralateral ear in children with acquired cholesteatoma. Acta Otolaryngol. 2012;132:404-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Chung JH, Lee SH, Min HJ, Park CW, Jeong JH, Kim KR. The clinical and radiological status of contralateral ears in unilateral cholesteatoma patients. Surg Radiol Anat. 2014;36:439-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Gupta AK, Nagarkar NM, Mann SB, Gupta SK. Bilateral otogenic temporal lobe and post-aural abscesses. J Laryngol Otol. 1997;111:284-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |