Published online Oct 6, 2022. doi: 10.12998/wjcc.v10.i28.10208
Peer-review started: April 22, 2022
First decision: May 30, 2022
Revised: June 11, 2022
Accepted: August 24, 2022
Article in press: August 24, 2022
Published online: October 6, 2022
Processing time: 158 Days and 0.9 Hours
The incidence of cardiac lymphoma is low, and it mainly occurs secondary to non-Hodgkin’s lymphoma, particularly diffuse large B-cell lymphoma. Here, we report a case of follicular lymphoma with cardiac involvement and severe heart failure as the sole clinical manifestation.
A 90-year-old male patient was first admitted to our hospital due to an accidentally discovered painless mass in the right lower abdomen. A biopsy of the mass revealed a follicular lymphoma. Positron emission tomography-computed tomography confirmed mild pericardial effusion, and echocardiography showed no structural abnormalities with normal ejection fraction at the time of diagnosis. The patient refused our recommendation of chemotherapy and was re-admitted 4 mo later due to heart failure. A series of subsequent echocardiographic examinations showed thickening of the left ventricular walls and increasing pericardial effusion over the following 2 mo. His heart failure exacerbated despite all symptomatic and supportive treatments. He passed away after an episode of aspiration pneumonia.
The diagnosis of cardiac lymphoma is difficult as its clinical manifestations are nonspecific, and prognosis is poor.
Core Tip: Most grade 1, 2, and 3A follicular lymphomas are indolent and treatment should be based on the patient’s basic condition. Here, we report a 90-year-old patient with follicular lymphoma, whose sole symptom was cardiac dysfunction that exacerbated rapidly into refractory stage IV cardiac failure. He responded poorly to all supportive and systematic treatments. Early detection of cardiac involvement in follicular lymphoma and timely intervention might be important in improving its prognosis.
- Citation: Sun YX, Wang J, Zhu JH, Yuan W, Wu L. Follicular lymphoma with cardiac involvement in a 90-year-old patient: A case report. World J Clin Cases 2022; 10(28): 10208-10213
- URL: https://www.wjgnet.com/2307-8960/full/v10/i28/10208.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i28.10208
The incidence of both primary and secondary cardiac malignant tumors is low compared to tumors of other organs. Less than 2% of primary cardiac tumors are cardiac lymphoma[1]. However, secondary involvement of the myocardium in patients with systemic lymphoma at autopsy is higher and varies from 8.7% to 20%[2,3]. Differential diagnosis between primary and secondary lymphoma is simple, and when confirming the diagnosis of cardiac lymphoma by pathological examination of the heart lesion, other sites of involvement must be excluded by whole body imaging examination including computed tomography (CT), magnetic resonance imaging (MRI) or positron emission tomography (PET)-CT. However, early diagnosis of cardiac lymphoma is difficult due to its nonspecific clinical manifestations.
All pathologic categories of lymphoma may invade the heart, of which disseminated large B-cell lymphoma may be the most common type[4]. Follicular lymphoma (FL) accounts for about 30% in the United States and 10% in Asia of all adult lymphomas. However, only 4.8% of patients with newly diagnosed FL are older than 85 years, suggesting a significantly lower incidence in patients over the age of 85 than in the general population[5]. Most grade 1, 2, and 3A FLs are indolent. Cardiac involvement as the main clinical manifestation is rare[6].
Here, we report a rare case of FL with heart involvement in a 90-year-old patient, whose main clinical manifestation was heart failure.
A 90-year-old man was admitted to our hospital due to an accidentally discovered painless mass in the right lower abdomen 2 wk before admission.
The painless mass in the right lower abdomen had been identified 2 wk previously. The mass showed no redness and ulceration and could not be returned to the abdominal cavity. No signs of abdominal pain or abnormal defecation, and no symptoms such as fever, marasmus, or night sweat were reported. B-ultrasound examination showed a hypoechoic mass with irregular morphology. The boundary between the mass and iliac vessels was unclear.
The patient had a history of atrial fibrillation for more than 30 years and a pacemaker was implanted 28 years prior. His current medication included digoxin and metoprolol, which helped to maintain his heart rate at 60-80 beats per min, and general low-intensity physical activity did not cause excessive fatigue or asthma. He had hypertension for more than 30 years, and his blood pressure was well controlled on amlodipine, irbesartan and hydrochlorothiazide, ranging from 140-150 to 60-70 mmHg. He also had diabetes for more than 20 years; however, his blood glucose levels were only mildly elevated. He did not adhere to his hypoglycemic therapy, and stopped taking medicine whenever self-monitored glucose levels were within normal ranges.
The patient did not have a history of alcohol consumption or smoking. He had no family history of hereditary disease.
During physical examination, a mass (approximately 50 mm × 30 mm) located in the middle of the right inguinal area was found. The mass was fixed with a hard texture.
Laboratory studies showed that the red blood cell count was 3.3 × 1012/L, hemoglobin was 117 g/L, and blood platelet count was 93 × 109/L. White blood cells and the neutrophil ratio were within the normal range. Erythrocyte sedimentation rate was 4 mm/h. Myocardial markers showed cardiac troponin T (cTnT) of 0.05 ng/mL and plasma N terminal pro-B type brain natriuretic peptide (NT-Pro BNP) of 672.8 pg/mL. Serum tumor markers showed that cytokeratin 19 fragment (Cyfra21-1) was 6.4 ng/mL, and the others were all within the normal range.
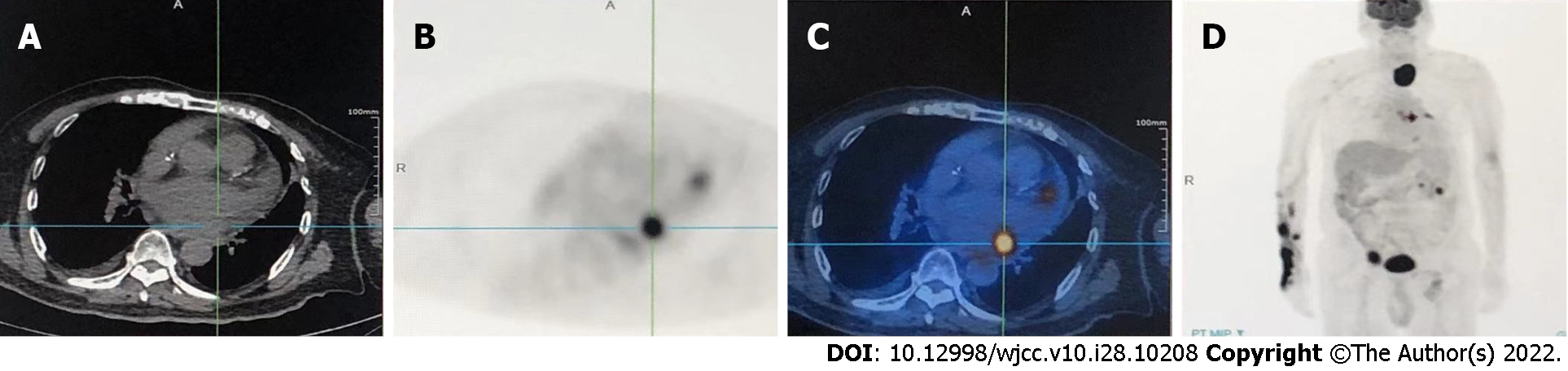
CT showed a soft tissue mass near the right inguinal region closely connected to the right external iliac artery. Multiple small lymph nodes were observed in the abdominal cavity, posterior peritoneum, and right inguinal area. A mild pericardial effusion (10 mm behind the left ventricular posterior wall) was seen on echocardiography. There was no obvious change in cardiac structure and ejection fraction at that time. On PET-CT, enlarged lymph nodes were found in the left abdominal cavity, right-iliac fossa (56.2 mm × 31.1 mm), and in the left lobar thyroid (55.6 mm × 46.3 mm). In addition, involvement of the pericardium could not be excluded (Figure 1).
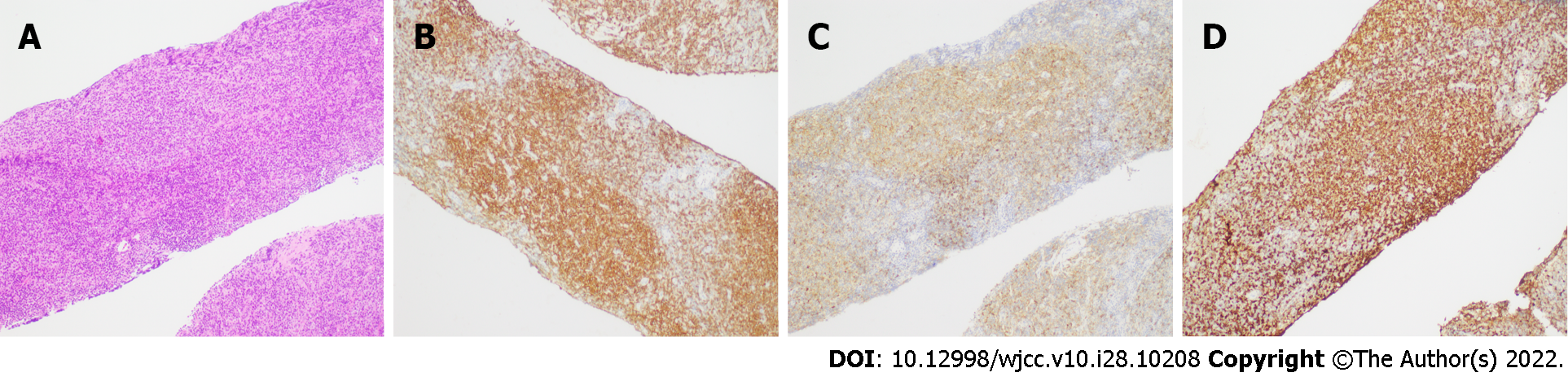
An ultrasound-guided fine needle biopsy of the painless mass was postponed for approximately 10 wk after his first admission as the patient and his family members worried about possible suffering following the procedure. On histological examination, the biopsy specimen contained massive proliferation of lymphoid tissue. Proliferation of B lymphocytes was obvious in this area. Lymphatic follicular structure was revealed in some parts of the biopsy specimen (Figure 2). Immunohistochemical test results showed B-cell lymphoma (Bcl-2)(+), Bcl-6(+), cluster of differentiation 10 (CD10)(+), CD20(+), CD21(+), CD3(+), CD5(+), CD56(-), CD79α(+), c-Myc(-), cyclin-D1(-), Ki-67(30%positive), multiple myeloma oncogene-1(50%+), CD15(-), CD30(scattered+), and anaplastic lymphoma kinase(-). His cTnT was 0.06 ng/mL and NT-Pro BNP was 2922 pg/mL.
The patient was diagnosed with FL (grade I-II, stage IV, group A) 14 wk after discovery of the painless mass.
Taking into account his advanced age, concomitant diseases as well as the risk of tracheal compression due to thyroid gland involvement, we recommended treatment with rituximab alone. However, the patient refused treatment.
Five weeks after the diagnosis of FL, the patient was re-admitted to our hospital due to oliguria (< 500 mL/d), chest distress, paroxysmal nocturnal dyspnea, and pitting edema over both legs. He complained of being unable to lie on his back for 2 d before entering the hospital. Laboratory tests showed that cTnT was 0.149 ng/mL and NT-Pro BNP was 20071 pg/mL. Echocardiography revealed a moderate amount of pericardial effusion (18 mm behind the left ventricle and 9 mm in front of the right ventricle) (Table 1). B-ultrasound examination showed right-sided pleural effusion. As the patient had severe heart failure [New York Heart Association (NYHA) grade IV], rituximab was considered inappropriate at that time and treatment was mainly aimed at improving his cardiac function. Apart from routine therapeutic measures such as controlling respiratory infection, managing diuresis, reducing his heart rate, dilating peripheral vessels, and improving myocardial remodeling, an intrathoracic drain was inserted, and the patient’s clinical symptoms were alleviated for only a short period of time. However, echocardiography showed that the pericardial effusion had rapidly increased. The thickness of the inter-ventricular septum and the left ventricular posterior wall were also increased (Table 1). In addition, serum cTnT and NT pro-BNP levels increased continuously, indicating exacerbation of heart failure. Five weeks after his second admission to hospital, monitoring of vital signs showed a sudden drop in arterial oxygen saturation to 50%-70%. Instant bedside sputum suction, chest X-ray and laboratory tests confirmed aspiration pneumonia. His serum cTnT concentrations increased progressively, with no changes in his electrocardiography; however, echocardiography revealed reduced mobility of the left atrium and ventricle (as shown in the Video 1 and 2), indicating lymphoma involvement of myocardial cells. The patient passed away 28 wk after the mass was found in the right lower abdomen.
| Days after first admission | ||||
| 85 | 121 | 133 | 142 | |
| Interventricular septum thickness in mm | 11 | 11 | 12 | 13 |
| Left ventricular posterior wall thickness in mm | 10 | 11 | 12 | 12 |
| Amount of pericardial effusion | Mild | Mild | Moderate | Massive |
As reviewed by Mendelson et al[7], cardiac lymphoma accounts for 1.3% of primary cardiac tumors and 0.5% of extranodal lymphomas[7]. Most cardiac lymphomas are of B-cell origin. Delayed diagnosis due to atypical symptoms, rapid evolution of the disease, and advanced stage of organ infiltration may be the reasons for its poor prognosis[8].
Symptoms of cardiac lymphoma are nonspecific and dependent on many factors such as tumor location, tumor size, and speed of tumor growth[9]. The most common clinical signs are dyspnea and chest pain. The patient in this case was short of breath when resting and unable to lie flat, which made him rituximab-intolerant. As stage IV cardiac function (NYHA) is one of the stated contradictions in the instructions for rituximab, we were unable to treat the patient on his second admission. He received symptomatic and supportive treatments such as diuresis management, heart rate control, myocardial remodeling improvement, and his heart failure symptoms improved only for a short time. However, as the disease progressed, his cTnT and NT-pro BNP levels increased continuously, and his echocardiography revealed weakened cardiac activity and increased pericardial effusion, indicating exacerbation of his secondary cardiac lymphoma.
Imaging examination is noninvasive and important in detecting cardiac lymphoma at an early stage, even though the final diagnosis is made after histological evaluation. Noninvasive transthoracic echocardiography is commonly used as the first-line assessment in cardiac diseases[4]. The echocardiographic features of secondary cardiac lymphoma often present as a nodular mass infiltrating the myocardium and sometimes with pericardial effusion[10], while primary cardiac lymphoma tends to involve the right side of the heart[1]. However, the accuracy of transthoracic echocardiography is limited by its restricted acoustic window[8]. Transesophageal echocardiography is a more sensitive method for evaluating the tumor[11]. CT and MRI are used to further characterize the tumor due to their marked improvement in tissue and contrast resolution[4]. PET-CT is a useful imaging modality for accurate staging of lymphoma and monitoring treatment response[12]. As our patient was too weak to complete cardiac CT or MRI examination (usually requiring the patient to maintain a supine position without movement for at least 15 min), bedside echocardiography was performed repeatedly, and suggested that cardiac involvement developed quickly from the pericardium to the myocardium. Considering his age, poor clinical status and concomitant diseases, myocardial biopsy was not performed. However, based on the findings of the histologic examination of inguinal lymph nodes, PET-CT scanning and transthoracic echocardiography, a diagnosis of secondary follicular cardiac lymphoma was made. The absence of cardiac pathological results constituted a limitation in this case.
A variety of treatments and combination treatments are recommended for cardiac lymphoma, including surgery, chemotherapy, immunotherapy, and radiotherapy[13]. The therapeutic strategy often involves chemotherapy for primary cardiac lymphoma[1]. Rituximab is also introduced as it has the potential to increase the survival rate when it is combined with cyclophosphamide, doxorubicin, vincristine, and prednisone[3]. Our patient was a weak elderly man diagnosed with stage IV lymphoma with two masses larger than 5 cm in size. Considering his advanced age and concomitant diseases, as well as the patient’s worries regarding the side effects of traditional chemotherapeutic drugs (the patient was a retired anesthesiologist), chemotherapy was not an option at the time of diagnosis. In addition, according to the National Comprehensive Cancer Network Guidelines for Patients: Follicular Lymphoma, Grade 1-2, 2019, rituximab alone is recommended for frail adults as the first-line regimen. However, he also decided to delay treatment, assuming that the disease might progress slowly at his age. As his disease quickly progressed over the next few weeks, he was intolerant to rituximab treatment. Eventually, aspiration pneumonia led to his death 14 wk after diagnosis, and only 28 wk after the mass in the right lower abdomen was found. Whether the patient’s prognosis might have been better if he had agreed and adopted timely treatment with rituximab is unknown. Clinicians should be more active in recommending treatment to elderly patients in the future.
Early diagnosis of cardiac lymphoma is of great importance to improve its poor prognosis. Physicians should be alerted to the detection of cardiac involvement in lymphoma patients, even when a patient presents no cardiac-related signs at diagnosis. Medical imaging examinations and timely treatment should be considered in patients with both primary and secondary cardiac lymphoma, even in frail or older patients. We suggest that cardiac lymphoma can develop very rapidly even in elderly patients; thus, aggressive treatment may be necessary in the absence of contraindications.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Demirli Atici S, Turkey; Imai Y, Japan; Tieranu CG, Romania S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Petrich A, Cho SI, Billett H. Primary cardiac lymphoma: an analysis of presentation, treatment, and outcome patterns. Cancer. 2011;117:581-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 225] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 2. | Alimi H, Poorzand H, Jafarian AH. Malignant lymphoma with diffuse cardiac involvement and pulmonary stenosis. J Cardiol Cases. 2021;23:198-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Jeudy J, Kirsch J, Tavora F, Burke AP, Franks TJ, Mohammed TL, Frazier AA, Galvin JR. From the radiologic pathology archives: cardiac lymphoma: radiologic-pathologic correlation. Radiographics. 2012;32:1369-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Jeudy J, Burke AP, Frazier AA. Cardiac Lymphoma. Radiol Clin North Am. 2016;54:689-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 5. | Cartron G, Trotman J. Time for an individualized approach to first-line management of follicular lymphoma. Haematologica. 2022;107:7-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Aledavood SA, Emadi Torghabeh A, Homaee Shandiz F, Memar B. Cardiac Involvement in Non-Hodgkin Lymphoma, an Incidental Large Atrial Mass: A Case Report. Iran J Cancer Prev. 2015;8:e3913. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Mendelson L, Hsu E, Chung H, Hsu A. Primary Cardiac Lymphoma: Importance of Tissue Diagnosis. Case Rep Hematol. 2018;2018:6192452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Gowda RM, Khan IA. Clinical perspectives of primary cardiac lymphoma. Angiology. 2003;54:599-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 100] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 9. | O'Mahony D, Peikarz RL, Bandettini WP, Arai AE, Wilson WH, Bates SE. Cardiac involvement with lymphoma: a review of the literature. Clin Lymphoma Myeloma. 2008;8:249-252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Bull S, Loudon M, Francis JM, Joseph J, Gerry S, Karamitsos TD, Prendergast BD, Banning AP, Neubauer S, Myerson SG. A prospective, double-blind, randomized controlled trial of the angiotensin-converting enzyme inhibitor Ramipril In Aortic Stenosis (RIAS trial). Eur Heart J Cardiovasc Imaging. 2015;16:834-841. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 111] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 11. | Meng Q, Lai H, Lima J, Tong W, Qian Y, Lai S. Echocardiographic and pathologic characteristics of primary cardiac tumors: a study of 149 cases. Int J Cardiol. 2002;84:69-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 209] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 12. | Cheson BD. PET/CT in Lymphoma: Current Overview and Future Directions. Semin Nucl Med. 2018;48:76-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 13. | Ikeda H, Nakamura S, Nishimaki H, Masuda K, Takeo T, Kasai K, Ohashi T, Sakamoto N, Wakida Y, Itoh G. Primary lymphoma of the heart: case report and literature review. Pathol Int. 2004;54:187-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 84] [Article Influence: 4.0] [Reference Citation Analysis (0)] |