Published online Oct 6, 2022. doi: 10.12998/wjcc.v10.i28.10201
Peer-review started: April 11, 2022
First decision: July 11, 2022
Revised: July 20, 2022
Accepted: August 23, 2022
Article in press: August 23, 2022
Published online: October 6, 2022
Processing time: 169 Days and 3.7 Hours
Pipeline dredging agents are new household deep cleaning products used to dredge blockages in kitchen and bathroom pipeline caused by grease, hair, vegetable residue, paper cotton fibre, and other organic substances. Pipeline dredging agents are corrosive chemicals that can cause poisoning through corrosive damage to the digestive tract; however, this has not been reported clinically. Therefore, this report emphasises that oral pipeline dredging agent poisoning can cause corrosive damage to the digestive tract and may have serious health consequences.
A 68-year-old man consumed liquor (200 mL) at approximately 13:00 on April 22, 2021. At approximately 16:00, his family found him unresponsive with blackened lips, blood spots in the corners of the mouth, and blood stains on the ground, as well as an empty bottle of a pipeline dredging agent. One hour later, he was admitted to the emergency department of a local hospital. Considering the empty bottle, he was suspected to have sustained severe corrosive damage to the digestive tract and was transferred to our department at 23:15 on April 22, 2021. He developed dysphagia and intermittent fever and experienced difficulty in opening his mouth throughout his hospital stay. The patient’s condition gradually stabilised. However, he suddenly developed respiratory failure on day 12, and endotracheal intubation and ventilator-assisted ventilation were performed. However, the patient died after 1.5 h despite emergency rescue efforts.
Pipeline dredging agents are highly corrosive and may cause corrosive damage to the digestive tract and asphyxia upon consumption.
Core Tip: A 68-year-old man who excessively consumed a pipeline dredging agent and 200 mL liquor was admitted to our hospital for approximately 10 h. The patient was diagnosed with acute pipeline dredging agent poisoning, acute alcohol poisoning, and corrosive damage to the digestive tract. The patient died despite emergency rescue efforts for respiratory failure.
- Citation: Li YQ, Yu GC, Shi LK, Zhao LW, Wen ZX, Kan BT, Jian XD. Clinical analysis of pipeline dredging agent poisoning: A case report. World J Clin Cases 2022; 10(28): 10201-10207
- URL: https://www.wjgnet.com/2307-8960/full/v10/i28/10201.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i28.10201
Pipeline dredging agents are new household deep cleaning products. They primarily dredge pipeline blockages caused by grease, hair, vegetable residue, paper cotton fibre, and other organic substances from kitchen and bathroom pipes. Corrosive damage to the digestive tract can occur in some patients who consume corrosive pesticides or chemicals orally[1]. Pipeline dredging agents are also known as pipeline dredging particles. They mostly consist of strong alkaline substances that can cause corrosive damage to the digestive tract; however, this has not been reported clinically. This report emphasises that oral pipeline dredging agent poisoning can cause corrosive damage to the digestive tract and may lead to serious health consequences.
A 68-year-old man was admitted for approximately 10 h after consumption of a pipeline dredging agent and 200 mL liquor.
The patient consumed 200 mL liquor at home at approximately 13:00 on April 22, 2021. At approximately 16:00, his family found him unresponsive with blackened lips, blood spots in the corners of the mouth, and blood stains on the ground beside him, along with an empty bottle of ‘pipeline dredging agent’ (50 g). He was admitted to a local emergency department 1 h later, where he was diagnosed with acute pipeline dredging agent poisoning and acute alcohol poisoning. Accordingly, he was administered naloxone and lansoprazole as symptomatic supportive treatment to reverse the effects of alcohol overdose and protect gastric mucosal, respectively. Later, the patient gradually gained con
The patient had a history of coronary heart disease for 8 years and denied any history of hypertension, diabetes, and other diseases.
No specific genetic diseases were reported by the family.
The patient’s vital signs were as follows: Temperature, 36.3°C; heart rate, 97 beats/min; respiratory rate, 18 breaths/min; blood pressure, 118/67 mmHg; and oxygen saturation, 98%. The patient, an elderly man, was moderately nourished and was lying in bed in an active position. He was conscious and cooperative during the examination. His range of mouth opening (approximately 2.5 cm) was slightly limited. Black burn marks were scattered on both sides of the face, particularly in the nasolabial sulcus. Mucous membranes, such as those on the lips and tongue, were black with obvious ulceration and bleeding (Figure 1A). The neck was soft, and no venous engorgement was observed. The patient’s thyroid gland was not palpable, and there was no thrill or bruit. The trachea was centred, and chest and respiratory movements were symmetrical. Cardiopulmonary physical examination yielded negative results, and the abdominal wall was soft with no tenderness. The liver, as well as the spleen, was not palpable under the ribs. Physiological reflection was observed, and no pathological reflection of Babinski's sign was induced.
The results of laboratory tests conducted at our department were as follows: WBC 6.47 × 109/L; neutrophil ratio (NEU%), 91.10%; alanine transaminase, 20 U/L (reference value 21–72 U/L); aspartate transaminase, 70 U/L (reference value 17–59 U/L); creatinine, 57 µmol/L; serum myoglobin, 72.20 ng/mL (reference value 0–70 ng/mL); high-sensitivity cardiac troponin I, 6.61 ng/L (reference value < 17.5 ng/L); N-terminal brain natriuretic peptide, 162.40 pg/mL; and lactic acid (Lac), 4.40 mmol/L.
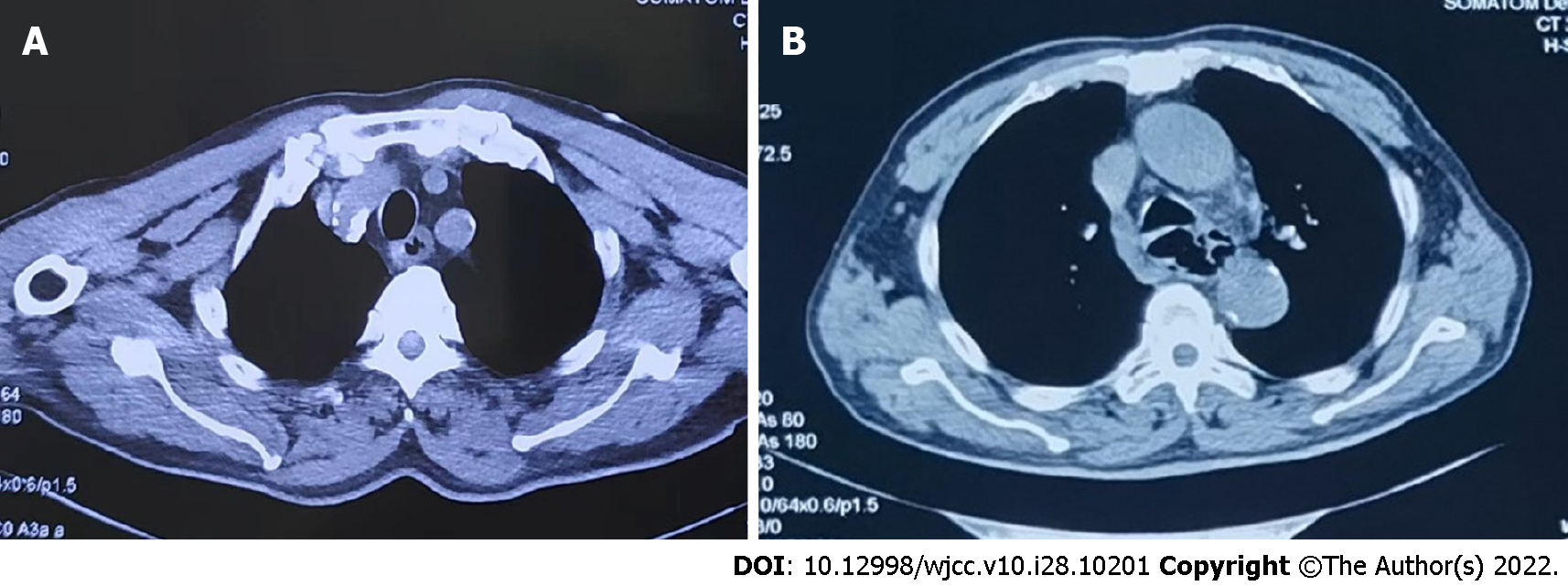
Chest computed tomography (CT) (Figure 2A) revealed coronary artery calcification, thickened oesophageal wall, and a dilated lumen. No significant changes were observed on ECG.
The patient was diagnosed with acute pipeline dredging agent poisoning, acute alcohol poisoning, and corrosive damage to the digestive tract.
Upon admission, oral kangfuxinye (10 mL, three times a day) (Chinese Medicine Approval: Z43020995, Hunan Kelun Pharmaceutical Co., Ltd. Yueyang, Hunan Province, China) and sucralfate suspensoid gel were administered to protect and repair the damaged oral and digestive mucosa. Betamethasone sodium phosphate injection (10.52 mg, once a day), lansoprazole (30 mg, twice a day), reduced glutathione (2.4 g, once a day), magnesium isoglycyrrhizinate injection (0.1 g, once a day) (Chinese Medicine Approval: H20051942, CTTQ, Lianyungang, Jiangsu Province, China), flucloxacillin (1.0 g, every 6 h), and furosemide (20 mg, twice a day) were intravenously administered. Activated charcoal (30 g) (Chinese Medicine Approval: H13022797, Hebei Changtian Pharmaceutical Group Co., Ltd., Baoding, China) and montmorillonite powder (30 g) (Ipsen [Tianjin] Pharmaceutical Co., Ltd., Tianjin, China) with mannitol (250 mL, ×2) were administered orally. Additionally, continuous veno-venous haemodialysis (CVVHF; Prismaflex ST 100) was performed.
On day 2, the patient experienced burning pain in the pharynx and retrosternally. His vital signs were as follows: temperature, 38.5°C; heart rate, 112 beats/min; respiratory rate, 22 breaths/min; blood pressure, 109/76 mmHg; and oxygen saturation, 99%. ECG showed sinus tachycardia. Oral Xipayiguyinye (10 mL, three times a day) (Chinese Medicine Approval: Z65020012, Xinjiang Qikang Habowei Pharmaceutical Co. LTD, Xinjiang, China) and metronidazole gargle were administered. Compound diclofenac sodium was also administered via intramuscular injection.
On day 3, the patient's oropharyngeal pain had worsened and he developed dysphagia. The laboratory test results were as follows: WBC, 13.00 × 109/L; NEU%, 77.70%; and Lac, 2.80 mmol/L. No obvious abnormalities were observed in the other results. Nutritional support was administered, and other previously administered treatments were continued.
On day 7, the black burn marks on the face had subsided, and the lip and tongue ulcers bleeding showed slight improvement. However, the patient’s range of mouth opening remained limited (Figure 1B). The patient was able to drink small amounts of water, but still had difficulty swallowing and experienced intermittent fever. The laboratory test results were as follows: WBC, 9.88 × 109/L and NEU%, 50.60%. Chest CT revealed thickened, dilated, and irregularly shaped oesophageal wall (Figure 2B); few fibrous foci in both lungs and little inflammation in the upper lobe of the left lung; and calcification of the aorta and coronary artery wall.
On day 9, he had a temperature of 38.9°C. His chest physical examination was normal. Accordingly, betamethasone sodium phosphate treatment was stopped and moxifloxacin was used.
On day 11, the patient’s vital signs were stable, and he was not feverish.
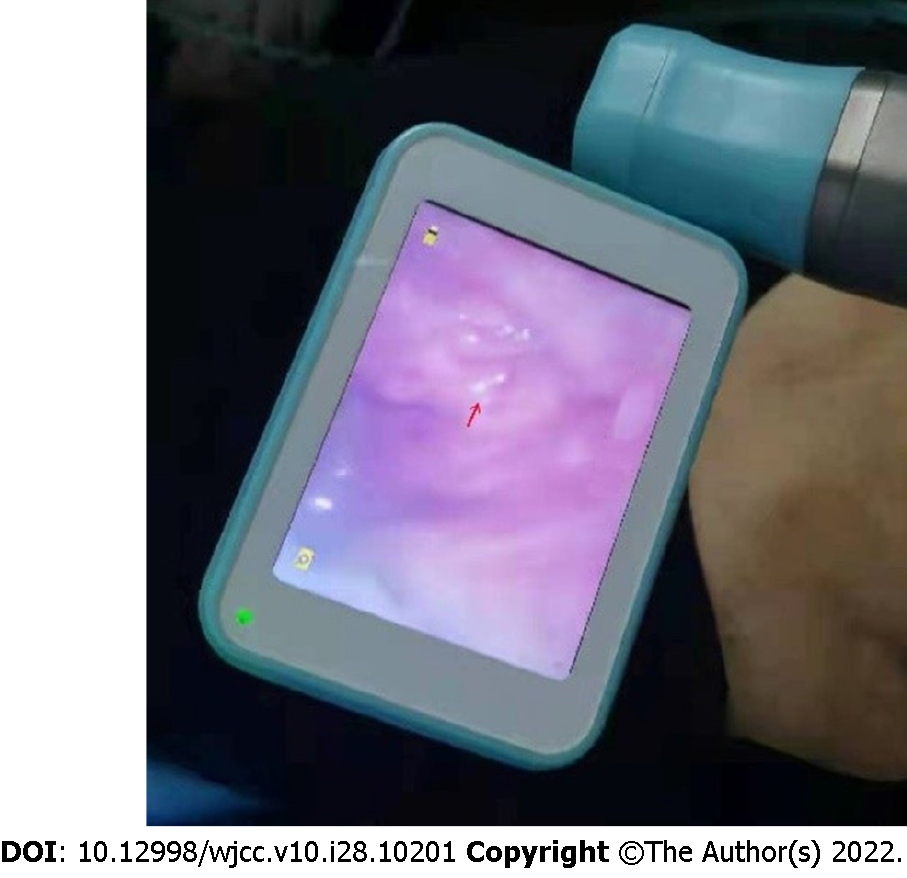
On day 12, the patient suddenly became irritable and developed dyspnoea at 5:48 AM. His vital signs were as follows: body temperature, 36.5°C; heart rate, 140 beats/min; respiratory rate, 46 breaths/min; blood pressure, 78/55 mmHg; and oxygen saturation, 84%. Endotracheal intubation and ventilator-assisted ventilation were performed. During endotracheal intubation, laryngoscopy revealed red granulation tissue following necrotic tissue abscission (Figure 3). The results of laboratory examinations performed after admission are shown in Table 1.
| Inspection item | Normal range | Day 1 | Day 3 | Day 7 |
| WBC (×109/L) | 3.5–9.5 | 6.5 | 11.0 | 9.9 |
| RBC (×1012/L) | 4.3–5.8 | 5.0 | 4.5 | 4.8 |
| Hb (g/L) | 130–175 | 160 | 146 | 154 |
| PLT (×109/L) | 125–350 | 229 | 207 | 339 |
| ALT (IU/L) | 21–72 | 20 | 11 | 33 |
| AST (IU/L) | 17–59 | 70 | 20 | 35 |
| LDH (IU/L) | 313–618 | 710 | 340 | 305 |
| BUN (mmol/L) | 3.2–7.1 | 5.7 | 6.8 | 8.9 |
| Cr (μmol/L) | 58–133 | 57 | 67 | 63 |
| CK (IU/L) | 55–170 | 380 | 276 | 32 |
| CK-MB (ng/mL) | 0.3–4.0 | 19.7 | 12.5 | 0.7 |
| D-Di (µg/mL) | < 0.50 | 4.89 | 0.38 | 1.53 |
The patient died at 7:15 AM despite emergency rescue efforts.
Pipeline dredging agents are available as particles, powders, flakes, liquids, and other forms. Solid pipeline dredging agents are also known as pipeline dredging particles and mostly consist of strong alkaline substances. They are mainly composed of sodium hydroxide, sodium carbonate, sodium hypochlorite, and foaming agents. Generally, acids with a pH of < 2 and bases with a pH of > 12 cause maximum damage[1]. Alkaline substances dissolve tissue proteins and saponify fat, thereby causing liquefactive necrosis. Liquefaction and necrosis produce a gelatinous substance that allows alkaline substances to penetrate further and exacerbate tissue damage[2]. An alkaline liquid also has a strong surface tension and exists in the tissue for a long time[3]. The ingestion of alkaline substances, especially solid alkaline particles, primarily damages the oesophagus[4], but it can also cause corrosive damage to the trachea and bronchi[5]. These particles adhere to the oral mucosa easily and remain in the oropharynx for a long time. Therefore, the lesions are localised predominantly in the larynx, which can easily cause local necrosis and oedema. Patients with oral poisoning reportedly present with a series of clinical manifestations, including nausea, vomiting, oral ulcers, oropharyngeal pain, salivation, abdominal pain, and palpitation[6]. Chest tightness, breathlessness, dyspnoea, dysphagia, hoarseness, hematemesis, peritonitis, and other serious injuries may occur in severe cases[7].
In the present case, the oral pipeline dredging agent was strongly alkaline. The primary clinical manifestations include oral ulcers, oropharyngeal pain, salivation, dyspnoea, dysphagia, and fever. Early application of glucocorticoids can not only effectively reduce the severity of sore throat and dysphagia[8] but also protect the damaged airway of patients[9]. Therefore, we actively administered glucocorticoids; however, they can reduce the body’s immune function, induce infection easily, and aid the spread of potential lesions[10]. Intermittent fever persisted even after anti-infective therapy in the patient. Glucocorticoids were discontinued as the cause of the fever was indeterminate. Upon admission, lansoprazole was administered to inhibit gastric acid secretion, and sucralfate suspensoid gel, kangfuxinye, Xipayiguyine, and metronidazole gargle were administered to protect the gastric mucosa, repair the oral mucosa, and prevent infection. To improve the acid-base balance of water and electrolyte retention, nutritional support therapy was provided. These were also the key factors for early improvement in the patient’s condition. The patient’s condition improved gradually, and his vital signs stabilised. However, the patient suddenly became irritable and developed respiratory failure at 5:48 on day 12. Endotracheal intubation and ventilator-assisted ventilation were performed. At 7:15, the patient died despite emergency rescue efforts. We believe that the primary causes of respiratory failure in the present case are as follows: (1) Solid pipeline dredging agent particles easily adhere to the oropharynx, causing local necrosis and oedema of the larynx. Simultaneously, high alkaline concentrations can easily reduce the slow wave frequency in the digestive tract mucosa, thereby inhibiting peristalsis of the throat, oesophagus, stomach, and intestine, prolonging the contact time with upper digestive tract[11], and further aggravate the local injury and oedema of the throat; (2) on day 12, the scab skin of the patient’s oropharynx and other parts loosened and fell off, resulting in asphyxia due to aspiration; and (3) withdrawal of glucocorticoids may increase airway secretions and aggravate laryngeal oedema. Respiratory failure leads to systemic hypoxia, acidosis, and severe hypoxia of the cardiac muscle cells. In addition, the primary cause of cardiac arrest may have been the fact that the patient had a history of coronary heart disease and developed ischaemia-reperfusion injury after asphyxia.
Based on the analysis and summary of the patient’s clinical data, we believe that the early vital signs were stable and airway assessment appeared safe, even after oral ingestion of non-volatile corrosive substances. The airway should actively be protected, and the vital signs and airway changes should be closely monitored. Our findings might aid clinicians in initiating appropriate interventions for pipeline dredging agent poisoning.
Pipeline dredging agents are highly corrosive. His oral administration may cause not only corrosive damage to the digestive tract but also asphyxia.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Toxicology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghimire R, Nepal; Tajiri K, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Tao X, Yu G, Guo W, Kan B, Song L, Li H, Jian X. Esophagitis dissecans superficialis associated with acute transoral paraquat poisoning: Clinical study of 15 cases. Sci Prog. 2021;104:368504211019647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | De Lusong MAA, Timbol ABG, Tuazon DJS. Management of esophageal caustic injury. World J Gastrointest Pharmacol Ther. 2017;8:90-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (5)] |
| 3. | Vancura EM, Clinton JE, Ruiz E, Krenzelok EP. Toxicity of alkaline solutions. Ann Emerg Med. 1980;9:118-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Hall AH, Jacquemin D, Henny D, Mathieu L, Josset P, Meyer B. Corrosive substances ingestion: a review. Crit Rev Toxicol. 2019;49:637-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol. 2013;19:3918-3930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 273] [Cited by in RCA: 208] [Article Influence: 17.3] [Reference Citation Analysis (7)] |
| 6. | Kluger Y, Ishay OB, Sartelli M, Katz A, Ansaloni L, Gomez CA, Biffl W, Catena F, Fraga GP, Di Saverio S, Goran A, Ghnnam W, Kashuk J, Leppäniemi A, Marwah S, Moore EE, Bala M, Massalou D, Mircea C, Bonavina L. Caustic ingestion management: world society of emergency surgery preliminary survey of expert opinion. World J Emerg Surg. 2015;10:48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Rigo GP, Camellini L, Azzolini F, Guazzetti S, Bedogni G, Merighi A, Bellis L, Scarcelli A, Manenti F. What is the utility of selected clinical and endoscopic parameters in predicting the risk of death after caustic ingestion? Endoscopy. 2002;34:304-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Aertgeerts B, Agoritsas T, Siemieniuk RAC, Burgers J, Bekkering GE, Merglen A, van Driel M, Vermandere M, Bullens D, Okwen PM, Niño R, van den Bruel A, Lytvyn L, Berg-Nelson C, Chua S, Leahy J, Raven J, Weinberg M, Sadeghirad B, Vandvik PO, Brignardello-Petersen R. Corticosteroids for sore throat: a clinical practice guideline. BMJ. 2017;358:j4090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Zhang W, Zhao G, Li L, Zhao P. Prophylactic Administration of Corticosteroids for Preventing Postoperative Complications Related to Tracheal Intubation: A Systematic Review and Meta-Analysis of 18 Randomized Controlled Trials. Clin Drug Investig. 2016;36:255-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Consensus Expert Group on Emergency Use of Glucocorticoids. [Expert consensus on emergency use of glucocorticoids]. Chin J Emerg Med. 2020;29:765-772. |