Published online Oct 6, 2022. doi: 10.12998/wjcc.v10.i28.10172
Peer-review started: March 23, 2022
First decision: May 31, 2022
Revised: June 30, 2022
Accepted: July 27, 2022
Article in press: July 27, 2022
Published online: October 6, 2022
Processing time: 187 Days and 21.3 Hours
The phrase “floating knee is a flail knee joint,” referring to ipsilateral femoral and tibial fractures, was first used by Blake and McBryde in 1975. This condition is often caused by a high-energy trauma with often extensive injury to the soft tissues, and is accompanied by life-threatening systemic complications, including head, chest or abdominal injuries and a high incidence of fat embolism. Floating knee is a severe and uncommon injury pattern.
A 27-year-old man sustained multiple injuries when the electric motorcycle he was riding was hit by a van. His injuries included traumatic hypovolemic shock, comminuted and open type II fractures of the left femoral shaft, fracture of the right femoral shaft, comminuted fracture of the bilateral tibial and fibular shaft, and multiple lacerations and abrasions on his forehead, lower lip, neck and limbs. The diagnosis was simultaneous bilateral floating knee complicated with soft tissue injuries. After emergency treatment and the exclusion of life-threating complications, open reduction and internal fixation were successfully performed using plates and screws in the bilateral femoral and tibial shafts.
Simultaneous bilateral floating knee is a rare and severe injury pattern. The treatment is challenging, and complications. We present a case report of a young adult who suffered from bilateral floating knees during road traffic accident. We also offer our treatment experience of this complex injury and review past literature.
Core tip: Blake and McBryde first used the term floating knee (FK) in 1975. FK often induces severe life-threatening complications, including head injury, intra-abdominal bleeding, vascular rupture, fat embolism syndrome, and acute respiratory distress syndrome. Treatment of FK is challenging. An urgent primary assessment and resuscitation followed by suitable and timely definitive treatment comprising systemic soft tissue and fracture considerations reduces the risk of complications. Simultaneous bilateral FK is extremely rare. We report a case of simultaneous bilateral FK, which included bilateral femoral, tibial, and fibular fractures caused by an electric motorcycle accident, and discuss its therapy process and associated complications.
- Citation: Wu CM, Liao HE, Lan SJ. Simultaneous bilateral floating knee: A case report. World J Clin Cases 2022; 10(28): 10172-10179
- URL: https://www.wjgnet.com/2307-8960/full/v10/i28/10172.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i28.10172
Blake and McBryde used the term floating knee (FK) in 1975, referring to ipsilateral fractures of the femur and tibia that disconnect the knee joint from the rest of the lower limb[1,2]. FK damage is a flail knee joint and includes associated diaphyseal, metaphyseal, and intra-articular fractures[3,4]. The exact incidence of FK remains undetermined[5], but it is likely to be infrequent, with Letts et al[6] reporting an incidence of 2.6% of all fractures in 1986. The incidence of FK, caused by high-velocity and high-energy trauma, is increasing because of changing lifestyles, high-speed motor vehicles, and poor road conditions[7]. FK often induces severe life-threatening complications, such as head injury, intra-abdominal bleeding, vascular rupture, fat embolism syndrome (FES), acute respiratory distress syndrome (ARDS), and soft tissue injury[8-10]. Simultaneous bilateral FK is extremely rare, constituting an unusual fracture pattern. No study has reported the exact incidence. In this study, we report a case of simultaneous bilateral FK, which included bilateral femoral, tibial, and fibular midshaft fractures caused by an electric motorcycle accident. We also offer our treatment experience and discuss its associated complications of this complex injury, based on past literature review.
A 27-year-old man, a laborer from Vietnam, sustained head injury and severe pain as well as swelling and deformity in both lower limbs as a result of a road traffic accident on July 7, 2018.
The patient had no medical history.
The patient had no special past illness.
The patient had no history of drug allergies, smoking, or drinking, and no relevant family history.
The patient was brought by ambulance to our emergency room (ER) for treatment. A general examination revealed that the patient had a head injury with a Glasgow Coma Scale score of E4V5M3 and clear consciousness, and he was able to communicate. The initial vitals revealed hypotension (82/55 mmHg), tachycardia (107 beats/min), and a respiration rate of 26 breaths/min. During the clinical physical examination, the patient was bedridden and was incapable of stepping on or making small motions with either foot. Multiple bleeding lacerations were observed on the left forehead (3.0 × 2.0 cm), lower lip (2.0 × 1.0 cm), anterior neck (4.0 × 1.0 cm), left anterior thigh (2.5 × 2.0 cm), left posterior heel (4.0 × 1.0 cm), and right posterior thigh (3.0 × 1.0 cm). Multiple abrasions were also identified on his face, body and limbs. The thighs and lower limbs appeared deformed, with free floating bone fragments. Distal pulses, including in the bilateral popliteal artery, posterior tibial artery, and pedal dorsal artery, were palpable.
Routine blood tests revealed that hemoglobin was 9.5 mg/dL, and other blood chemistry results, including for liver and kidney function and electrolyte assessment, were all within the normal range.
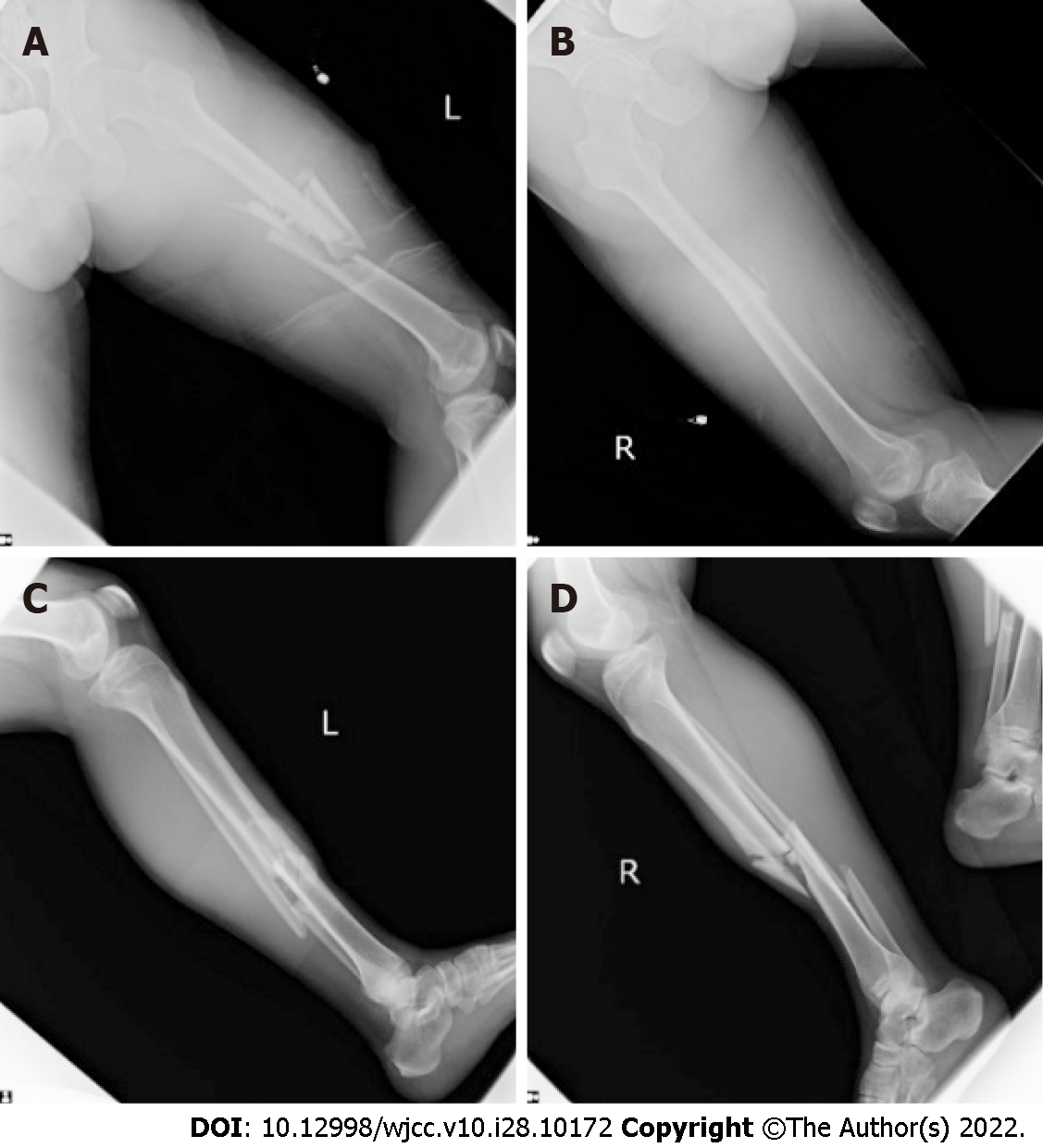
A plain radiograph revealed displaced bilateral femoral, tibial, and fibular midshaft fractures (Figure 1). Computed tomography (CT) identified no notable intracranial, intrathoracic, or intra-abdominal bleeding.
Based on the examination and imaging findings, the main diagnoses were traumatic hypovolemic shock, comminuted and open type II fracture of the left femoral shaft, fracture of the right femoral shaft, comminuted fracture of the bilateral tibial and fibular shaft, and multiple lacerations and abrasions on the forehead, lower lip, neck and limbs.
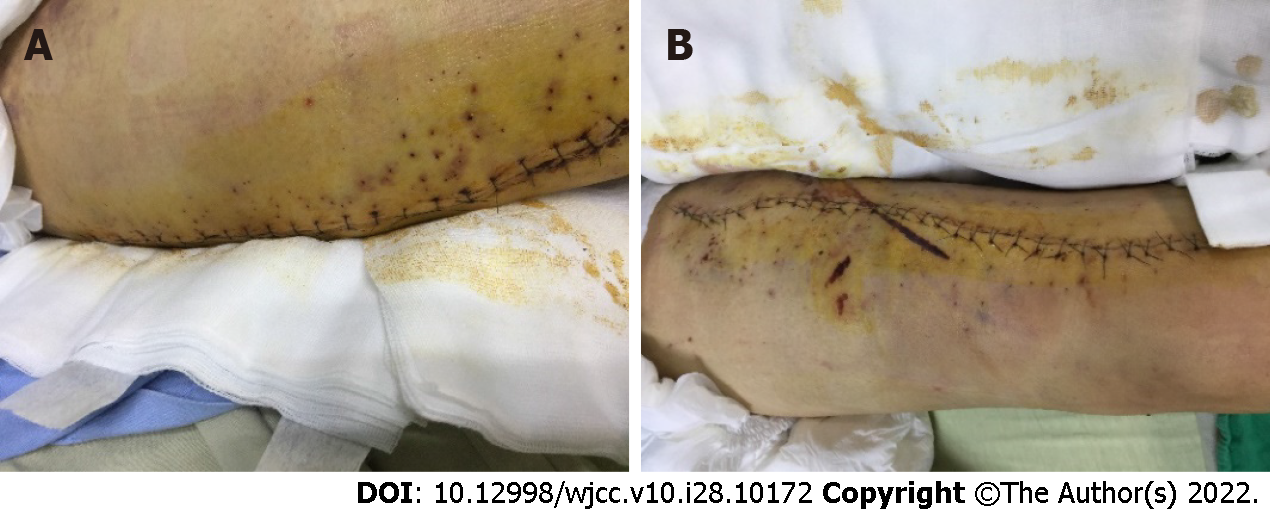
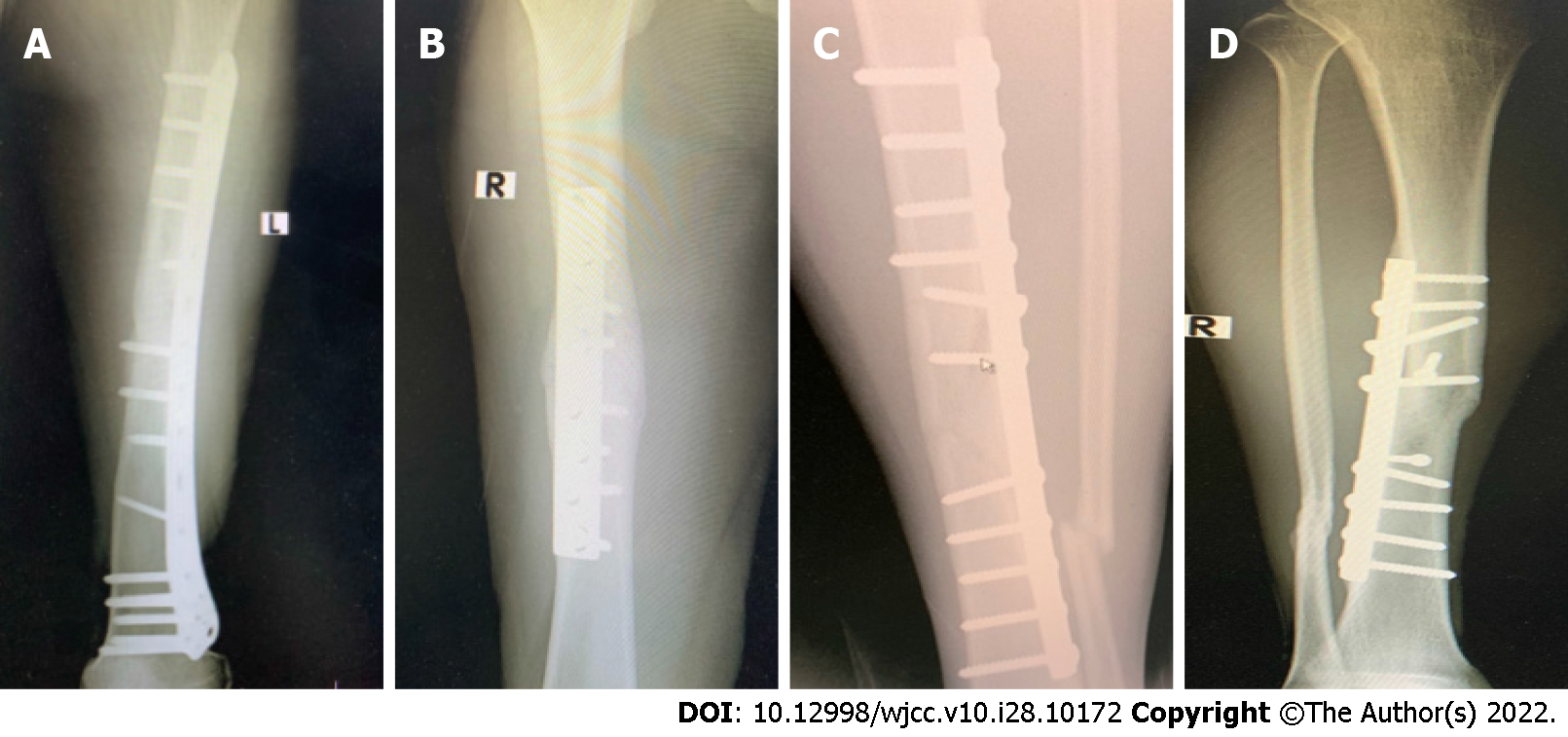
The patient received a blood transfusion of 2 U of packed red blood cells (RBCs) to treat hypovolemic shock. Primary suture of the forehead and lower lip wounds was performed in the ER. Within 4 h of sustaining the injury, after the laboratory data had been received and life-threating complications excluded, the patient was transferred to the operating theater for surgery. The surgical procedure was performed on the left side first because of the greater number of comminuted and open left femoral fractures. The patient received general anesthesia at 08:10 h and was placed on the operating table in the right lateral decubitus position. After sterilization and draping, we performed open reduction and internal fixation (ORIF) with a locking plate in the left femoral shaft. The operating table was then tilted backward approximately 20° to expose the anterior of the leg more fully, and ORIF was performed using a narrow dynamic compression plate (DCP). Two 1/8 Hemovac drains were then inserted into the thighs and calves, and the wound was closed in layers. Finally, with an 18-gauge needle, we punctured hundreds of small holes around the closed wound in the left leg and thigh, imitating a Chinese medicine blood-letting method, to allow the accumulated blood in the tissue to flow out to prevent skin necrosis and compartment syndrome (Figure 2). The same ORIF procedure was performed on the right femoral fracture using a broad DCP and on the tibial fracture using a narrow DCP after changing the patient’s position to left lateral decubitus (Figure 3). The surgical procedure was completed at 02:50 h on the following day. The total operative time was 6 h 40 min. The estimated blood loss was 0.9 L intraoperatively, and the patient received 4 U of packed RBC and 4.2 L of crystalloid solution.
The patient remained intubated following surgery, and his ventilatory and vital signs were closely monitored in the surgical intensive care unit. Initially, antibiotics (1.0 g cefazolin every 6 h and 80 mg gentamycin every 12 h) were administered to prevent wound infection, and nonsteroidal anti-inflammatory drugs were administered for 2 d to relieve pain. The patient’s recovery was positive, and his respiratory condition was smooth. We removed the endotracheal tube after weaning him off the ventilator on July 10, 2018, but a petechial rash on both forearms and progressive shortness of breath with dyspnea and hypoxemia were detected, resulting in emergency endotracheal intubation 9 h later. The patient was sedated using propofol infusion. Simultaneously, we performed further tests, including chest X-ray and blood, arterial blood gas, C-reactive protein (CRP), and D-dimer tests, with the following results: body temperature 38.0°C, white blood cell count 11 320/µL, hemoglobin 8.8 g/dL, CRP 14.15 mg/dL, D-dimer 6915 ng/mL, PO2 37 mmHg, PCO2 43 mmHg, and O2 saturation 73%. These results indicated FES and pneumonia, and we therefore consulted a pulmonologist and cardiologist. The cardiologist administered an anticoagulant (6000 IU clexane every 12 h) to improve FES. An infectious disease specialist was also consulted, who prescribed antibiotics (500 mg vancomycin intravenously every 12 h and 500 mg boojum intravenously every 8 h) to treat pneumonia. The patient’s condition improved gradually, and sedation was withdrawn on July 14, 2018. After several days of treatment, chest X-ray and CT with contrast revealed no abnormal findings. The patient was weaned off the ventilator, and the endotracheal tube was removed successfully on July 16, 2018. He was transferred to the ordinary ward the following day, where he remained until his condition was stable. The patient was discharged on July 23, 2018.
The patient underwent rehabilitation after being discharged. Approximately 4 mo after surgery, he was able to stand and walk without external support. No limited motion or claudication in the bilateral lower limbs was noted. He then returned to Vietnam, returning to work 6 mo after surgery. An X-ray 13 mo postoperatively demonstrated successful fracture union (Figure 4).
When Blake and McBryde first developed the concept of FK in 1975, they classified the injured extremities according to the fracture site: type I fractures involved femoral and tibial shaft fractures, type IIA fractures involved the knee joint, and type IIB fractures involved the hip or ankle joints[1].
In 1978, Fraser et al[11] revised the classification system, in which FK injuries involved the intra-articular knee joint, which affects treatment choices. Type I involves simultaneous femoral and tibial shaft fractures without extension into the knee joint, and type II fractures extend into the knee and are subdivided in the following: type IIA involves a tibial plateau fracture and an ipsilateral femoral shaft fracture; type IIB includes distal femoral fractures extending into the knee joint; and type IIC involves both tibial plateau and distal femoral fractures extending into the knee joint.
An overall incidence of 4.6% and 3.8% has been reported for bilateral femoral and bilateral tibial shaft fractures, respectively[12]. As the number of motor vehicle accidents increases, a progressive increase in the incidence of ipsilateral femur and tibia fractures has been reported. Concomitant fractures of the ipsilateral femur and tibia are serious because of the high mortality associated with these injuries. Although the incidence of FK is undetermined[13], the related mortality rates range from 5% to 15%, and amputations are reported in up to 27% of patients. The incidence of knee ligament injuries related to FK is as high as 53% according to the literature[7,14-16].
Accurate reduction and firm fixation to regain articular and mechanical alignment are the treatment goals to optimize later function[13]. Generally, femoral fractures should be fixed prior to the tibial fracture, except in the case of an open tibial fracture[17]. The choice of implants for fixation includes intramedullary nails, plates, or a combination of the two. Although Rethnam et al[18] reported a short fracture union time and positive functional recovery in patients treated with intramedullary nails for extra-articular fractures and plates for intra-articular fractures in FK, each fracture is unique, and treatment should be decided based on a patient’s individual circumstances, the fracture pattern, and the extent of the soft tissue injury[17]. The patient in this study had simultaneous bilateral FK, a type I fracture as per Blake et al’s and Fraser et al’s classification[1,11]; thus, we decided to use plates and screws for the fixation to reduce the cost of the procedure for the patient, avoid the time involved in changing the patient’s surgical position in the event of pulmonary complications, and avoid any excess radiative exposure for the patient and medical personnel compared with intramedullary nailing.
Although stabilization of femoral or tibial fracture is considered the gold standard during the first 24 h, a staged approach using damage-control orthopedic (DCO) surgery is also recommended according to the patient’s real condition[3]. Patients who sustain major orthopedic trauma, such as FK, must be graded as stable or critical in terms of vital signs, and treatment should follow the evolving DCO approach[3,19]. Life-threatening systemic complications, including head, chest and abdominal injuries with internal bleeding, popliteal artery ruptures, and open fractures, should be treated first, and femoral and tibial fractures should be temporarily immobilized through splinting, skin traction, or external fixation. Immediate definitive internal reduction and fixation are reserved for hemodynamically stable patients[17].
Because FK is a serious long bone fracture accompanied by a combination of other complex bone, ligamentous, and other soft tissue injuries, patients are at high risk of complications[20]. Early complications such as excessive blood loss, superficial and deep wound infection, limb amputation, pneumonia, FES , pulmonary embolism, ARDS and multiple organ failure have been reported. Late complications include joint stiffness, bone malunion, nonunion, chronic osteomyelitis, heterotopic ossification, implant failure, and post-traumatic arthritis[13].
In fat embolism, fat particles enter the circulatory system with vascular occlusion, causing more serious FES. FES is common in patients with long bone fractures. Its incidence is 1%–3% in patients with single long bone fractures and up to 33% in patients with bilateral femoral fractures. The mortality rate is 5%–15%[21,22]. The clinical symptoms of FES usually occur during the first 12–72 h after traumatic injury and include respiratory distress, altered mental status, and skin petechiae[9,23,24]. Pulmonary dysfunction with dyspnea, tachypnea and hypoxemia is the primary symptom, occurring in 75% of cases. Respiratory failure might develop in more than 10% of cases, and 5%–8% of patients might progress to severe ARDS. Approximately 50% of FES patients develop severe hypoxemia and respiratory insufficiency requiring mechanical ventilation[25-27].
The patient in our study had simultaneous bilateral FK with complete femoral, tibial and fibular midshaft fractures in six long bones in both lower limbs; type I fracture in the Blake and McBryde classification. Endotracheal intubation with mechanical ventilation was reapplied because of respiratory insufficiency with dyspnea and hypoxemia 9 h after the initial removal of the endotracheal tube. FES was suspected as the cause. No designated therapy exists for FES; prevention, early diagnosis, and adequate symptomatic treatment are the key responses[26,28]. Rapid supportive treatment of the patient’s respiratory system and additional pharmaceutical treatment provide positive clinical outcomes.
Because this patient experienced severe bilateral FK, the soft tissue of his legs was severely swollen during surgery. To avoid blisters and skin necrosis, we applied a Chinese medicine blood-letting method after the wound was sutured. The skin around the wound was punctured with hundreds of small holes using an 18-gauge needle to allow the accumulated blood in the tissue to flow out, and a drainage tube was inserted to reduce the continued swelling of the soft tissue and prevent compartment syndrome and tissue necrosis[29-31]. After the operation, we administered intravenous antibiotics (1.0 g cefazolin every 8 h for 2 d) and oral antibiotics for the subsequent 3 d. Simultaneously, the wound dressing was changed twice a day for the first 3 d after the operation and then once a day.
The functional outcomes of FK are measured with seven criteria defined by Karlström and Olerud. The Karlström–Olerud criteria include the following: subjective symptoms from thigh or leg; subjective symptoms from knee or ankle joint walking ability return to preinjury work and sports angulation or rotational deformity or both; and shortening and restricted joint mobility of the hip, knee or ankle joint. Scores for each criterion are divided into excellent, good, acceptable and poor[3,32]. Our patient was able to walk independently without external support and was free from bilateral hip, ankle and ankle joints at 4 mo postoperatively. He complained of intermittent mild pain in the left calf, but no pain medication was required. He has returned to most of his preinjury activities, including working 6 mo after surgery. All of his fractures had healed successfully after 13 mo. The patient’s bilateral lower limbs were normal function without shortening, rotation and angulation deformity.
We presented a highly unusual case of a young adult with bilateral FK resulting from a severe road traffic accident. The incidence of unilateral FK is rare, and that of simultaneous bilateral FK even more so. FK is a devastating injury with life-threatening complications, and it often results from high-energy trauma. Patients might present in a critical condition with multiple severe injuries. Treatment of FK is challenging and following with DCO protocol. An urgent primary assessment and resuscitation followed by suitable and timely definitive treatment comprising systemic soft tissue and fracture considerations reduces the risk of complications.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Luo ZW, China; Sangani V, United States S-Editor: Zhang H L-Editor: Kerr C P-Editor: Zhang H
| 1. | Blake R, McBryde A Jr. The floating knee: Ipsilateral fractures of the tibia and femur. South Med J. 1975;68:13-16. [PubMed] |
| 2. | Piétu G, Jacquot F, Féron JM; et les membres du GETRAUM. Le genou flottant: étude rétrospective de 172 cas [The floating knee: a retrospective analysis of 172 cases]. Rev Chir Orthop Reparatrice Appar Mot. 2007;93:627-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Apostolopoulos AP, Angelis S, Elamin SE, Clewer G. Bilateral Floating Knee Injury-Management of a Complex Injury. J Long Term Eff Med Implants. 2019;29:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Lundy DW, Johnson KD. "Floating knee" injuries: ipsilateral fractures of the femur and tibia. J Am Acad Orthop Surg. 2001;9:238-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Bertrand ML, Andrés-Cano P. Management of the Floating Knee in Polytrauma Patients. Open Orthop J. 2015;9:347-355. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Letts M, Vincent N, Gouw G. The "floating knee" in children. J Bone Joint Surg Br. 1986;68:442-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 30] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Veith RG, Winquist RA, Hansen ST Jr. Ipsilateral fractures of the femur and tibia. A report of fifty-seven consecutive cases. J Bone and Joint Surgery. 1984;66:991-1002. [RCA] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 48] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Philip PJ, Georgekutty, Stephen M, Sultan AS. Functional outcome of floating knee injuries after fixation: A follow up study. Int J Orthop Sci. 2020;6:336-339. [DOI] [Full Text] |
| 9. | Ebina M, Inoue A, Atsumi T, Ariyoshi K. Concomitant fat embolism syndrome and pulmonary embolism in a patient with a femoral shaft fracture. Acute Med Surg. 2016;3:135-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Demirtas A, Azboy I, Alemdar C, Gem M, Ozkul E, Bulut M, Uzel K. Functional outcomes and quality of life in adult ipsilateral femur and tibia fractures. J Orthop Translat. 2019;16:53-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Fraser RD, Hunter GA, Waddell JP. Ipsilateral fracture of the femur and tibia. J Bone Joint Surg Br. 1978;60-B:510-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 82] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Kontakis GM, Tossounidis T, Weiss K, Pape HC, Giannoudis PV. Fat embolism: special situations bilateral femoral fractures and pathologic femoral fractures. Injury. 2006;37 Suppl 4:S19-S24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Vallier HA, Manzano GW. Management of the Floating Knee: Ipsilateral Fractures of the Femur and Tibia. J Am Acad Orthop Surg. 2020;28:e47-e54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Mohamadean A, Beeh HA. Floating knee injuries: treatment with a single approach. Egypt Orthop J. 2017;52:6. [DOI] [Full Text] |
| 15. | Oh CW, Oh JK, Min WK, Jeon IH, Kyung HS, Ahn HS, Park BC, Kim PT. Management of ipsilateral femoral and tibial fractures. Int Orthop. 2005;29:245-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Yadav U, Dhupper V, Das J, Lamba A, Gaurav, Behera KC, Devgan A, Kumar N. Bilateral floating knee: a rare case report with review of literature. Int J Res Orthop. 2020;6:851. [DOI] [Full Text] |
| 17. | Muñoz Vives J, Bel JC, Capel Agundez A, Chana Rodríguez F, Palomo Traver J, Schultz-Larsen M, Tosounidis T. The floating knee: a review on ipsilateral femoral and tibial fractures. EFORT Open Rev. 2016;1:375-382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Rethnam U, Yesupalan RS, Nair R. Impact of associated injuries in the floating knee: a retrospective study. BMC Musculoskelet Disord. 2009;10:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Roberts CS, Pape HC, Jones AL, Malkani AL, Rodriguez JL, Giannoudis PV. Damage control orthopaedics: evolving concepts in the treatment of patients who have sustained orthopaedic trauma. Instr Course Lect. 2005;54:447-462. [PubMed] |
| 20. | Chen AT, Vallier HA. Noncontiguous and open fractures of the lower extremity: Epidemiology, complications, and unplanned procedures. Injury. 2016;47:742-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Makarewich CA, Dwyer KW, Cantu RV. Severe neurologic manifestations of fat embolism syndrome in a polytrauma patient. Am J Orthop. 2015;44:E25-8. [PubMed] |
| 22. | Al Shareef K, Asadullah M, Helal M. Fat Embolism Syndrome Due to Fracture Right Femur: A Case Report. Egypt J Hosp Med. 2017;68:923-928. [DOI] [Full Text] |
| 23. | Mellor A, Soni N. Fat embolism. Anaesthesia. 2001;56:145-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 230] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 24. | Gurd AR. Fat embolism: an aid to diagnosis. J Bone Joint Surg Br. 1970;52:732-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 210] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Carlson DS, Pfadt E. Fat embolism syndrome. Nursing. 2011;41:72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Fowler AA, Hamman RF, Good JT, Benson KN, Baird M, Eberle DJ, Petty TL, Hyers TM. Adult respiratory distress syndrome: risk with common predispositions. Ann Intern Med. 1983;98:593-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 558] [Cited by in RCA: 504] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 27. | King MB, Harmon KR. Usuall forms of Pulmonary embolism. Clin chest Med. 1994;15:561-580. [RCA] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 70] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Porpodis K, Karanikas M, Zarogoulidis P, Konoglou M, Domvri K, Mitrakas A, Boglou P, Bakali S, Iordanidis A, Zervas V, Courcoutsakis N, Katsikogiannis N, Zarogoulidis K. Fat embolism due to bilateral femoral fracture: a case report. Int J Gen Med. 2012;5:59-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Chen PD, Chen GZ, Xu YX. Study strategies for bloodletting therapy in treatment of acute soft tissue injuries. Zhong Xi Yi Jie He Xue Bao. 2011;9:237-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Erqing D, Haiying L, Zhankao Z. One hundred and eighty-nine cases of acute articular soft tissue injury treated by blood-letting puncture with plum-blossom needle and cupping. J Tradit Chin Med. 2005;25:104-105. [PubMed] |
| 31. | Zhou W, Niu X, Ma J. [Blood-letting therapy combined with acupuncture for 50 cases of ankle joint sprain]. Zhongguo Zhen Jiu. 2015;35:43. [PubMed] |
| 32. | Karlström G, Olerud S. Ipsilateral fracture of the femur and tibia. J Bone Joint Surg Am. 1977;59:240-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 64] [Article Influence: 1.3] [Reference Citation Analysis (0)] |