Published online Oct 6, 2022. doi: 10.12998/wjcc.v10.i28.10130
Peer-review started: February 24, 2022
First decision: April 19, 2022
Revised: May 9, 2022
Accepted: August 21, 2022
Article in press: August 21, 2022
Published online: October 6, 2022
Processing time: 215 Days and 12.5 Hours
Primary liver cancer is one of the most common malignant tumours, while primary splenic lymphoma is a rare malignancy. Thus, cases of hepatocellular carcinoma (HCC) combined with splenic lymphoma are extremely rare.
We present a 62-year-old woman who was admitted to the Interventional Radiology Department with a lump in the spleen and liver as well as multiple enlarged lymph nodes visible by ultrasound. Contrast-enhanced computed of the abdomen revealed a circular, low-density, shallow mass (approximately 2.6 cm in diameter) in the left intrahepatic lobe and multiple round, low-density shadows in the spleen with clear boundaries (maximum diameter 7.6 cm). Based on the characteristic clinical symptoms and explicit radiological findings, the clinical diagnosis was HCC with metastasis to the liver portal, retroperitoneal lymph nodes, and spleen. After transcatheter arterial chemoembolization and sequential radiofrequency ablation, the -fetoprotein level returned to the normal range, and the hepatitis B cirrhosis improved. In addition, splenic tumour biopsy confirmed the diagnosis of primary malignant lymphoma, which went into remission after chemotherapy.
HCC with primary splenic non-Hodgkin lymphoma is extremely rare and easily misdiagnosed. Better understanding would facilitate early diagnosis, treatment and prognosis.
Core Tip: This case of hepatocellular carcinoma with splenic primary non-Hodgkin lymphoma is extremely rare and easily misdiagnosed. A better understanding of such cases would facilitate early diagnosis, treatment and prognosis.
- Citation: Wu FZ, Chen XX, Chen WY, Wu QH, Mao JT, Zhao ZW. Multiple primary malignancies – hepatocellular carcinoma combined with splenic lymphoma: A case report. World J Clin Cases 2022; 10(28): 10130-10135
- URL: https://www.wjgnet.com/2307-8960/full/v10/i28/10130.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i28.10130
Multiple primary malignancies (MPMs) are defined as more than one synchronous or metachronous cancer in the same individual[1]. If the tumours originate from different sites and/or belong to different histological or morphological groups, they are considered MPMs. The incidence of MPMs in the cancer population varies between 2.4% and 8% but up to 17% within 20 years of follow-up[2].
Primary liver cancer is one of the most common malignant tumours. With improvements in clinical diagnosis and treatment, the diagnosis rate of hepatocellular carcinoma (HCC) complicated with extra
This report describes a rare case of HCC combined with splenic lymphoma.
A 62-year-old female patient with blurred vision in the right eye for > 3 mo was admitted to the Ophthalmology Department in Lishui Hospital of Zhejiang University.
The patient with blurred vision in the right eye for > 3 mo was admitted to the Ophthalmology Department in Lishui Hospital of Zhejiang University.
This patient was a hepatitis B carrier with cirrhosis of the liver for > 2 years. She reported that she had never smoked tobacco or drunk alcohol.
No specific cancer history was recorded on her pedigree.
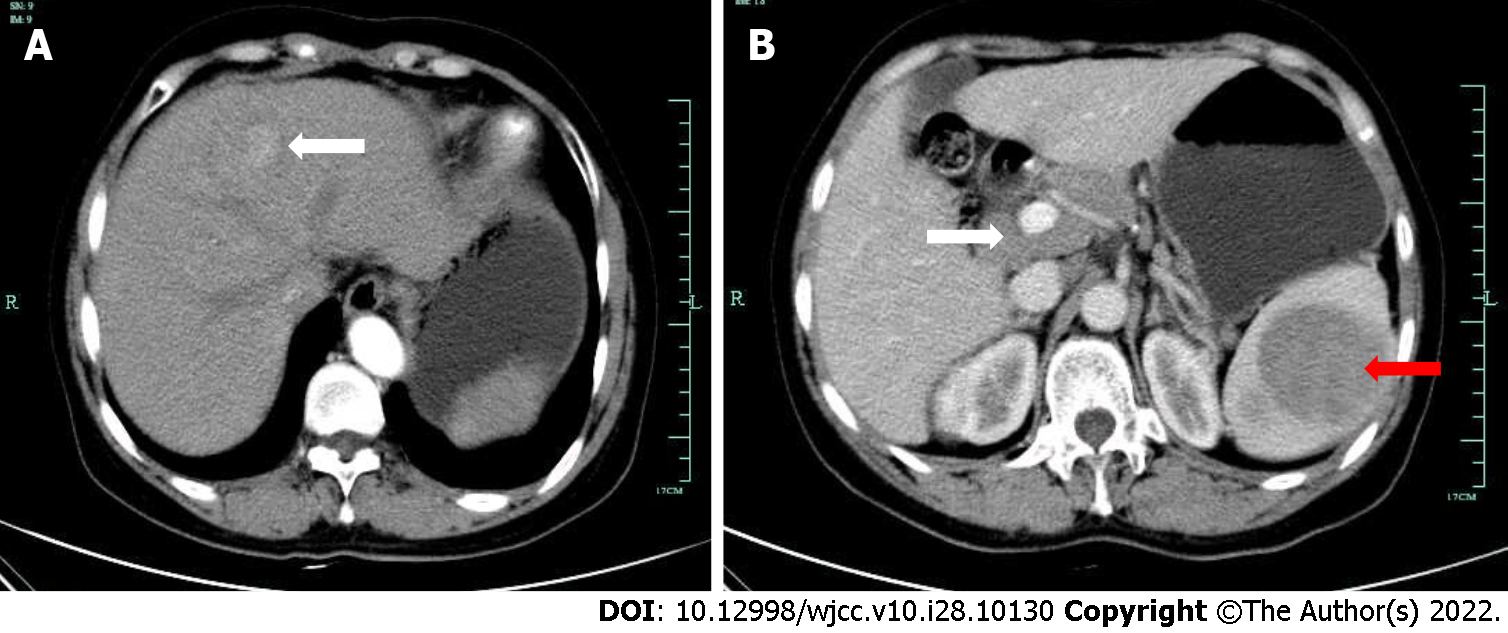
Abdominal ultrasound showed intrahepatic hypoechoic nodules, multiple hypoechoic deposits in the spleen, and multiple enlarged retroperitoneal lymph nodes. The physical examination revealed that she had a palpable tender mass with a smooth surface 4 cm under the left ribcage. Contrast-enhanced computed tomography (CT) of the abdomen revealed a circular low-density shallow mass (approximately 2.6 cm diameter) on the left intrahepatic leaves; arterial phase lesions were significantly enhanced with a relatively low density in the portal phase, which is typical for liver cancer with fast forward and backward characteristics. Multiple circular low-density shadows were detected in the spleen with clear boundaries (maximum diameter 7.6 cm), and the CT value was 34 HU. The enhancement of the lesion was lightly heterogeneous and had a low density compared with the normal spleen parenchyma. Multiple enlarged lymph nodes were detected around the liver portal vein and retroperitoneal space with partial fusion conglobation, which revealed cells suspected for HCC with possible metastasis to the liver portal, retroperitoneal lymph nodes, and spleen.
Hepatitis B virus (HBV) markers were HBsAg+, HBeAb+, HBcAb+, serum -fetoprotein (AFP) 1394.3 ng/mL, and HBV DNA < 500 copies/mL. Immunohistochemical staining of the lesion sample was positive for CD20, PAX5, Bcl-2, Bcl-6 and CD10, and partially positive for Mum-1 and Ki67 (70% cells); CD21 staining for follicular dendritic cell network damage was positive, while CD3 and CD45RO were negative.
Positron emission tomography (PET)/CT disclosed an enlarged spleen with multiple confluent mass lesions. Radiation absorption was unusually high with a maximum standardized uptake value (SUV) of 16.2 in the spleen. Multiple enlarged lymph nodes were observed in the neck, left clavicle, axilla, right hilum, mediastinum, liver hilum and peritoneum, lower abdominal cavity, left pelvic wall, and inguinal region. There was increased radiation uptake in those regions with a maximum SUV of 15.9. In the peritoneum, lymph nodes were partly fused, with unclear boundaries and partial pressure on the surrounding (Figure 1).
Based on these findings, the patient was diagnosed with splenic primary NHL.
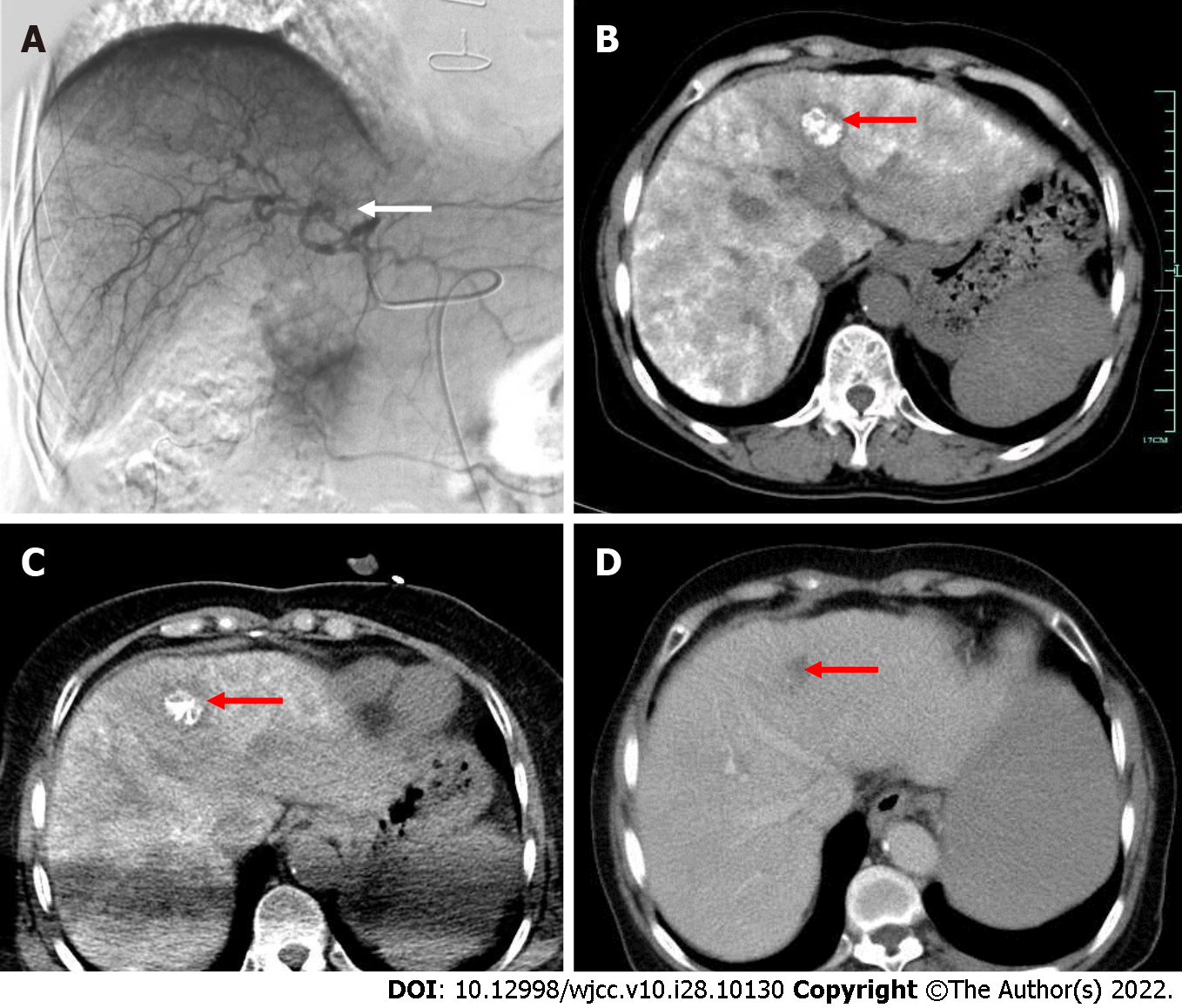
The patient was recommended to be treated with hepatic arteriography and transcatheter arterial chemoembolization (TACE) (Figure 2A). Liver CT showed dense lipiodol deposition in the lesions (Figure 2B). To further consolidate treatment, CT-guided percutaneous radiofrequency ablation was performed on the hepatic lesion (Figure 2C). One month after treatment, the AFP level of the patient had returned to the normal range, and the tumour had regressed completely (Figure 2D).
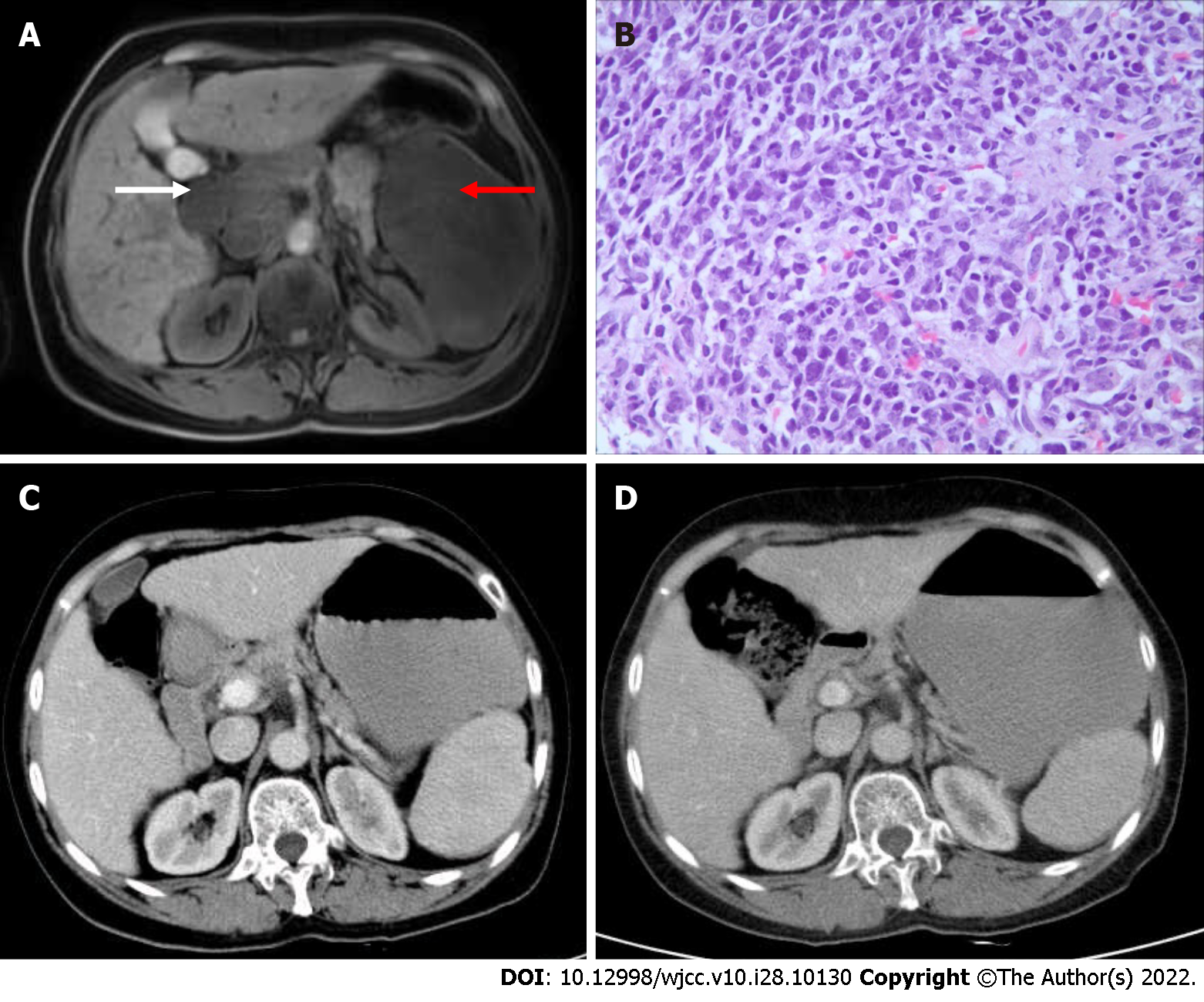
Approximately 3 mo after treatment, magnetic resonance imaging of the upper abdomen showed complete necrosis of the left hepatic lobe lesions, and the hepatic portal vein, spleen and retroperitoneal lymph nodes were significantly enlarged. The largest spleen lesion reached 12.6 cm in diameter (Figure 3A). Further evaluation by splenic biopsy showed a patchy distribution of tumour cells and the disappearance of normal structures, which was considered diffuse large B-cell lymphoma (Figure 3B). Immunohistochemical staining of the lesion sample was positive for CD20, PAX5, Bcl-2, Bcl-6 and CD10 and partially positive for Mum-1 and Ki67 (70% cells). CD21 staining for FDC network damage was positive, while CD3 and CD45RO were negative. PET/CT revealed an enlarged spleen with multiple confluent masses. Radiation absorption was unusually high, with a maximum SUV of 16.2 in the spleen. Multiple enlarged lymph nodes were observed in the neck, left clavicle, axilla, right hilum, mediastinum, liver hilum and peritoneum, lower abdominal cavity, left pelvic wall, and inguinal region. There was increased radiation uptake in those regions, with a maximum SUV of 15.9. In the peritoneum, the lymph nodes were partly fused, with unclear boundaries and partial pressure on the surroundings. Based on these findings, the patient was diagnosed with splenic primary non-Hodgkin's lymphoma.
Next, the patient received R-CHOP combined chemotherapy in June 2015: Rituximab 600 mg, vindesine (VDS) 4 mg and idarubicin needle (IDA) 20 mg on d 1; cyclophosphamide IFO2.0 on d 1-3; prednisone 90 mg on d 1-5. One month after chemotherapy, abdominal enhanced CT showed that the enlarged hilar and retroperitoneal lymph nodes had disappeared, and the spleen lesions were significantly reduced. Due to financial difficulties, the patient declined further use of rituximab and underwent a CHOP regimen (IFO2.0 on d 1-3; VDS 4 mg and liposomal doxorubicin 40 mg on d 1; prednisolone 90 mg on d 1-5) on August 20, September 17, October 17, and November 22, 2015. The splenic lesion was further reduced (Figure 3C), and the patient is now on regular follow-up and in good health (Figure 3D).
One month after chemotherapy, abdominal enhanced CT showed that the enlarged hilar and retroperitoneal lymph nodes had disappeared, and the spleen lesions were significantly reduced.
Multiple primary malignancies (MPMs) are defined as two or more unrelated primary malignant tumours that originate from different organs and occur in the same patient simultaneously or successively. The case reported here had a medical history of chronic hepatitis B and elevated serum AFP. Primary small hepatic carcinoma in the left lobe and primary NHL in the spleen were confirmed by enhanced CT, hepatic artery digital subtraction angiography imaging, and splenic biopsy. According to the latest National Comprehensive Cancer Network Hepatobiliary Cancers Clinical Practice Guidelines[7], these findings meet the diagnostic criteria for MPMN. Cases of primary hepatic tumour combined with splenic lymphoma are rare. Due to the lack of experience, the patient was initially misdiagnosed with primary hepatic carcinoma with metastasis to the hepatic portal, retroperitoneal lymph node, and spleen. Primary liver cancer transfers intrahepatically through the intrahepatic portal vein system, hepatic vein, and hilar lymph nodes. Distant metastasis commonly occurs in the lung and is extremely rare in the spleen. A large number of macrophages and lymphocytes, including cytotoxic T cells with direct killing effects, are present inside the spleen, making it unsuitable for cancer cell growth[8]. After the intrahepatic lesion was cured, the serum AFP gradually returned to normal. However, the spleen, hepatic portal vein, and retroperitoneal lymph nodes were enlarged, inconsistent with the AFP level, ruling out the possibility of liver cancer metastasis. Additionally, splenic lesion biopsy confirmed a diagnosis of NHL.
The majority of primary splenic NHL originates from B cells, characterizing splenomegaly. Compared with other imaging examinations, PET/CT has a high sensitivity for NHL lesions. It can detect not only infringed lymph nodes but also pathological changes outside the junction. Therefore, this technique is important for diagnosis, staging, treatment planning, and efficacy evaluation in malignant lymphoma[9]. Recently, researchers found that the hepatitis B rate is high in NHL patients[10], suggesting a relationship between both pathologies. The onset of most liver cancer cases is caused by hepatitis B cirrhosis in China. The diagnosis of primary liver cancer with lymph node metastasis should be concurrent, and it needs to be differentiated from NHL. Currently, imaging and pathological exa
TACE combined with conventional radiofrequency ablation could achieve a curative effect locally in early small hepatic carcinoma. NHL is a systemic malignant tumour. Appropriate chemotherapy should be prescribed for patients with HBV infection, minimizing liver damage with antiviral drugs. In this case, a good response was achieved after chemotherapy.
Primary hepatic carcinoma combined with primary splenic lymphoma is rare. The understanding of EHPM should be improved to avoid misdiagnosis, and timely splenic biopsy should be performed for the accurate diagnosis of primary splenic lymphoma.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kumar SKY, India; Manrai M, India S-Editor: Yan JP L-Editor: Kerr C P-Editor: Yan JP
| 1. | Shan S, She J, Xue ZQ, Su CX, Ren SX, Wu FY. Clinical characteristics and survival of lung cancer patients associated with multiple primary malignancies. PLoS One. 2017;12:e0185485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Sakellakis M, Peroukides S, Iconomou G, Boumpoucheropoulos S, Kalofonos H. Multiple primary malignancies: a report of two cases. Chin J Cancer Res. 2014;26:215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 3. | Hong S, Jeong SH, Lee SS, Chung JW, Yang SW, Chung SM, Jang ES, Kim JW, Kim JH, Kim H, Cho JY, Yoon YS, Han HS. Prevalence and outcomes of extrahepatic primary malignancy associated with hepatocellular carcinoma in a Korean population. BMC Cancer. 2015;15:146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Kee KM, Wang JH, Wang CC, Cheng YF, Lu SN. Hepatocellular Carcinoma associated with Extra-hepatic Primary Malignancy: its Secular change, Clinical Manifestations and Survival. Sci Rep. 2016;6:30156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Kai K, Miyoshi A, Kitahara K, Masuda M, Takase Y, Miyazaki K, Noshiro H, Tokunaga O. Analysis of Extrahepatic Multiple Primary Malignancies in Patients with Hepatocellular Carcinoma according to Viral Infection Status. Int J Hepatol. 2012;2012:495950. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Abdelwahed Hussein MR. Non-Hodgkin’s lymphoma of the oral cavity and maxillofacial region: a pathologist viewpoint. Expert Rev Hematol. 2018;11:737-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Benson AB, D’Angelica MI, Abbott DE, Anaya DA, Anders R, Are C, Bachini M, Borad M, Brown D, Burgoyne A, Chahal P, Chang DT, Cloyd J, Covey AM, Glazer ES, Goyal L, Hawkins WG, Iyer R, Jacob R, Kelley RK, Kim R, Levine M, Palta M, Park JO, Raman S, Reddy S, Sahai V, Schefter T, Singh G, Stein S, Vauthey JN, Venook AP, Yopp A, McMillian NR, Hochstetler C, Darlow SD. Hepatobiliary Cancers, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2021;19:541-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 575] [Article Influence: 143.8] [Reference Citation Analysis (0)] |
| 8. | Kilani-Jaziri S, Mokdad-Bzeouich I, Krifa M, Nasr N, Ghedira K, Chekir-Ghedira L. Immunomodulatory and cellular anti-oxidant activities of caffeic, ferulic, and p-coumaric phenolic acids: a structure-activity relationship study. Drug Chem Toxicol. 2017;40:416-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 9. | Shaikh F, Chan AC, Awan O, Jerath N, Reddy C, Khan SA, Graham MM. Diagnostic Yield of FDG-PET/CT, MRI, and CSF Cytology in Non-Biopsiable Neurolymphomatosis as a Heralding Sign of Recurrent Non-Hodgkin’s Lymphoma. Cureus. 2015;7:e319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Juárez-Salcedo LM, Sokol L, Chavez JC, Dalia S. Primary Gastric Lymphoma, Epidemiology, Clinical Diagnosis, and Treatment. Cancer Control. 2018;25:1073274818778256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 73] [Article Influence: 10.4] [Reference Citation Analysis (0)] |