Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9478
Peer-review started: April 27, 2022
First decision: May 12, 2022
Revised: May 31, 2022
Accepted: August 5, 2022
Article in press: August 5, 2022
Published online: September 16, 2022
Processing time: 127 Days and 21.4 Hours
Arterial thrombosis is a serious and rare complication of ovarian hyperstimulation syndrome (OHSS). Herein, we describe a case of OHSS complicated by common carotid artery thrombosis and malignant middle cerebral artery infarction after egg retrieval and before embryo transfer.
A 32-year-old female with a family history of thrombosis who was undergoing in vitro fertilization due to unexplained infertility, was admitted due to abdominal distension for 3 d and coma for 2 h. She received egg retrieval 7 d ago and embryo transfer had not yet been performed. Blood biochemical analysis showed estrogen of 15781 pmol/L. Gynecological examination showed palpable masses on both sides of the adnexal areas. Ultrasound observed enlarged ovaries and abdominal ascites. Imaging examination of the head and neck revealed fresh malignant middle cerebral artery infarction in the left side of brain and internal carotid artery as well as occlusion in the left carotid artery, internal carotid artery, and middle cerebral artery. The patient was finally diagnosed with severe OHSS, complicated by common carotid artery thrombosis and malignant middle cerebral artery infarction. Liquid replacement, anticoagulation, vascular endothelium protection, brain protection and decompressive craniectomy were carried out. Rehabilitation training was then performed for 6 mo. At present, she has poor speaking ability and decreased muscle strength on the right side.
There is a risk of thrombosis during any period of OHSS. During in vitro assisted reproduction, for cases with a family history of thrombosis, hyperlipidemia and other high-risk factors, serum lipid levels should be controlled as soon as possible to improve metabolic dysfunction. When thrombosis occurs, timely and effective treatment should be performed to improve the prognosis.
Core Tip: Arterial thrombosis is a serious and rare complication of ovarian hyperstimulation syndrome (OHSS), which can be life-threatening without timely treatment. Herein, we report a case of OHSS complicated by common carotid artery thrombosis and malignant middle cerebral artery infarction after egg retrieval and before embryo transfer. Based on the characteristics of this case, we conclude that thrombosis may occur during any period of OHSS. During in vitro assisted reproduction, for cases with high risk factors for thrombosis (such as hyperlipidemia), metabolic dysfunction should be corrected. When thrombosis occurs, timely and effective treatment should be performed to improve the prognosis.
- Citation: Xu YT, Yin QQ, Guo ZR. Common carotid artery thrombosis and malignant middle cerebral artery infarction following ovarian hyperstimulation syndrome: A case report. World J Clin Cases 2022; 10(26): 9478-9483
- URL: https://www.wjgnet.com/2307-8960/full/v10/i26/9478.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i26.9478
Ovarian hyperstimulation syndrome (OHSS), a rare and unique complication associated with in vitro assisted reproduction, is an excessive response to exogenous gonadotropins, which is characterized by multiple follicles in bilateral ovaries, enlarged ovaries, abnormal capillary permeability, and abnormal extravasation of body fluids and proteins. It is diagnosed based on symptoms (such as abdominal distension), physical examination (such as enlarged ovaries), imaging examination (such as ascites), and laboratory examination (such as coagulation abnormalities and hormone levels). According to Golan’s classification[1], it is divided into mild (grade 1 and 2), moderate (grade 3) and severe OHSS (grade 4 and 5). Severe OHSS may cause renal failure, hypovolemic shock, thromboembolism, respiratory distress syndrome, and even death. Thrombosis is a serious complication of OHSS with an incidence rate of 0.11%[2]. Arterial thrombosis as a complication of OHSS is extremely rare, which can be life-threatening without timely treatment. In this report, we describe a case of OHSS complicated by common carotid artery thrombosis and malignant middle cerebral artery infarction after egg retrieval and before embryo transfer.
One week after egg harvesting, the patient developed abdominal distension which lasted for 3 d and coma which lasted for 2 h.
Abdominal distension started 3 d before presentation with coma.
The patient underwent in vitro fertilization for unexplained infertility. Egg retrieval was performed 7 d ago but embryo transfer had not yet been performed.
The patient had a family history of thrombosis but denied a history of polycystic ovary syndrome.
Physical examination showed the following: blood pressure 80/50 mmHg, heart rate 120 bpm, well-proportioned body, subcoma, obvious abdominal distension, positive shifting dullness, high muscle tone, and Babinski sign (+). National Institutes of Health Stroke Scale (NIHSS) score at admission was 29. Gynecological examination showed that the masses were palpable on both sides of the adnexal areas, with a mass size of 9 cm × 7 cm × 7 cm on the left side, and a mass size of 12 cm × 8 cm × 8 cm on the right side.
As shown in Table 1, blood tests revealed the following: white blood cell count 29.82 × 109/L, hematocrit 0.454, platelet count 269 × 109/L, hemoglobin 151 g/L, fibrinogen content 5.19 g/L, antithrombin III 85.3%, total cholesterol 5.71 mmol/L, triglycerides 2.81 mmol/L, free fatty acids 1.34 mmol/L, low-density lipoprotein cholesterol 3.76 mmol/L, homocysteine 9.4 μmol/ L, high-density lipoprotein cholesterol 1.05 μmol/L, and estrogen 15781 pmol/L.
| Items | Results |
| Blood count | White blood cell count 29.82 × 109/L, hematocrit 0.454, platelet count 269 × 109/L, hemoglobin 151 g/L |
| Coagulation factor | Fibrinogen content 5.19 g/L, antithrombin III 85.3% |
| Blood lipid level | Total cholesterol 5.71 mmol/L, triglycerides 2.81 mmol/L, free fatty acids 1.34 mmol/L, low-density lipoprotein cholesterol 3.76 mmol/L, homocysteine 9.4- μmol/L, high-density lipoprotein cholesterol 1.05 μmol/L |
| Hormone level | Estrogen 15781 pmol/L |
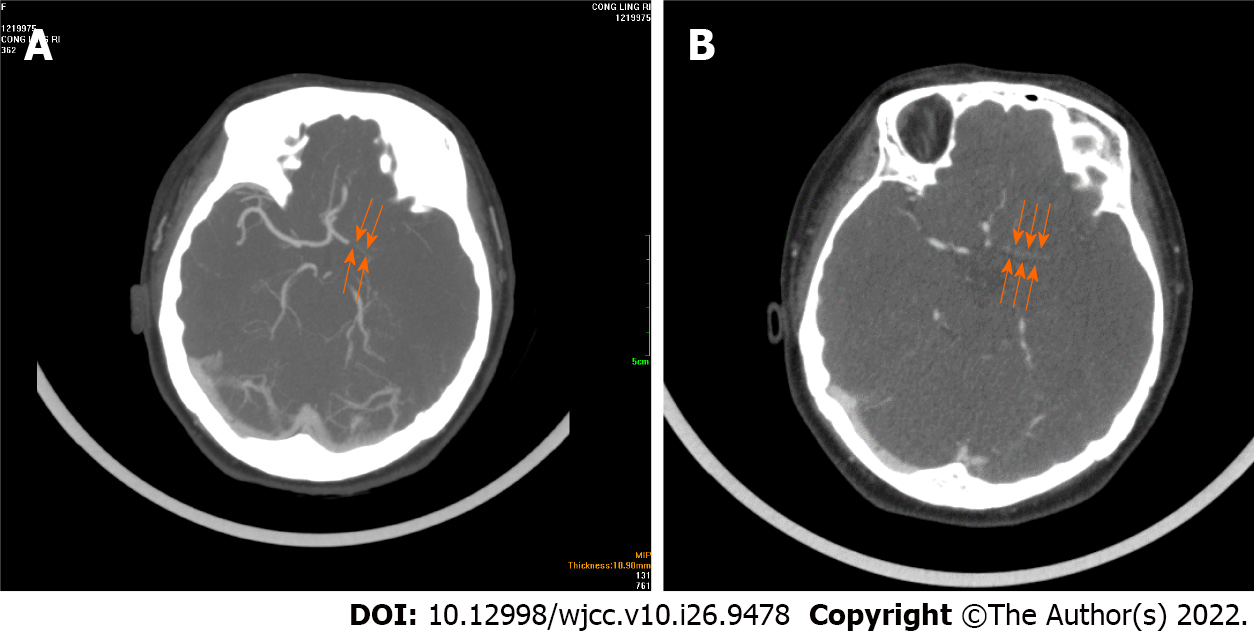
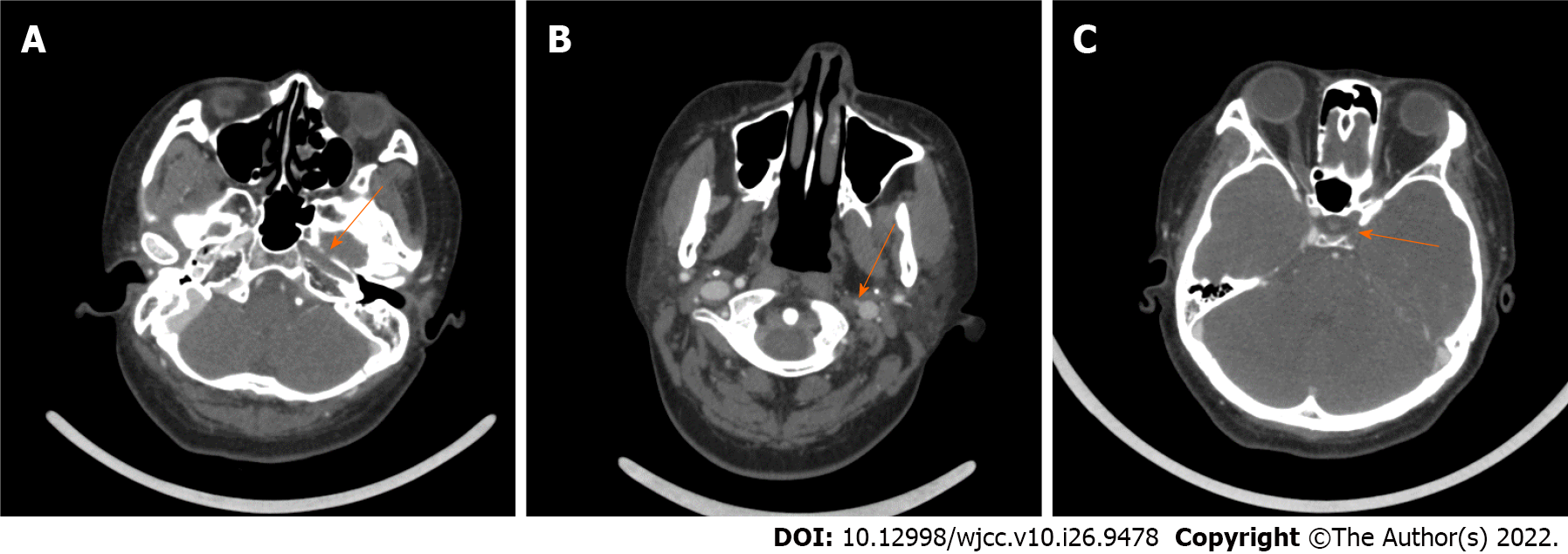
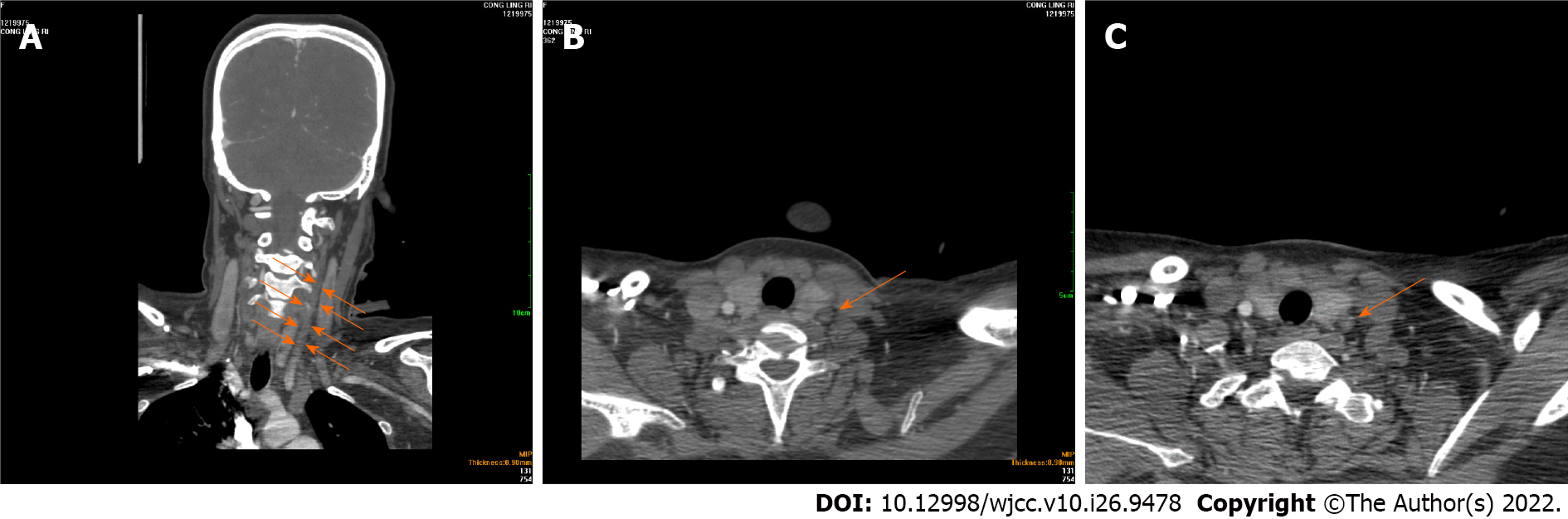
Gynecological color Doppler ultrasound showed that both ovaries were enlarged. The size of the left ovary and right ovary was approximately 9.0 cm × 6.6 cm and 12.0 cm × 7.9 cm, respectively. Abdominal cavity B-ultrasound showed a lot of ascites with the largest anteroposterior diameter of the dark area of about 6.2 cm. These findings indicated severe OHSS. Head magnetic resonance imaging + magnetic resonance angiography (MRA) observed a large area of fresh malignant middle cerebral artery infarction on the left side, suggesting occlusion of the middle cerebral artery (Figure 1) and the left internal carotid artery (Figure 2). On head and neck computed tomography angiography (CTA), the left carotid artery, internal carotid artery, and left middle cerebral artery were occluded, suggesting common carotid artery thrombosis (Figure 3).
The final diagnosis was OHSS complicated by common carotid artery thrombosis and malignant middle cerebral artery infarction.
Fluid replacement, anticoagulation with low molecular weight heparin sodium, vascular endothelium protection with atorvastatin, brain protection with edaravone and butylphthalide, and, intracranial pressure reduction with mannitol and furosemide were administered. During treatment, decompression with left side craniectomy was performed due to worsened cerebral edema. Symptomatic and rehabilitation treatment were performed following surgery.
At present, the speaking ability of the patient is awkward. She can walk a few steps with support. The left limb muscle strength is level 5, left muscle tone is normal, and left pathology sign is (-). The right upper limb muscle strength is level 2, right lower limb muscle strength is level 4, right muscle tone is decreased, and right pathological sign is (+). The discharge NIHSS score was 8. The patient is under constant follow-up.
Malignant middle cerebral artery infarction is a devastating type of ischemic stroke. The main clinical factors associated with malignant middle cerebral artery infarction include decreased level of consciousness, nausea or vomiting, and heavy smoking[3]. The most closely related pathogenesis of carotid artery thrombosis is atherosclerotic plaque. Other mechanisms of carotid artery thrombosis include hypercoagulability, hyperfibrinogenemia, hyperlipidemia, and antiphospholipid syndrome[3,4]. Digital subtraction angiography is the gold standard for the diagnosis of carotid artery thrombosis[5], but MRA, CTA or Doppler ultrasound can also be used to confirm carotid artery thrombosis.
The incidence of OHSS complicated by thrombosis is only 0.04%[6]. Of the thromboses associated with OHSS, arterial thrombosis accounts for 19%, which usually occurs at the same time as OHSS, and within 2 wk after embryo transfer (average 10 d). Venous thrombosis related to OHSS accounts for 81%, which usually occurs within 1 wk to 3 mo of pregnancy after embryo transfer, or after the relief of clinical OHSS symptoms (an average of 40 d to 42 d after embryo transfer), and mostly located in upper limbs[7-9].
In the present study, the patient underwent in vitro fertilization for unexplained reasons, denied a history of polycystic ovary syndrome, and had a family history of thrombosis. Abdominal distension occurred during the assisted pregnancy. Hyperlipidemia and shifting dullness were found during physical examination. B-ultrasound indicated ascites and the size of bilateral ovaries increased. The estrogen level increased to 15781 pmol/L, the red blood cell ratio was 0.454, and the white blood cell count was 29.82 × 109/L, suggesting severe OHSS. Common carotid artery thrombosis formed after egg retrieval (before embryo transfer), involving the internal carotid, external carotid and intracranial arteries. The thrombosis had a wide range and large area, and occurred earlier than the peak of OHSS.
The main pathological basis of arterial thrombosis is endothelial cell damage in the vascular wall, which mostly results from atherosclerosis and abnormal lipid metabolism, and further induces platelet aggregation and initiates the coagulation and fibrinolysis system[10]. Hyperlipidemia can cause changes in the composition and function of blood coagulation factors, increase blood viscosity, slow blood flow and local vortex formation, and thereby promote thrombosis[11,12]. OHSS patients can develop an increase in the number of white blood cells. The activated multinucleated leukocytes and neutrophils can produce a large amount of reactive oxygen species and cathepsin G, and the increased level of ovarian-derived inflammatory cytokines can cause vascular endothelial cell damage[13]. The patient in this report developed OHSS during in vitro assisted reproduction, which was complicated by hyperlipidemia. OHSS and hyperlipidemia may together result in thrombosis. It has been shown that 47% of patients with arterial thrombosis have a hypercoagulable state[4]. In this study, the patient had severe OHSS and high levels of estrogen. High levels of estrogen can increase vascular permeability, leading to hemoconcentration, hypovolemia, further activation of vasoactive substances, and, hypercoagulability, which may be the cause of carotid artery thrombosis and non-atherosclerotic plaque. In young adults, cerebral infarction and vascular brain disease can also be caused by hematological disorders[14]. The patient in this report should receive further tests to exclude thrombosis due to blood diseases, such as factor V Leiden, prothrombin gene mutation, plasma homocysteine, aCL antibody, lupus anticoagulant, anti-2 glycoprotein I antibody, etc.
Our patient also had a family history of venous thromboembolism, suggesting the possibility of inherited thrombophilia. Thrombophilia is a disease state that is prone to thromboembolism due to gene mutations leading to a lack of anticoagulant protein or deficiency of coagulation factor and plasminogen[15]. According to the etiology, it is divided into inherited thrombophilia and acquired thrombophilia. The main clinical feature of thrombophilia is thrombosis proneness. Anticoagulant protein deficiency is the most common disease in the Chinese population[16]. The patient in this study displayed the characteristics of inherited thrombophilia. She and her relatives should receive further measurement of antithrombin III activity, protein S activity and protein C activity to evaluate the risk of thrombosis, thus providing valuable evidence for early anticoagulation in assisted reproduction.
In summary, during assisted reproduction, OHSS should be actively prevented, and physicians should be highly vigilant of the risk of thrombosis during any period of OHSS. For OHSS patients with iatrogenic or non-iatrogenic risk factors of thrombosis, and a family history of thrombosis and hyperlipidemia, early evaluation and control of lipid levels should be performed to minimize the occurrence of thrombosis and improve the prognosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Arboix A, Spain; Hannun P, Brazil S-Editor: Wang DM L-Editor: Webster JR P-Editor: Wang DM
| 1. | Golan A, Ron-el R, Herman A, Soffer Y, Weinraub Z, Caspi E. Ovarian hyperstimulation syndrome: an update review. Obstet Gynecol Surv. 1989;44:430-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 569] [Cited by in RCA: 517] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 2. | Wang N, Chen Z, Guo X, Cheng H, Wang P, Wang T, Wang L, Tash D, Ren P, Zhu B, Guan D, Zhang G, Zhao R. Sudden Death Due to Severe Ovarian Hyperstimulation Syndrome: An Autopsy-Centric Case Report. Am J Forensic Med Pathol. 2021;42:88-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Arboix A, García-Eroles L, Oliveres M, Comes E, Sánchez MJ, Massons J. Malignant middle cerebral artery infarction: a clinical study of 32 patients. Rev Invest Clin. 2015;67:64-70. [PubMed] |
| 4. | Ferrero E, Ferri M, Viazzo A, Labate C, Pecchio A, Berardi G, Piazza S, Cumbo P, Nessi F. Free-floating thrombus in the internal carotid artery: diagnosis and treatment of 16 cases in a single center. Ann Vasc Surg. 2011;25:805-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Elijovich L, Mainali S, Doss V, Arthur A, Watridge C. Medical management of free-floating carotid thrombus. Clin Neurol Neurosurg. 2013;115:1532-1535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Ma YL, Zhang X, Xu X, Zhang D, Xu Y. Late-onset cerebral venous and sinus thrombosis after ovarian hyperstimulation syndrome in in vitro fertilization: a case report and literaturereview. Zhonghua Shengzhi Yu Biyun Zazhi. 2018;38:509-512. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Mor YS, Schenker JG. Ovarian hyperstimulation syndrome and thrombotic events. Am J Reprod Immunol. 2014;72:541-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Kasum M, Danolić D, Orešković S, Ježek D, Beketić-Orešković L, Pekez M. Thrombosis following ovarian hyperstimulation syndrome. Gynecol Endocrinol. 2014;30:764-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Huang KL, Hsu TY, Tsai CC, Ou YC, Lan KC. Right neck venous thrombosis following ovarian hyperstimulation syndrome in a patient with protein S deficiency: A case report and review of literature. Taiwan J Obstet Gynecol. 2021;60:148-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Wang LH, Zhang LM, Chen T. Research progress in the etiology and pathogenesis of carotid artery thrombosis. Shiyong Linchuang Yixue. 2014;15:134-137. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Ji F, Xu X. Comparative observation of the effects of three statins in the treatment of elderly atherosclerotic acute cerebral infarction with hyperlipidemia. Shandong Medicine 2014; 24:50-52.. [DOI] [Full Text] |
| 12. | Chen RY, Gao SL, Zheng QC. Study on the correlation between carotid atherosclerotic plaque and blood lipids and blood pressure in patients with acute cerebral infarction. Zhongguo Laonianxue Zazhi. 2011;31:2220-2221. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Li X, Zheng J. Mechanical thrombectomy for middle cerebral artery occlusion associated with ovarian hyperstimulation syndrome: case report and review of the literature. Ann Palliat Med. 2021;10:3504-3509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Arboix A, Jiménez C, Massons J, Parra O, Besses C. Hematological disorders: a commonly unrecognized cause of acute stroke. Expert Rev Hematol. 2016;9:891-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 15. | Fu YQ, Wang SY, Jia CW. Research progress in the diagnosis and treatment of in vitro fertilization-embryo transfer-related thrombophilia. Zhongguo Linchuang Yisheng Zazhi. 2020;48:535-538. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Song WT, Liu FH. Screening and research progress of thrombophilia. Jibing Jiance Yu Kongzhi. 2018;6:199-202. [DOI] [Full Text] |