Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9428
Peer-review started: April 16, 2022
First decision: June 7, 2022
Revised: June 9, 2022
Accepted: August 5, 2022
Article in press: August 5, 2022
Published online: September 16, 2022
Processing time: 139 Days and 1.3 Hours
Students in the 9th grade of junior high school in Changsha were under a 75 d lockdown due to the coronavirus disease 2019 (COVID-19) pandemic. After the resumption of school post-lockdown, the 9th grade students in Changsha faced the entrance physical examination test for senior high school.
We report on 3 cases of occult fracture on the same site in adolescents of the same grade since resumption of school after the lockdown from the COVID-19 pandemic. Three students in the 9th grade of junior high school who were facing the physical examination in 2 wk were diagnosed with an occult fracture of the distal femur.
It is recommended that the students, parents, education providers and policy makers should all pay attention to the physical exercise of students when the resumption of school after lockdown occurs and they should be aware of occult fractures when the adolescents have pain after physical exercise.
Core Tip: We report about 3 cases of occult fracture on the same site in adolescents of the same grade since resumption of school after lockdown from the coronavirus disease 2019 pandemic. It is recommended that the students, parents, education providers and policy makers should all pay attention to the physical exercise of students with the resumption of school after lockdown and they should be aware of occult fractures when the adolescents experience pain after physical exercise.
- Citation: Wang KJ, Cao Y, Gao CY, Song ZQ, Zeng M, Gong HL, Wen J, Xiao S. Resumption of school after lockdown in COVID-19 pandemic: Three case reports. World J Clin Cases 2022; 10(26): 9428-9433
- URL: https://www.wjgnet.com/2307-8960/full/v10/i26/9428.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i26.9428
Students in the 9th grade of junior high school in Changsha were under 75 d of lockdown due to the coronavirus disease 2019 (COVID-19) pandemic. After the resumption of school post-lockdown, the 9th grade students in Changsha faced the entrance physical examination test for senior high school. Therefore, these students started hard physical training for examination immediately after the prolonged lockdown. As a result, some of them suffered occult fractures from physical training due to less exercise during the lockdown period. The present study reports an occult fracture of the distal femur of 3 students in the 9th grade of junior high school facing a physical examination. Thus, the occult fracture should attract the attention of all students, parents, and teachers facing physical training examinations after school resumption.
An occult fracture refers to a fracture that cannot be detected on X-ray but can be confirmed by magnetic resonance imaging (MRI) or computed tomography (CT)[1]. Occult fracture includes complete and incomplete fractures. In clinical practice, complete occult fracture leads to fracture displacement, while incomplete occult fracture rarely causes fracture displacement and is mainly manifested as local pain and limited function[2]. In this study, 3 cases of adolescent occult fracture are reported.
Case 1: Male, 14-years-old, was admitted in the outpatient department because of "pain of the right knee joint with limited activity for 3 d after a 1 km long-distance running training".
Case 2: Male, 14-years-old, was admitted in the outpatient department because of "pain under the left knee joint for 2 d after a 1 km long-distance running training".
Case 3: Female, 13-years-old, was admitted in the outpatient department because of "pain on the right knee joint after 1 km running training for 1 d".
All 3 cases feel pain after a 1000-m long-distance running training.
Case 1: The patient endured the pain and completed the long-distance running.
Case 2: The patient terminated the training immediately and was sent to the school Infirmary.
Case 3: The patient continued training and visited the hospital after 1 d.
Past medical history of all 3 cases were negative.
Personal and family history, medication history, social history and allergic history of all 3 cases were negative.
Case 1: Height 167 cm, weight 53 kg, body mass index (BMI) 19.0, slight swelling of the right knee joint, local tenderness at the posterior and lateral side of the distal femur, slight limitation of the right knee joint activity, range of activity in the extension of 10° to the flexion of 110°, floating patella test (-), McMurray test (-) and drawer test (-).
Case 2: Height 168 cm, weight 48 kg, BMI 17.0, slight swelling of the left knee joint, local tenderness in the proximal part of the left tibia, unrestricted movement of the left knee joint, the range of motion was 0°-120°, floating patella test (-), McMurray test (-) and drawer test (-).
Case 3: Height 164 cm, weight 49 kg, BMI 18.2, slight swelling of the right knee joint, local tenderness in the distal part of the right femur, unrestricted movement of the left knee joint, the range of motion was 0°-120°, floating patella test (-), McMurray test (-) and drawer test (-).
All 3 cases: Blood regular test (-), C-reactive protein (-), erythrocyte sedimentation rate (-), serum calcium (-), 1,25-(OH)2-VitD3 test (-) and rheumatism factors test (-).
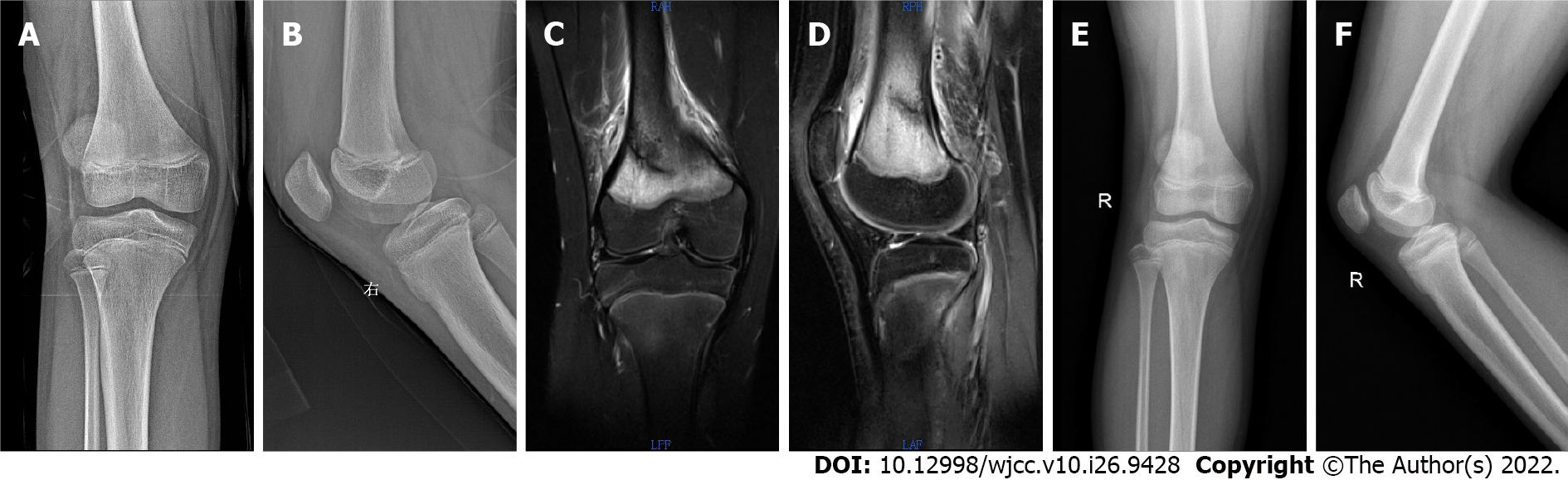
Case 1: Right knee joint positive and lateral radiograph (-) (Figure 1A and B), bone mineral density (BMD) (-), MRI of right knee joint shows posterior and lateral incomplete fracture of right distal femur (Figure 1C and D).
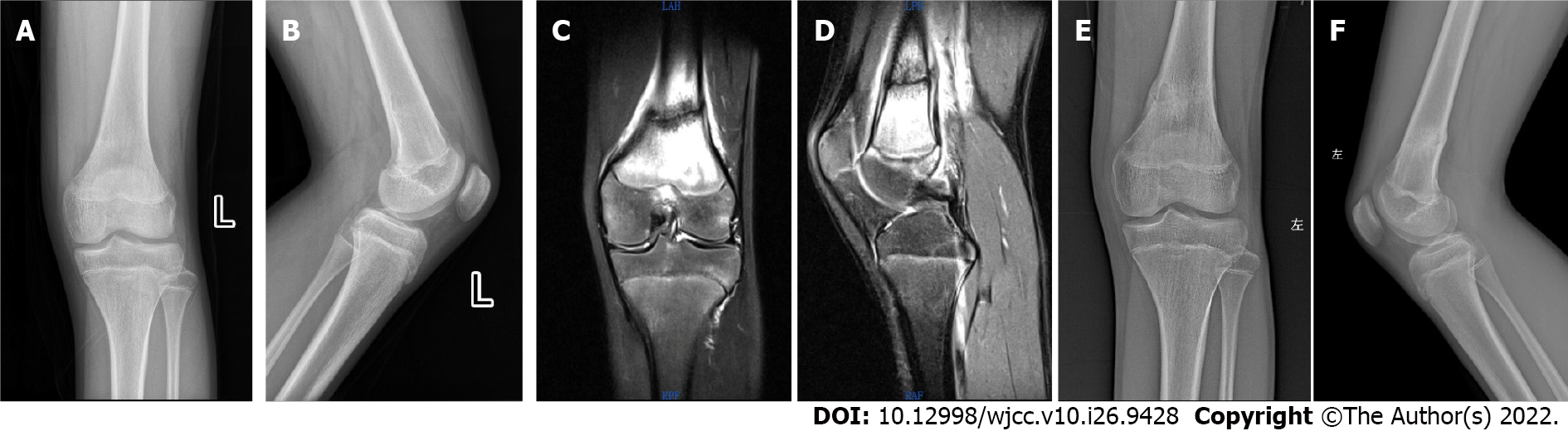
Case 2: Left knee joint (+), lateral radiograph (-) (Figure 2A and B), BMD (-), left knee joint MRI showed the left distal femur occult fracture (Figure 2C and D).
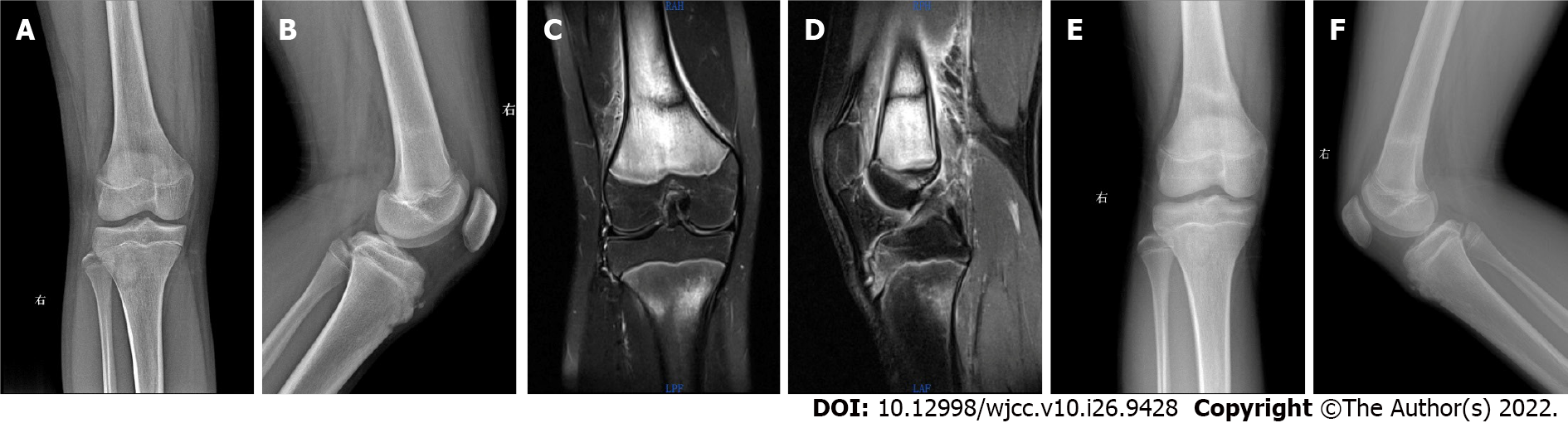
Case 3: Right knee joint (+), lateral radiograph (-) (Figure 3A and B), BMD (-), MRI of right knee joint showed an incomplete fracture of the right distal femur (Figure 3C and D).
Case 1: Right posterolateral occult incomplete fracture.
Case 2: Incomplete occult fracture of the left distal femur.
Case 3: Incomplete occult fracture of the distal right femur.
The injured lower limb in all 3 cases was fixed with plaster and was free of weight-bearing for 4 wk, light weight bearing for 2 wk and then gradual return to normal activity. Also, high calcium and protein diet was given to all three patients.
In 8 wk, X-rays showed good fracture healing (Figure 1E and F, Figure 2E and F, Figure 3E and F), and the patients were admitted to running training.
After the resumption of school post-lockdown in the COVID-19 pandemic, the 9th grade students in Changsha faced the entrance physical examination test for senior high school.This caused a sudden increase in the amount of exercise, which increases the weight-bearing, muscle contraction of the lower extremities, the strength exerted on the lower extremities and the risk of fracture.
The 3 cases we reported are students in the 9th grade of junior high school. This year, they undertook an entrance physical examination test for senior high school 1 mo after returning to school. Therefore, after the beginning of school, they immediately undertook long-distance or short-distance running training. The amount of exercise increased suddenly and the pain symptoms effectuated the process of exercise, indicating that excessive exercise is the cause of fracture. In the subsequent X-ray, MRI, BMI, serum calcium, 1,25-(OH)2-VitD3, rheumatism factors and other laboratory tests, the diagnosis of pathological fracture was excluded. Thus, the diagnosis of fracture should be considered when there is a history of a sudden increase in the amount of exercise; the pain is localized in the same area in different physical examinations and was confirmed by further imaging examination.
The main pathological changes of occult fracture were trabecular fracture, no cortical disruption, local intra-cancellous edema and hemorrhage[3,4]. Although no cortical interruption is detected, it is not sufficient to cause a noticeable change in the X-ray attenuation coefficient, such that the plain X-ray film has no abnormal signs[5]. MRI displayed local hyperemia of bone marrow and transitional perfusion of the capillary bed which led to bone marrow edema. Free water increases during edema. A series of changes in the local chemical composition of bone tissue altered the MRI relaxation time and abnormal signal changes[6-8]. Therefore, no obvious fracture line and surrounding soft tissue hematoma were detected in the first X-ray examination for the three children in this study. However, the local pain of the child had not improved significantly after rest. A hidden fracture was suspected in combination with the patient’s history of significantly increased activity in the recent period. Thus, an MRI examination was recommended. Suppose the MRI examination could not be performed temporarily. In that case, the fracture fixation is recommended according to the pain area. This is then dealt with after the MRI examination is completed or the X-ray data reviewed after 3-4 wk to detect callus formation which helps in the diagnosis.
The bone tissue of adolescents is in the stage of rapid growth; hence, the metaphyseal bone is weak rendering it easy to fracture under external force[9,10]. In this study, 2/3 cases were males and 1/3 was a female (13-14-years-old) which matched the principles.
Occult fracture is often an incomplete fracture and thus the probability of displacement is less. Also, the healing can be smooth under the protection of plaster and other externalfixation[11-12]. Moreover, callus formation was observed on the X-ray film after 8 wk of follow-up and the functions of all patients were restored.
The present study focuses on occult fracture at a particular location within an unique period in a specific population. Adolescents were under lockdown at home for a long time due to the pandemic. Thus, after school resumes, the students, parents, education providers and policymakers should focus on students’ lack of physical exercise before examination training. The sudden increase in the amount of exercise may cause a hidden fracture in young people.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pediatrics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Giacomelli L, Italy; Khan MA, United Arab Emirates; Liu J, United States; Primadhi RA, Indonesia S-Editor: Wang DM L-Editor: Filipodia P-Editor: Wang DM
| 1. | Mink JH, Deutsch AL. Magnetic resonance imaging of the knee. Clin OrthopRelat Res. 1989;29-47. [PubMed] |
| 2. | Vellet AD, Marks PH, Fowler PJ, Munro TG. Occult posttraumatic osteochondral lesions of the knee: prevalence, classification, and short-term sequelae evaluated with MR imaging. Radiology. 1991;178:271-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 262] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 3. | Mandalia V, Fogg AJ, Chari R, Murray J, Beale A, Henson JH. Bone bruising of the knee. Clin Radiol. 2005;60:627-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 64] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Griffith JF, Roebuck DJ, Cheng JC, Chan YL, Rainer TH, Ng BK, Metreweli C. Acute elbow trauma in children: spectrum of injury revealed by MR imaging not apparent on radiographs. AJR Am J Roentgenol. 2001;176:53-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Rangger C, Kathrein A, Freund MC, Klestil T, Kreczy A. Bone bruise of the knee: histology and cryosections in 5 cases. Acta OrthopScand. 1998;69:291-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 118] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Johnson DL, Urban WP Jr, Caborn DN, Vanarthos WJ, Carlson CS. Articular cartilage changes seen with magnetic resonance imaging-detected bone bruises associated with acute anterior cruciate ligament rupture. Am J Sports Med. 1998;26:409-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 218] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 7. | Mink JH, Deutsch AL. Occult cartilage and bone injuries of the knee: detection, classification, and assessment with MR imaging. Radiology. 1989;170:823-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 302] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 8. | Farr JN, Tomás R, Chen Z, Lisse JR, Lohman TG, Going SB. Lower trabecular volumetric BMD at metaphyseal regions of weight-bearing bones is associated with prior fracture in young girls. J Bone Miner Res. 2011;26:380-387. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Sadineni RT, Pasumarthy A, Bellapa NC, Velicheti S. Imaging Patterns in MRI in Recent Bone Injuries Following Negative or Inconclusive Plain Radiographs. J Clin Diagn Res. 2015;9:TC10-TC13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Bahk YW, Jeon HS, Kim JM, Park JM, Chung YA, Kim EE, Kim SH, Chung SK. Novel use of gamma correction for precise (99m) Tc-HDP pinhole bone scan diagnosis and classification of knee occult fractures. Skeletal Radiol. 2010;39:807-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Davies NH, Niall D, King LJ, Lavelle J, Healy JC. Magnetic resonance imaging of bone bruising in the acutely injured knee--short-term outcome. Clin Radiol. 2004;59:439-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Kaplan PA, Walker CW, Kilcoyne RF, Brown DE, Tusek D, Dussault RG. Occult fracture patterns of the knee associated with anterior cruciate ligament tears: assessment with MR imaging. Radiology. 1992;183:835-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 136] [Article Influence: 4.1] [Reference Citation Analysis (0)] |