Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9378
Peer-review started: April 6, 2022
First decision: June 16, 2022
Revised: July 2, 2022
Accepted: August 5, 2022
Article in press: August 5, 2022
Published online: September 16, 2022
Processing time: 148 Days and 14.1 Hours
Hypoparathyroidism is uncommon, and cataracts secondary to hypoparathyroidism are even rarer. Herein, we report a case of bilateral cataracts following hypoparathyroidism.
A 27-year-old man presented to our hospital because of painless and progressive visual impairment of both eyes over two years. He was previously diagnosed with hypocalcemia but did not take calcium supplements regularly. He had no history of anterior neck thyroid surgery. After admission, the biochemical analysis indicated a serum calcium level of 1.21 mmol/L and an intact parathyroid hormone level of 0 pg/mL. Ocular examination revealed bilateral symmetrical opacity of the lens presenting as punctate opacity in the posterior subcapsular cortex together with radial opacity in the peripheral cortex (N1C2P3). Phacoemulsification with an intraocular lens was performed in both eyes sequentially. Postoperatively, the patient had a satisfactory recovery and greatly improved visual acuity.
This patient had hypocalcemia owing to idiopathic parathyroid insufficiency. Hypoparathyroidism may go unnoticed for years but with some latent clinical manifestations, such as bilateral symmetrical posterior subcapsular cataracts. This case report highlights that the cause of hypocalcemia in particularly young patients should be further investigated. Clinicians should be aware of hypoparathyroidism as a cause of bilateral cataracts. Early identification of hypoparathyroidism can save patients from further complications.
Core Tip: Bilateral hypocalcemic cataracts secondary to hypoparathyroidism are rarely observed in ophthalmology. The main clinical manifestation is convulsions caused by hypocalcemia in the early stage. Here, we report a case of bilateral cataract with previously diagnosed hypocalcemia but for the first time to find the cause of idiopathic parathyroid insufficiency. Hypoparathyroidism may go unnoticed for years but with some latent clinical manifestations, such as bilateral symmetrical posterior subcapsular cataracts. The cause of hypocalcemia in particularly young patients should be investigated.
- Citation: Li Y. Bilateral hypocalcaemic cataracts due to idiopathic parathyroid insufficiency: A case report. World J Clin Cases 2022; 10(26): 9378-9383
- URL: https://www.wjgnet.com/2307-8960/full/v10/i26/9378.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i26.9378
Hypoparathyroidism is a disease characterized by parathyroid hormone (PTH) deficiency. In general, it can be classified based on different modalities, including congenital or acquired, genetic or nongenetic and isolated or syndromic[1]. However, the most common cause is a complication of anterior neck thyroid surgery[2]. The clinical diagnosis of hypoparathyroidism is according to the classical manifestations in patients with a low ionized or albumin-corrected blood calcium level, hyperphosphatemia and an intact PTH level that is low or not in the normal range[3]. PTH is secreted by parathyroid glands, which are maintained by serum calcium levels; thus, the serum calcium level is the first to be affected when parathyroid glands are maldeveloped or damaged during surgery. Chronic hypocalcemia can lead to the occurrence of hypocalcemic cataracts[4]. Bilateral hypocalcemic cataracts are a rare complication of hypoparathyroidism. We encountered a case of bilateral hypocalcemic cataracts due to idiopathic parathyroid insufficiency.
Painless and progressive visual impairment of both eyes over two years.
A 27-year-old man presented to our hospital because of painless and progressive visual impairment of both eyes over two years. The patient had no other positive symptoms apart from blurred vision. The patient had no other positive symptoms apart from blurred vision. The patient had no history of ocular diseases.
He was diagnosed with hypocalcemia when he was young but did not know exactly when and the serum calcium concentration at that time. He relied on a diet of milk or calcium-containing foods and calcium tablets to supplement his calcium levels at that time but subsequently did not take regular calcium supplements. He started to experience muscle cramps in his upper extremities, less markedly in his thighs and calves approximately ten years ago. However, he did not seek help for these symptoms until the occurrence of epilepsy. Seven years ago, he underwent cerebral surgery for epileptic seizures.
The patient denied any diagnoses of personal or family history.
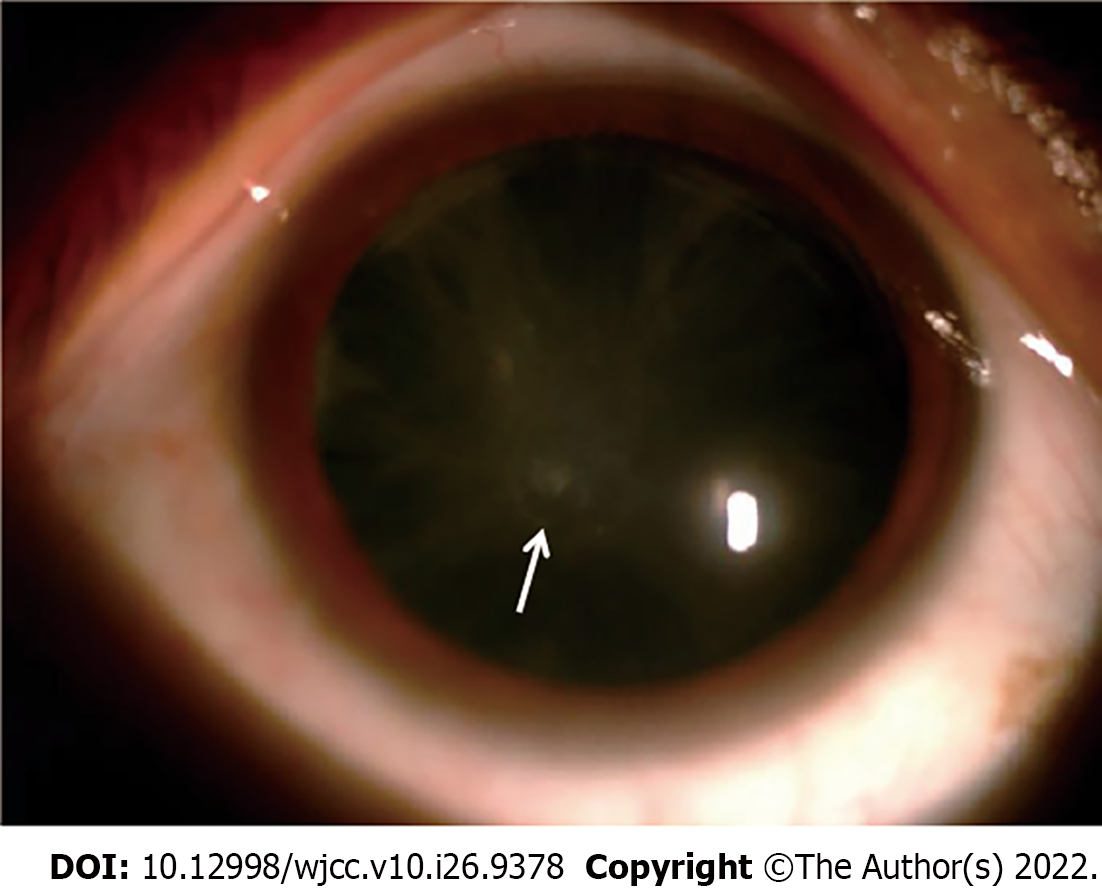
The ocular examination revealed a preoperative binocular visual acuity of 16/200, and the best-corrected visual acuity (BCVA) was not improved. The intraocular pressure in the right and left eyes was 15 mmHg and 16 mmHg, respectively. There was bilateral symmetrical opacity of the lens presenting as punctate opacity in the posterior subcapsular cortex together with radial opacity in the peripheral cortex. Fundus examination showed no pathological changes.
The biochemical analysis indicated a serum total calcium level of 1.21 mmol/L (serum ionized calcium level 0.72 mmol/L in arterial blood gas analysis), a serum phosphorus level of 1.67 mmol/L and a serum magnesium level of 0.62 mmol/L, indicating significantly low levels of serum calcium and magnesium but high serum phosphorus. His intact PTH level was 0 pg/mL. Adrenocorticotropic hormone (ACTH), cortisol hormone at 8:00 am, thyroid-stimulating hormone, thyroid hormones (TT3, TT4, FT3, FT4), whole blood count, coagulation function, renal and liver function tests were within normal limits (Table 1). An electrocardiogram showed that there was a prolonged QT interval.
| Parameter | Result | Reference |
| Calcium | 1.21 mmol/L | 2.11-2.52 mmol/L |
| Serum ionize calcium | 0.72 mmol/L | 1.10-1.30 mmol/L |
| Phosphorus | 1.67 mmol/L | 0.85-1.51 mmol/L |
| Magnesium | 0.62 mmol/L | 0.75-1.02 mmol/L |
| Parathyroid hormone (PTH) | 0 pg/mL | 12.40-76.80 pg/mL |
| Total triiodothyronine (TT3) | 1.23 ng/mL | 0.61-1.81 ng/mL |
| Total tetraiodothyronine (TT4) | 105.50 nmol/L | 58.1-140.6 nmol/L |
| Free triiodothyronine (FT3) | 3.29 pg/mL | 2.30-4.20 pg/mL |
| Free tetraiodothyronine (FT4) | 1.25 ng/dl | 0.89-1.76 ng/dl |
| Thyroid stmulatng hormone (TSH) | 2.7220 μIU/mL | 0.55-4.78 μIU/mL |
| Adrenocorticotropic hormone (ACTH) | 20.67 pg/mL | 7.20-63.30 pg/mL |
| Cortisol at 8:00 am | 13.00 μg/dL | am: 4.82-19.50 μg/dL |
| pm: 2.47-11.90 μg/dL |
Anterior segment photography revealed punctuate opacity in the posterior subcapsular cortex together with radial opacity in the peripheral cortex (Figure 1).
The diagnosis of bilateral hypocalcemic cataracts was made due to idiopathic parathyroid insufficiency.
The patient was intravenously administered a 100 mL infusion of 10% calcium gluconate in 1000 mL of 5% dextrose at a rate of 50 mL/h, and the serum calcium level increased from 1.21 mmol/L to 2.01 mmol/L. We performed phacoemulsification surgery with implantation of IOLs (Figure 2) (+20.0 diopters in right eye; +20.5 diopters in left eye; ZCB00, Johnson & Johnson, Santa Ana, United States) in both eyes at one-month intervals.
The postoperative binocular visual acuity of the BCVA was 20/20, and the patient had a satisfactory recovery with greatly improved visual acuity. He was referred to the endocrinology department for further treatment.
PTH maintains the level of ionized calcium in the blood and extracellular fluids. PTH binds to cell surface receptors in bone and kidney, thereby triggering responses that increase blood calcium. PTH also increases the renal synthesis of 1,25(OH)2D3, which then acts on intestine to augment absorption of dietary calcium, in addition to promoting calcium fluxes into the blood from bone and kidney[2]. Thyroid surgery is the most common cause of hypoparathyroidism[5]. Hypoparathyroidism also exists in the isolated form or as a syndrome related to other (usually autoimmune) disorders. Low calcium, high phosphorous, and low PTH confirmed the diagnosis of primary hypoparathyroidism[6]. Our patient had no history of any neck surgery or radiation exposure. Autoimmune adrenal involvement was also ruled out by serological tests (normal basal plasma ACTH tests) for this patient. Therefore, there were no clinical manifestations or biochemical features of Addison’s disease or mucocutaneous candidiasis, which is a type of autoimmune polyglandular syndrome[7]. Additionally, there were no characteristic symptoms of an underlying genetic disease. The biochemical analysis indicated that magnesium deficiency affects the secretion and action of PTH. When the level of magnesium in the serum decreased to 0.5 mmol/L, PTH secretion was stimulated, with severe hypomagnesemia (below 0.4 mmol/L) inhibiting PTH secretion and causing relative hypoparathyroidism[8]. The serum magnesium level in this patient was decreased but not as low as 0.4 mmol/L. Other causes of hypocalcemia were ruled out, such as metabolic disturbances, renal failure or malabsorption. The low serum calcium and magnesium but high serum phosphorus, history of chronic tetany together with bilateral cataracts and undetectable PTH fulfilled the criteria for the diagnosis of hypoparathyroidism[3]. As there were no other possible etiologies identified, his hypoparathyroidism was considered idiopathic.
The association of hypoparathyroidism and cataracts was first described in 1880[9]. Hypoparathyroidism secondary to cataracts has been reported successively[5]. The pathogenesis of cataracts in hypoparathyroidism is proposed to be membrane damage due to low calcium levels in the aqueous humour[10]. Calcium plays a crucial role in triggering intracellular signaling and regulating cellular processes. Long-term hypocalcemia can cause muscle cramps, paresthesia, seizure, etc., whereas hypercalcemia can cause ectopic calcification. Calcium homeostasis is critical for the body, as calcium maintains the growth and homeostasis of the whole lens[11,12]. For cataracts secondary to hypoparathyroidism, some literature reported that low blood calcium reduced the calcium concentration around the crystalloid capsule, which suppressed the active ion transport function of the crystalloid capsule membrane and led to water and sodium storage in the lens. The following consequences were observed: crystal fiber swelling, rupture, crystal protein denaturation, decomposition and caused cataract[13,14]. Disturbed calcium homeostasis can cause lens opacity through related mechanisms, such as abnormal differentiation of lens epithelial cells (LECs) into fibrocytes, increased migration of LECs into the posterior capsule, lens protein clustering and calcium channel inactivation[15-17]. In this case, we observed that the lens presented bilateral and symmetrical punctate opacity in the posterior subcapsular cortex together with radial opacity in the peripheral cortex. We also observed iridescent opacity in the deep layer of the cortex. The patient had experienced gradual vision loss for two years, which severely worsened in the preceding year, suggesting that the function of LECs was gradually damaged. For this patient, the main reason is hypocalcemia caused by parathyroid dysfunction, which affects the calcium homeostasis of the lens. He underwent cataract surgery, and the calcium concentration of his aqueous humor was 1.03 mmol/L, comparable to that of the aqueous humor produced by filtered serum, thereby confirming the diagnosis. However, previous researchers cultured clear lenses and LECs in culture medium containing a high concentration of Ca2+ and found that lens opacity was associated with an increase in Ca2+ concentration in vitro. An abnormally high extracellular calcium concentration could damage calcium homeostasis in LECs and eventually lead to cataracts[18]. In conclusion, disruption of calcium homeostasis in either hypercalcemia or hypocalcemia leads to cataract formation.
This patient was diagnosed with a calcium deficiency in childhood but did not take calcium supplements regularly. Additionally, there were no further investigations of the cause of the calcium deficiency, even when he underwent cerebral surgery for misdiagnosing epileptic seizures, until hypocalcemia led to bilateral cataracts. Recent studies reported that higher 25(OH)D levels in aqueous humor and serum were associated with cataracts[19-22]. However, to elucidate the role of the 25(OH)D level in cataracts, a larger clinical study is needed, including a control group of patients without cataracts. The diagnosis of hypoparathyroidism mainly depends on whether there are severe symptoms of hypocalcemia and parathyroid dysfunction. For this patient, it was not simply the lack of calcium but deficiency of PTH; therefore, he requires further standardized treatment and follow-up in the endocrinology department after ocular surgery. Although this patient may temporarily tolerate such a low concentration of serum calcium, there is still a risk of progressing to a more severe clinical presentation over time.
This patient had hypocalcemia owing to idiopathic parathyroid insufficiency. Hypoparathyroidism may go unnoticed for years but with some latent clinical manifestations, such as bilateral symmetrical posterior subcapsular cataracts. This case report highlights that the cause of cataracts with hypocalcemia should be further investigated, particularly in young patients. Clinicians should be aware of hypoparathyroidism as a cause of bilateral cataracts. Early identification of hypoparathyroidism can save patients from further complications.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Mittal M, India; Mohapatra SSD, India S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Cianferotti L, Marcucci G, Brandi ML. Causes and pathophysiology of hypoparathyroidism. Best Pract Res Clin Endocrinol Metab. 2018;32:909-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Clarke BL, Brown EM, Collins MT, Jüppner H, Lakatos P, Levine MA, Mannstadt MM, Bilezikian JP, Romanischen AF, Thakker RV. Epidemiology and Diagnosis of Hypoparathyroidism. J Clin Endocrinol Metab. 2016;101:2284-2299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 204] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 3. | Gafni R I, Collins M T. Hypoparathyroidism[J]. N Engl J Med. 2019;380:1738-1747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 74] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 4. | Triantafyllou E, Yavropoulou MP, Anastasilakis AD, Makras P. Hypoparathyroidism: is it that easy to treat? Hormones (Athens). 2019;18:55-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Daba KT, Weldemichael DK, Mulugeta GA. Bilateral hypocalcemic cataract after total thyroidectomy in a young woman: case report. BMC Ophthalmol. 2019;19:233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Bilezikian JP. Hypoparathyroidism. J Clin Endocrinol Metab. 2020;105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 117] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 7. | Eisenbarth GS, Gottlieb PA. Autoimmune polyendocrine syndromes. N Engl J Med. 2004;350:2068-2079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 352] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 8. | Vetter T, Lohse MJ. Magnesium and the parathyroid. Curr Opin Nephrol Hypertens. 2002;11:403-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 91] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Saha S, Gantyala SP, Aggarwal S, Sreenivas V, Tandon R, Goswami R. Long-term outcome of cataract surgery in patients with idiopathic hypoparathyroidism and its relationship with their calcemic status. J Bone Miner Metab. 2017;35:405-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Takahashi H. [Ca(2+)-ATPase activity in the hypocalcemic cataract]. Nippon Ganka Gakkai Zasshi. 1994;98:142-149. [PubMed] |
| 11. | Schöfl C. [Update - Calcium Metabolism]. Dtsch Med Wochenschr. 2019;144:1125-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Fang AP, Li KJ, Shi HY, He JJ, Li H. Habitual dietary calcium intakes and calcium metabolism in healthy adults Chinese: a systematic review and meta-analysis. Asia Pac J Clin Nutr. 2016;25:776-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 13. | Granström KO, Hed R. Idiopathic hypoparathyroidism with cataract and spontaneous hypocalcaemic hypercalciuria. Acta Med Scand. 1965;178:417-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Philipson B, Angelin B, Christensson T, Einarsson K, Leijd B. Hypocalcaemia with zonular cataract due to idiopathic hypoparathyroidism. With a note on the prevalence of severe hypocalcaemia in a health screening. Acta Med Scand. 1978;203:223-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Maddala R, Nagendran T, de Ridder GG, Schey KL, Rao PV. L-type calcium channels play a critical role in maintaining lens transparency by regulating phosphorylation of aquaporin-0 and myosin light chain and expression of connexins. PLoS One. 2013;8:e64676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Gupta PD, Johar K, Vasavada A. Causative and preventive action of calcium in cataracto-genesis. Acta Pharmacol Sin. 2004;25:1250-1256. [PubMed] |
| 17. | Gosak M, Gojić D, Spasovska E, Hawlina M, Andjelic S. Cataract Progression Associated with Modifications in Calcium Signaling in Human Lens Epithelia as Studied by Mechanical Stimulation. Life (Basel). 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Matsushima H, Mukai K, Yoshida S, Obara Y. Effects of calcium on human lens epithelial cells in vitro. Jpn J Ophthalmol. 2004;48:97-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Cho MC, Kim RB, Ahn JY, Yoo WS, Kim SJ. Aqueous humor and serum 25-Hydroxyvitamin D levels in patients with cataracts. BMC Ophthalmol. 2020;20:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Rao P, Millen AE, Meyers KJ, Liu Z, Voland R, Sondel S, Tinker L, Wallace RB, Blodi BA, Binkley N, Sarto G, Robinson J, LeBlanc E, Mares JA. The Relationship Between Serum 25-Hydroxyvitamin D Levels and Nuclear Cataract in the Carotenoid Age-Related Eye Study (CAREDS), an Ancillary Study of the Women's Health Initiative. Invest Ophthalmol Vis Sci. 2015;56:4221-4230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Jee D, Kim EC. Association between serum 25-hydroxyvitamin D levels and age-related cataracts. J Cataract Refract Surg. 2015;41:1705-1715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Park S, Choi NK. Serum 25-hydroxyvitamin D and Age-Related Cataract. Ophthalmic Epidemiol. 2017;24:281-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |