Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9348
Peer-review started: April 1, 2022
First decision: June 16, 2022
Revised: June 20, 2022
Accepted: August 5, 2022
Article in press: August 5, 2022
Published online: September 16, 2022
Processing time: 153 Days and 19.7 Hours
Difficult airway is a significant cause of anesthesia-associated death and disability. Currently, physical examinations of thyromental distance, mouth opening, Mafampaii classification, etc. combined with X-ray, computed tomography (CT), and other imaging technologies are mainly used to evaluate difficult airways. However, in many special cases, i.e., emergency surgery, imaging examinations cannot be completed preoperatively. Such patients' airway can only be evaluated through general physical examination, which inevitably increases the likelihood of an unexpected difficult airway during anesthesia.
We report a rare case of difficult intubation because of severe upper trachea distortion after induction. Emergency holmium laser lithotripsy was performed under transurethral ureteroscopy because the patient had anuria for 4 d and a creatinine level of 890 μmol/L. Due to the urgency of the condition, chest radiography or chest CT was not examined before surgery and the anesthesiologist did not evaluate the airway adequately, resulting in an unexpected difficult airway.
The incidence of tracheal malformation and tracheal stenosis is extremely low, but the risk of hypoxia and even death due to difficult airways is extremely high for such patients. It is recommended to complete preoperative imaging examinations of the airway. For life-threatening emergency patients, a pre-anesthesia reassessment should be performed and surgeons should be prepared to prevent and manage the difficult airway.
Core Tip: In this paper, we report a case of severe upper tracheal distortion resulting in an unexpectedly difficult airway. The incidence of tracheal malformation and tracheal stenosis is extremely low, but the risk of hypoxia and even death due to difficult airways is extremely high for such patients. It is recommended to complete preoperative imaging examinations of the airway. For life-threatening emergency patients, a pre-anesthesia reassessment should be performed, attention should be paid to bedside physical examination, and surgeons should be prepared to prevent and manage the difficult airway.
- Citation: Zhou JW, Wang CG, Chen G, Zhou YF, Ding JF, Zhang JW. Unexpected difficult airway due to severe upper tracheal distortion: A case report. World J Clin Cases 2022; 10(26): 9348-9353
- URL: https://www.wjgnet.com/2307-8960/full/v10/i26/9348.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i26.9348
Difficult airway is a significant cause of anesthesia-associated death and disability; a previous study suggests that 30% of anesthesia-associated death events are related to improper airway safety management[1,2]. Currently, physical examinations of thyromental distance, mouth opening, Mafampaii classification, etc. combined with X-ray, computed tomography (CT), and other imaging technologies are mainly used to evaluate difficult airways. However, in many special cases, i.e., emergency surgery, imaging examinations cannot be completed preoperatively. Such patients' airway can only be evaluated through general physical examination, which inevitably increases the likelihood of an unexpected difficult airway during anesthesia[3,4]. Herein we report the anesthesia care of a patient who underwent emergency surgery with an unexpected difficult airway due to severe upper tracheal distortion.
A male patient presented with left lumbago with anuria for 4 d.
The patient developed left lumbago and anuria for 4 d without obvious inducement. He was diagnosed with left ureteral calculi accompanied by hydronephrosis and infection, renal failure, urinary tract infection, gallbladder calculi, traumatic osteoarthropathy of the right hip joint, and hypertension.
The patient had previous hypertension for many years (taking amlodipine tablets 5 mg, QD), his blood pressure control was reasonable, and he had no headache, dizziness, or discomfort. He had a history of right hip injury in childhood, hepatitis, and tuberculosis.
This part does not cover related content.
The physical examinations revealed the following: Temperature: 36.5 °C; Pulse rate: 78 times/min; Respiration rate: 20 times/min; Blood pressure: 213/102 mmHg; Height 160 cm; Weight 55 kg; Scoliosis; Rales in the lower lungs; Deformity of the right lower limb; Percussive pain in the left kidney area (+).
Positive laboratory results mainly included C-reactive protein 47.65 mg/L, white blood cell count 12.7 × 109/L, creatinine 890 μmol/L, and potassium 4.80 mmol/L.
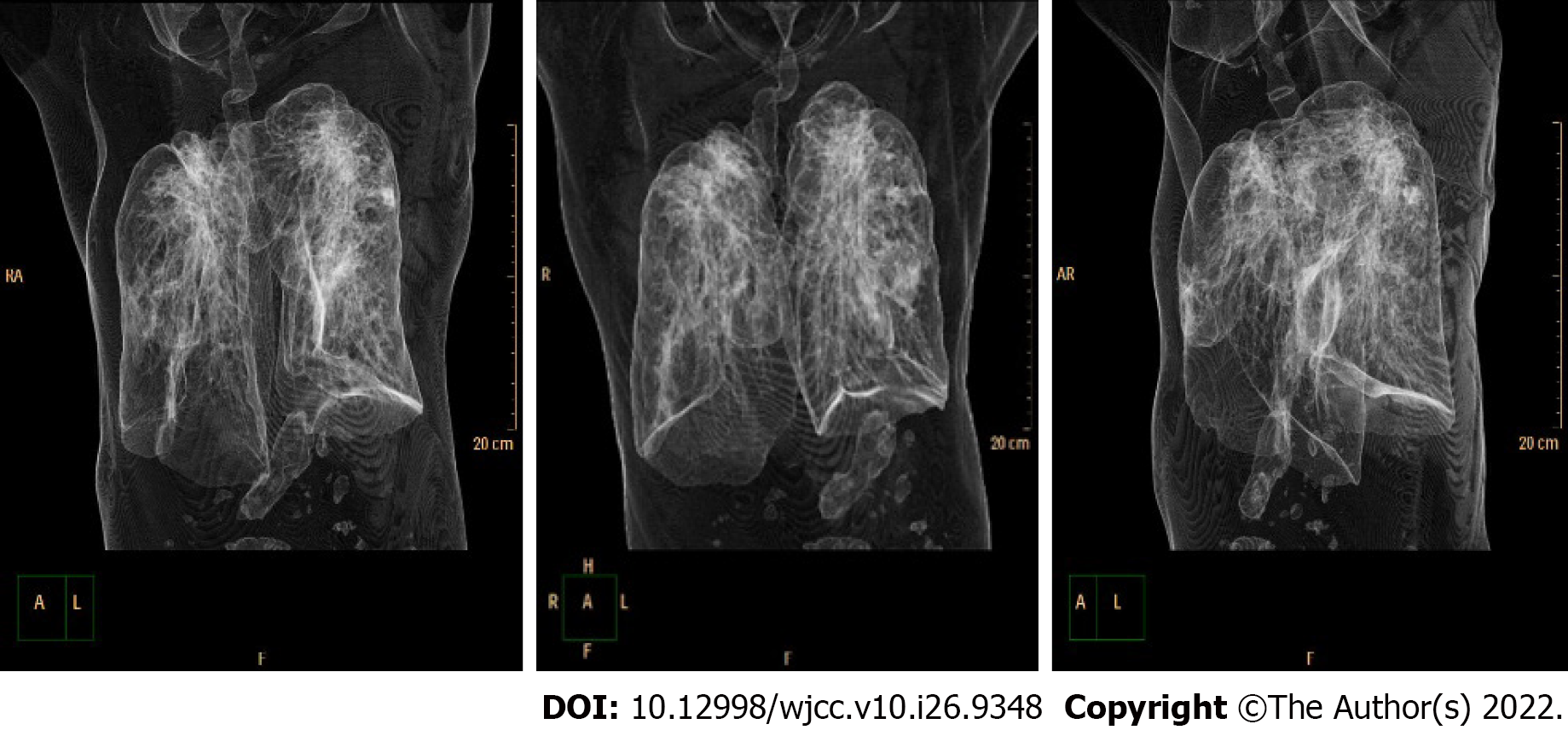
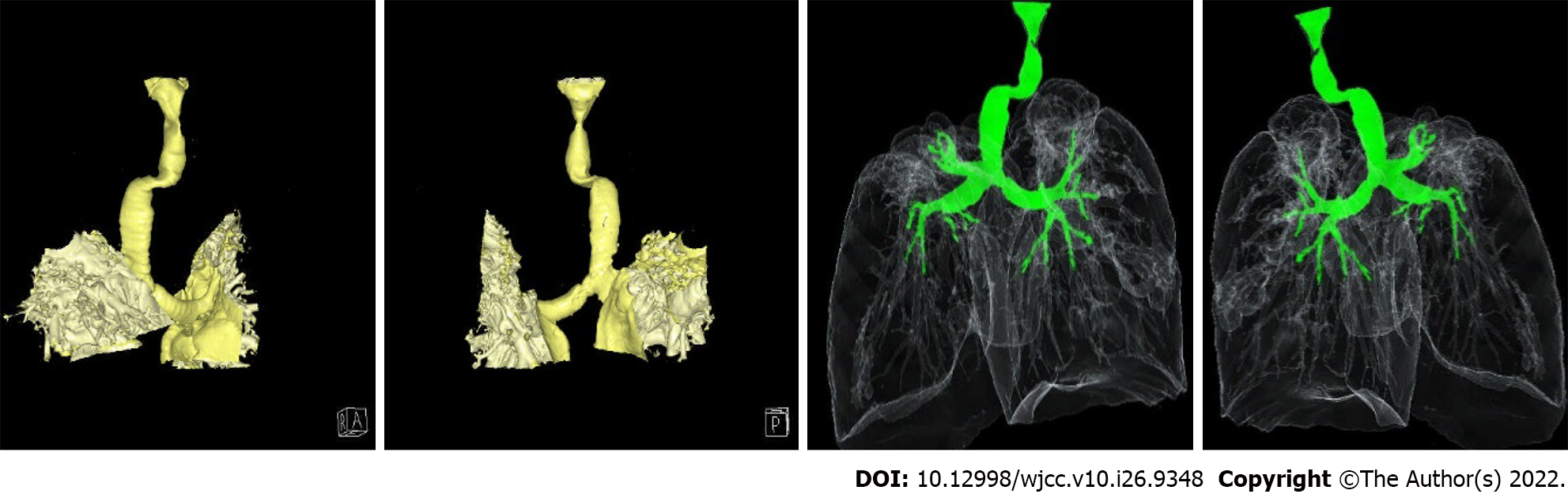
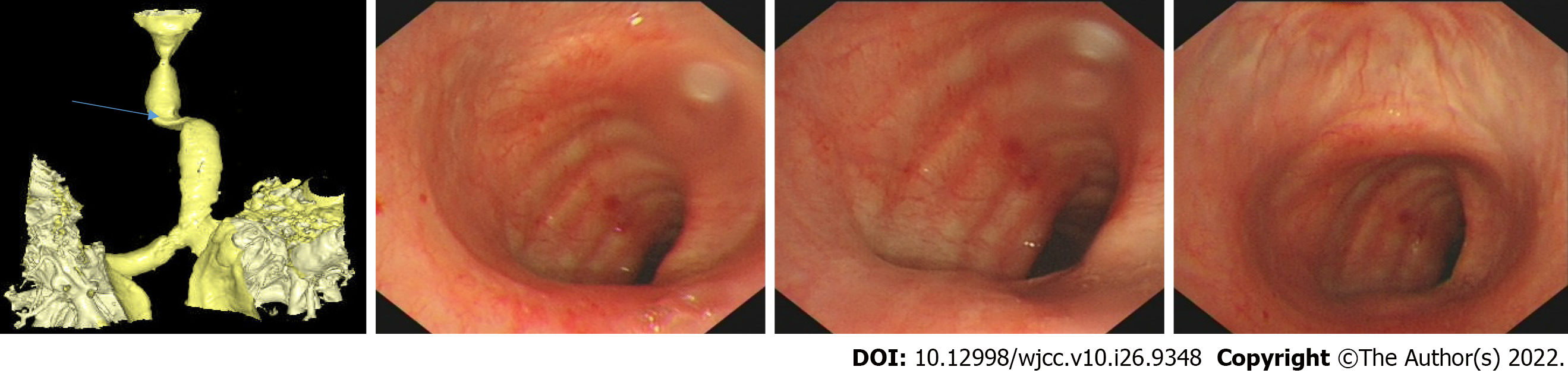
Ultrasonography of the urinary system showed nephrarctia with echogenic changes and hydronephrosis of the right kidney; compensatory renal enlargement with echogenic change and multiple renal calculi with hydronephrosis of the left kidney, as well as dilation of the left upper ureter. Abdominal CT showed left lower ureteral calculi with upper urinary tract hydropsy, ascites, nephrarctia of the right kidney, and bilateral renal small calculi. Preoperative diagnoses included renal failure, hyperkalemia, and left ureteral calculi with hydrops and infection. In order to find the real cause of the patient's unanticipated difficult airway, postoperative CT scan and 3D reconstruction of the trachea (see Figures 1 and 2) and fiberoptic bronchoscopy (see Figure 3) were performed after receiving the patient's informed consent.
The final diagnoses were as follows: (1) Ureteral calculus with hydronephrosis and infection (left); (2) Kidney failure; (3) Urinary tract infection; (4) Bronchitis; (5) Hypertension; (6) Emphysema; and (7) Traumatic arthropathy of the hip (right).
Emergency holmium laser lithotripsy was performed under transurethral ureteroscopy and general anesthesia.
No adverse events occurred, and the patient benefited from timely treatment in accordance with the guidelines.
The incidence of tracheal malformation and tracheal stenosis is extremely low, and its pathogenesis is still unclear. It is believed that factors causing abnormal differentiation of tissues and organs could lead to tracheal dysplasia or malformed changes resulting in a difficult airway perioperatively[5]. Medical risks are also different due to various factors such as the patient's characteristics, medical history, surgical method, and current condition[6]. Since the airway cannot be opened, the chance of severe complications such as cerebral hypoxia or cardiac arrest in a short period of time increases[7]. To prevent such risks clinically, airway assessment has become a critical part of preoperative risk assessment to prevent the difficult airway from causing severe anesthesia complications or even death.
A previous study has suggested that three-dimensional reconstruction of the trachea and bronchus has high sensitivity and accuracy in diagnosing tracheobronchial stenosis[8]. The patient's postoperative airway reconstruction from CT images suggested a severe rightward twist at about 2.8 cm below the glottis of the main trachea, and the twist turned laterally at about 1.1 cm and then downward until the tracheal juga. Meanwhile, tracheoscopy revealed severe twisting of the main trachea with mild stenosis. This result was consistent with the difficulty of inserting the tracheal catheter after it was 2 cm passing through the glottis and the condition of two consecutive turns found under fiberoptic bronchial guidance. It further confirmed that the patient's severe tracheal distortion caused the inability of the steel-wire reinforced tracheal tube to pass through the corner with stenosis. Due to surgical urgency, although the basic condition of the patient was assessed before anesthesia, because the patient's trachea was twisted high and close to his larynx, condition like malformation of the trachea was not detected in time during the assessment, resulting in the unexpected difficult airway. Fortunately, in this case, the anesthesiologist mastered good airway safety management skills and followed the difficult airway management guidelines to adopt standardized procedures to manage unexpected difficult airways in the critical situation, thus not leading to serious adverse consequences[9].
Further inquiry of the medical history after the operation revealed that the patient had secondary tuberculosis for more than 40 years and developed thoracic scoliosis 5 years ago, but the patient denied any history of poliomyelitis and other diseases. Considering the patient’s imaging findings, his long-term chronic secondary tuberculosis may have led to significant lateral traction of the lung tissue, which caused a twisted trachea. In addition, given the patient’s conditions of thoracic scoliosis, thoracic malformation, etc., severe tracheal distortion and stenosis caused by the above reasons cannot be ruled out. To this end, we searched the studies in multiple databases, and no report of severe trachea distortion caused by diseases, i.e., tuberculosis, was reported, while the studies and reports about etiologies of airway distortion have suggested that the history of diphtheria in childhood, airway fatty deposition, and mucopolysaccharidosis can lead to severe airway stenosis and trachea tortuosity[10-12]. However, when the patient's medical history was further inquired about after surgery to understand his specific condition, it was found that the patient had only a junior education level, paid minimal attention to his diseases, and had no relevant medical information records. As a result, the abovementioned influencing factors could not be confirmed by the patient's past illness history.
According to the above discussions, anesthesiologists should clinically pay close attention to unexpected difficult airways, especially in emergency surgery patients. Sorbello et al[13] confirmed that the commonly used clinical methods to measure airway difficulty include Mafampaii classification, thyromental distance, mouth opening, head-neck range of motion, chest-chin distance, etc. However, these methods cannot accurately predict the probability of intubation difficulty when performing laryngoscopy directly. It is believed that no perfect airway assessment tool can comprehensively address the risk assessment needs of patients with a difficult airway. In contrast, the combined analysis of multiple assessment tools can better predict complex and difficult airways[14]. The study also suggested that preoperative airway ultrasound can be used to evaluate the intubation conditions of patients. However, it is unclear which specific ultrasonic scan parameters can be used as reliable indicators for evaluating difficult airways[15,16].
Hence, when a patient does not have distinctive features of difficult airway, such as glossohypertrophia, oral soft tissue abscesses, and lack of radiological imaging results due to emergency resuscitation or other reasons, more attention should be paid to bedside assessment. Especially, preoperative airway imaging including ultrasonography of airway, pulmonary auscultation, etc. are particularly important[17-19]. The patient was in critical condition upon admission; therefore, emergency ureteroscopy holmium laser lithotripsy was performed without a preoperative chest radiology examination, resulting in inadequate preparation before anesthesia, the inability to assess the risk of anesthesia before surgery fully, as well as an unexpected difficult airway. Fortunately, no adverse event occurred due to proper management.
In summary, severe upper tracheal malformation in adult patients is very rare, but the risk of hypoxia and even death due to difficult airways is extremely high for such patients. Especially for patients with a preoperative history of neck trauma surgery, pulmonary tuberculosis, diphtheria, airway fatty deposition, mucopolysaccharidosis, etc., enough attention should be paid to perioperative anesthesia and safety management. It is recommended to complete preoperative imaging examinations of the airway as much as possible. For life-threatening emergency patients, a pre-anesthesia reassessment should be performed, attention should be paid to bedside physical examination, and surgeons always be prepared to prevent and manage the difficult airway.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee KS, South Korea; Pandey NM, India; Tsuchiya M, Japan S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Xia M, Cao S, Zhou R, Wang JY, Xu TY, Zhou ZK, Qian YM, Jiang H. Acoustic features as novel predictors of difficult laryngoscopy in orthognathic surgery: an observational study. Ann Transl Med. 2021;9:1466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 2. | Cook TM, MacDougall-Davis SR. Complications and failure of airway management. Br J Anaesth. 2012;109 Suppl 1:i68-i85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 269] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 3. | Yi H, Wang K, Liang CB. One Elderly Patient with Unexpected Difficult Airway: Secondary Tracheal Distortion Caused by Cervical Vertebra Surgery in Childhood. Zhonghua Mazuixue Zazhi. 2021;41:256. [DOI] [Full Text] |
| 4. | Foz C, Peyton J, Staffa SJ, Kovatsis P, Park R, DiNardo JA, Nasr VG. Airway Abnormalities in Patients With Congenital Heart Disease: Incidence and Associated Factors. J Cardiothorac Vasc Anesth. 2021;35:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Subspecialty Group of Pharyngolaryngology. Society of Otorhinolaryngology Head and Neck Surgery, Chinese Medical Association; Subspecialty Group of Phoniatrics, Society of Otorhinolaryngology Head and Neck Surgery, Chinese Medical Association; Subspecialty Group of Pharyngolaryngology of Editorial Committee of the Chinese Journal of Otorhinolaryngology Head and Neck Surgery, Chinese Medical Association. Expert Consensus on Diagnosis and Treatment of Laryngotracheal Stenosis. Zhonghua Erbiyanhoutoujing Waike Zazhi. 2018;53:410-413. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Zuercher M, Casso G, Krugel V, Potié A, Barry MP, Schoettker P. Tracheal intubation using intubating laryngeal tube iLTS-D™ and LMA Fastrach™ in 99 adult patients: A prospective multicentric randomised non-inferiority study. J Clin Anesth. 2022;78:110671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Fiadjoe JE, Nishisaki A, Jagannathan N, Hunyady AI, Greenberg RS, Reynolds PI, Matuszczak ME, Rehman MA, Polaner DM, Szmuk P, Nadkarni VM, McGowan FX Jr, Litman RS, Kovatsis PG. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med. 2016;4:37-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 286] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 8. | Toyota K, Uchida H, Ozasa H, Motooka A, Sakura S, Saito Y. Preoperative airway evaluation using multi-slice three-dimensional computed tomography for a patient with severe tracheal stenosis. Br J Anaesth. 2004;93:865-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, Fiadjoe JE, Greif R, Klock PA, Mercier D, Myatra SN, O'Sullivan EP, Rosenblatt WH, Sorbello M, Tung A. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022;136:31-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 570] [Article Influence: 190.0] [Reference Citation Analysis (0)] |
| 10. | Antoniou T, Papadopoulos K, Kampanarou S, Ftikos P, Perreas K, Theodoraki K. Secondary tracheal distortion in an adult patient after therapy for diphtheria at childhood. J Card Surg. 2020;35:1115-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Poore TS, Prager J, Weinman JP, Larson A, Houin P. Tracheal and lower airway changes in a patient with mucolipidosis type II. Pediatr Pulmonol. 2020;55:1843-1845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Gadepalli C, Stepien KM, Sharma R, Jovanovic A, Tol G, Bentley A. Airway Abnormalities in Adult Mucopolysaccharidosis and Development of Salford Mucopolysaccharidosis Airway Score. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Sorbello M, Petrini F. Supraglottic Airway Devices: the Search for the Best Insertion Technique or the Time to Change Our Point of View? Turk J Anaesthesiol Reanim. 2017;45:76-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Detsky ME, Jivraj N, Adhikari NK, Friedrich JO, Pinto R, Simel DL, Wijeysundera DN, Scales DC. Will This Patient Be Difficult to Intubate? JAMA. 2019;321:493-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 130] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 15. | Gottlieb M, Holladay D, Burns KM, Nakitende D, Bailitz J. Ultrasound for airway management: An evidence-based review for the emergency clinician. Am J Emerg Med. 2020;38:1007-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 16. | Falcetta S, Cavallo S, Gabbanelli V, Pelaia P, Sorbello M, Zdravkovic I, Donati A. Evaluation of two neck ultrasound measurements as predictors of difficult direct laryngoscopy: A prospective observational study. Eur J Anaesthesiol. 2018;35:605-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 17. | Binar M, Arslan F, Aydin U. Another cause of difficult airway in an elderly patient: Tongue-base abscess. Gerodontology. 2018;35:155-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Bruno MA, Drabek T, Manole MD. Difficult Intubation and Ventilation in an Infant With Retropharyngeal Abscess With Mediastinal Extension. Pediatr Emerg Care. 2019;35:e104-e106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Yoshimatsu Y, Morita R, Suginaka M, Furukawa K, Nakamura N, Yamairi K, Maruyama N, Kaji M, Kamimori T, Fujiwara H. Difficult intubation due to unknown congenital tracheal stenosis in the adult: a case report and literature review. J Thorac Dis. 2018;10:E93-E97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |