Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9318
Peer-review started: March 7, 2022
First decision: May 11, 2022
Revised: May 16, 2022
Accepted: August 5, 2022
Article in press: August 5, 2022
Published online: September 16, 2022
Processing time: 181 Days and 20.1 Hours
Ovarian anomalies except for uni- or bilateral streak gonads are rare. We present a rare case of an ovarian anomaly in which both ovaries were connected by extra tissue.
A 32-year-old, primipara with a twin pregnancy at 36 weeks of gestation was admitted to the hospital with severe preeclampsia. She underwent emergency cesarean section owing to persistent headache, blurred vision, and general edema. Following a peritoneal incision, a thin rectangular-shaped tissue was seen in front of the uterus. After delivery, the extra tissue was removed; no other anomalies were reported in either the ovaries or uterus. Pathology results of the removed tissue disclosed a well-vascularized loose stromal tissue with few follicles and scattered luteinized cells. In this case, to prevent pelvic adhesion or intestinal obstruction resulting from volvulus, strangulation, and torsion, the extra tissue was removed.
We report a case of a rare ovarian anomaly where both ovaries were connected by extra tissue. If the extra tissue extends to the abdominal cavity, it should be removed to prevent pelvic adhesion or abdominal complications including intestinal volvulus, strangulation, and torsion.
Core Tip: Herein we present the case of a rare ovarian anomaly where both ovaries were connected by extra tissue. If the extra tissue extends to the abdominal cavity, it should be removed to prevent pelvic adhesion or abdominal complications including intestinal volvulus, strangulation, and torsion.
- Citation: Choi MG, Kim JW, Kim YH, Kim AM, Kim TY, Ryu HK. Congenital ovarian anomaly manifesting as extra tissue connection between the two ovaries: A case report . World J Clin Cases 2022; 10(26): 9318-9322
- URL: https://www.wjgnet.com/2307-8960/full/v10/i26/9318.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i26.9318
Several ovarian anomalies have been reported. Among them is ovarian absence; in phenotypic females, the absence of both ovaries is generally linked to chromosome abnormalities and gonadal dysgenesis syndrome. In this case, individuals are likely to have streak gonads or underdeveloped gonads, which are a risk factor for malignancy[1]. Congenital unilateral ovarian agenesis in a normal female is extremely rare and asymptomatic in most cases. Ipsilateral renal or ureteric agenesis and/or ipsilateral malformation of the fallopian tube may be accompanied by congenital unilateral ovarian agenesis. The etiology of unilateral ovarian agenesis has yet to be explained. The two most likely causes of unilateral ovarian agenesis are an asymptomatic torsion of the ovary with consequent organ ischemia and reabsorption or a defect in the development of the Mullerian and gonadal structures underlying vascular anomalies[2]. Another example of ovarian anomalies is ectopic ovaries; whether accessory or supernumerary, ectopic ovaries are also extremely rare, 1 in 29000 to 1 in 70000 gynecologic admissions[3], and may be associated with other congenital genitourinary abnormalities[1]. An accessory ovary contains ovarian tissue and is usually connected to a normal ovary. In contrast, supernumerary ovaries are not attached to the ovary but may be found at various sites in or outside the pelvis. In this report, we present a rare case of an unreported anomaly in which both ovaries were connected by extra tissue.
A 32-year-old female presented with high blood pressure.
The primipara woman with a twin pregnancy at 36 weeks of gestation was admitted to the hospital with high blood pressure and proteinuria. Her blood pressure was 160/100 mmHg, while laboratory test results showed 3+ proteinuria. The pregnancy followed a successful in vitro fertilization-embryo transfer.
The patient had no history of past illness.
The patient had no specific history of genetic diseases.
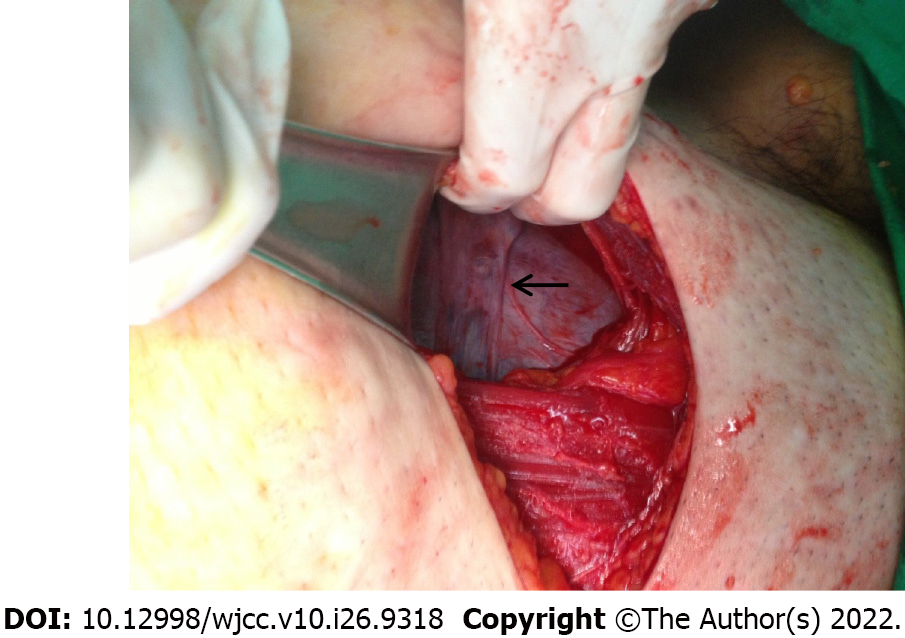
She underwent emergency caesarean section owing to persistent headache, blurred vision, and general edema. Following a peritoneal incision, a thin rectangular-shaped tissue was seen in front of the uterus (Figure 1); it formed a connection between the two ovaries (Figure 2). We displaced this tissue, incised the uterus, and delivered the fetuses.
There were no specific findings related to laboratory examinations.
There was no specific findings observed on imaging examinations.
Congenital ovarian anomaly manifesting as an extra tissue connection between the two ovaries.
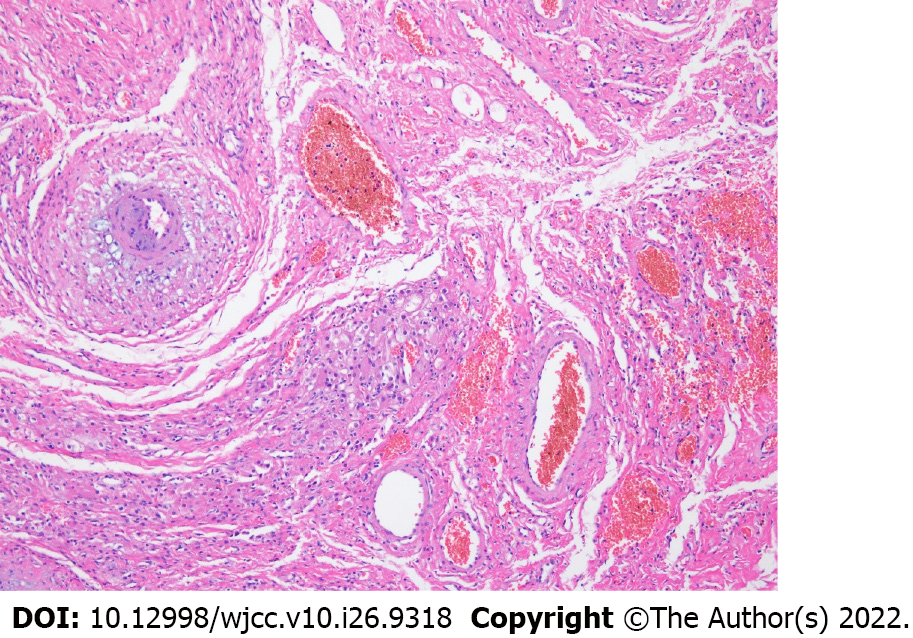
After delivery, we set the margins of both ovaries to avoid injuring the normal ovaries. First, both ends of the extra tissue were ligated and excised. Then the extra tissue was removed; no other abnormal findings were observed in both the ovaries and uterus. We explored the lower abdomen as much as possible to check for extra ovary tissues and any other malformations such as renal anomalies, but there were no specific findings. Pathology results of the removed tissue disclosed a well-vascularized loose stromal tissue with few follicles and scattered luteinized cells (Figure 3).
After surgery, the patient recovered and was discharged on the third postoperative day. During an outpatient follow-up after one month, the patient had no abdominal symptoms and ultrasonography revealed no abnormal findings on both adnexa.
Several studies have reported numerous cases of ovarian anomalies including bilateral and unilateral ovary absence, accessory, and supernumerary ovary. However, there are no reports on cases of connected ovaries, and to the best of our knowledge, this is the first case report. Our patient was admitted to the hospital with severe preeclampsia. She did not present other symptoms such as abdominal pain or pelvic pain and the pregnancy followed a successful in vitro fertilization-embryo transfer. She underwent an emergency caesarean section owing to severe headache, blurred vision, and general edema. A tissue connection between both ovaries was discovered by chance. In vitro fertilization is associated with several complications including ovarian hyperstimulation syndrome (characterized by swollen and painful ovaries), which results from the use of injectable fertility drugs, such as human chorionic gonadotropin (HCG)[4]. However, there seems to be no association between connected ovaries and ovulation induction complications. The extra tissue attached to an ovary may be asymptomatic and is not associated with infertility. In most cases, it may be left untreated with observation. However, as in the present case, if both ovaries are connected and a rectangular-shaped tissue lies in the abdominal cavity, this extra tissue can cause pelvic adhesion or intestinal volvulus, strangulation, and torsion resulting in intestinal obstruction[5]. Therefore, the extra tissue should be removed.
Herein we report the case of a rare ovarian anomaly where both ovaries were connected by extra tissue. In this case, to prevent pelvic adhesion or intestinal obstruction resulting from volvulus, strangulation, and torsion, the extra tissue was removed.
Provenance and peer review: Unsolicited article; Externally peer-reviewed.
Peer-review model: Single-blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Khaled I, Egypt; Naem AA, Syria; Yang YZ, China S-Editor: Ma YJ L-Editor: Webster JR P-Editor: Ma YJ
| 1. | Clement PB. Anatomy and histology of the ovary. In: Kurman RJ (ed) Blaustein’s pathology of the female genital tract. Springer. New York 2002; 649-674. Available from: https://link.springer.com/chapter/10.1007/978-1-4757-1942-0_15. |
| 2. | Dueck A, Poenaru D, Jamieson MA, Kamal IK. Unilateral ovarian agenesis and fallopian tube maldescent. Pediatr Surg Int. 2001;17:228-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Vendeland LL, Shehadeh L. Incidental finding of an accessory ovary in a 16-year-old at laparoscopy. A case report. J Reprod Med. 2000;45:435-438. [PubMed] |
| 4. | Mayo Clinic. In vitro fertilization(IVF). Published 2019. Available from: https://www.mayoclinic.org/tests-procedures/in-vitro-fertilization/about/pac-20384716. |
| 5. | Menzies D, Ellis H. Intestinal obstruction from adhesions--how big is the problem? Ann R Coll Surg Engl. 1990;72:60-63. [PubMed] |