Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9219
Peer-review started: April 6, 2022
First decision: June 11, 2022
Revised: June 26, 2022
Accepted: July 29, 2022
Article in press: July 29, 2022
Published online: September 16, 2022
Processing time: 148 Days and 18.4 Hours
This paper reviews the underlying evidence for various aspects of the conver
Core Tip: The therapeutic mechanism of mindfulness intervention in attention deficit hyperactivity disorder (ADHD) may be mainly via the convergence mechanism. Few studies have deeply explored the neurobiological mechanisms of mindfulness intervention in ADHD treatment. Differences in the efficacy of subtypes of mindfulness intervention, and corresponding specific imaging changes need further investigation. Pre- and post-treatment changes in regions of the executive control loop and default-mode network may be a key direction.
- Citation: Xu XP, Wang W, Wan S, Xiao CF. Convergence mechanism of mindfulness intervention in treating attention deficit hyperactivity disorder: Clues from current evidence. World J Clin Cases 2022; 10(26): 9219-9227
- URL: https://www.wjgnet.com/2307-8960/full/v10/i26/9219.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i26.9219
Attention deficit hyperactivity disorder (ADHD) is one of the most common developmental neuropsychiatric disorder characterized by attention deficit, hyperactivity, and impulsivity[1,2]. ADHD symptoms occur in a variety of contexts, severely affecting patients’ social function and development. Children and adolescents with ADHD often have other mental comorbidities, including autism spectrum disorder, tic disorder, obsessive-compulsive disorder, depressive disorder, and anxiety disorder[3,4]. Additionally, they are prone to various neurological problems, including headaches and epilepsy[5]. Currently, international recommendations for the combined use of medication and psychotherapy for children and adolescents vary[6-8]. Moreover, the nervous systems of children and adolescents are not fully developed, leading to significant differences across individuals and further complicating diagnosis and treatment[9]. Adult patients with ADHD often have adverse outcomes, including residual core symptoms/relapse, delayed recovery from multiple comorbidities, and impaired social function and reduced quality of life[10,11]. Currently, for adult ADHD patients, a comprehensive treatment plan based on central stimulants combined with psychotherapy is recommended[1,12].
ADHD is widely considered a neurodevelopmental disease and its pathogenesis has been associated with polygenic variation[13], subcortical abnormalities in the cerebral cortex[14], down/up-regulation of the brain-gut axis[15], and immunity[16]. However, reliable biomarkers or other objective criteria for diagnosing ADHD have not been identified[17], and the exact mechanisms of pathogenesis and mitigation have not been elucidated. ADHD is estimated to have a remission rate of 55%-85%, indicating that it persists to adulthood in < 50% of children and adolescents[18,19]. However, a recent 16-year longitudinal study showed that > 90% of children with ADHD in multimodal treatment studies may have residual symptoms in early adulthood, and that only 9.1% of the study’s participants achieved sustained remission[20]. These studies show that although ADHD treatment is effective in most cases, achieving intermittent remission periods, sustained remission is low. Thus, the mechanism by which various treatment modalities alleviate ADHD needs further investigation. Therefore, current research efforts seek to improve ADHD remission and explore neural targets for different treatments aimed at alleviating ADHD symptoms.
In the 21st century, neuroimaging technologies, such as electroencephalography, magnetic resonance imaging, and functional near-infrared spectroscopy, have advanced rapidly[21], offering valuable neuroimaging tools for studying the mechanisms of ADHD. In 2018, Sudre et al[22] summarized previous ADHD neuroimaging studies and suggested multiple cognitive developmental models that may elucidate the mechanisms of alleviating ADHD. Among them, the convergence mechanism may explain the results of most therapeutic interventions. The model hypothesizes that specific strategies can correct early irregularities in specific brain regions and promote the normalization of neural activation patterns from multiple dimensions, such as neuroanatomical structures and neural circuit function[23]. Remission may primarily be caused by the normalization of neural regions that control top-down cognitive processes, and it is likely that the neural characteristics of adult ADHD patients who achieve remission are not substantially different from those of healthy individuals[22]. This hypothesis is supported by multiple studies showing that regions like the right caudate nucleus may undergo gradual microarchitecture normalization after long-term stimulant treatment[14], and that remission in adult individuals is closely related to the convergence of brain activity patterns. Additionally, a recent randomized controlled trial (RCT) found that systematic right inferior frontal cortex (rIFC) functional magnetic resonance neurofeedback therapy has a positive effect on brain function in adolescent ADHD patients. This treatment upregulates rIFC function in the impaired cognitive control network and improves activation of the left frontal-insula-striatal and premotor regions, thereby improving symptoms[24,25].
Other models that may explain ADHD remission are the compensation/neural re-organization model, the fixed anomalies model, the carried forward model, and the cascading anomalies model, which have been partly confirmed by various studies, including neurophysiology and neuroimaging studies[17,26,27]. It is hypothesized that there is compatibility between multiple models and that different treatments may trigger different improvement processes[23]. Although recent studies have yielded more evidence in support of the convergence model, it has not been investigated in detail in the field of mindfulness intervention, and a comprehensive examination is warranted.
Although norepinephrine and dopamine reuptake inhibitors, such as methylphenidate, are effective in relieving the main symptoms of ADHD and play an important role in clinical treatment, benefit to some patients is limited by the following factors: (1) Contraindications[28-30]. Contraindications to methylphenidate include hyperthyroidism, pregnancy, hypertonia, and drug abuse[31]. If patients have such conditions, it is difficult to use psychopharmacological treatment; (2) Even without contraindications, the drug has low efficacy in many patients and about 20%-50% of adult ADHD patients may not respond to methylphenidate[28]. Data from multiple RCTs show that the therapeutic effect of central stimulants is often unsustainable and reduced dosage often causes rapid return of symptoms[32]; (3) Unacceptable side effects in some patients. Common side effects of central stimulants include headache, loss of appetite, weight loss, mouth dryness, palpitations, insomnia, gastrointestinal infections, and abnormally elevated blood pressure[33,34]; (4) Central stimulants such as methylphenidate often fail to improve patients’ comorbidities. ADHD patients often have a variety of mental disorders or emotional symptoms. Norepinephrine and dopamine reuptake inhibitors can only improve inherent attention deficit, impulsivity, and hyperactivity and in the presence of other drugs, complex drug interactions often make treatment difficult[35]. It is worth mentioning that viloxazine, which is also a norepi
Mindfulness intervention originated from Eastern Buddhism[42]. Mindfulness-based stress reduction (MBSR) programs for relieving chronic pain first emerged in 1979[43,44]. Since then, mindfulness intervention has undergone scientific development and developed into a systematic intervention strategy[42,45]. Mindfulness is often described as a conscious, non-judgmental awareness of internal and external experiences with two core elements: (1) Maintaining attention to the immediate experience; and (2) Maintaining a receptive attitude towards that experience[42,46]. This awareness can be developed through gradual exercise. Several modern subtypes of mindfulness interventions have been applied in clinical/non-clinical populations, including MBSR, mindfulness-based cognitive therapy (MBCT), dialectical behavior therapy (DBT), and acceptance and commitment therapy[38]. Mindfulness intervention was first introduced into the field of ADHD treatment in 2004[47]. During mindfulness intervention, ADHD patients perform breathing exercises and body relaxation exercises and gradually become aware of emotions in an open and accepting attitude, which helps them manage attention[48]. They may gain awareness and attention to everything that occurs at the moment and improve symptoms in executive function and emotional disorders[49]. Previous studies have shown that mindfulness may be used as a tool for reducing impairments in patients with residual ADHD symptoms[50]. Mindfulness is regarded as the third wave of ADHD psychological theory, and it differs from traditional CBT, which not only explores the content of the relationship between thought and emotion, but also the relationship’s context[51]. In addition to alleviating symptoms, mindfulness intervention contains a more holistic health perspective and is feasible, efficacious, and safe, as shown by numerous clinical trials and meta-analyses[38]. Mindfulness intervention strategies for ADHD mainly include MBCT, DBT, and other non-specific mindfulness interventions[51], such as mindfulness meditation-based mobile applications[49].
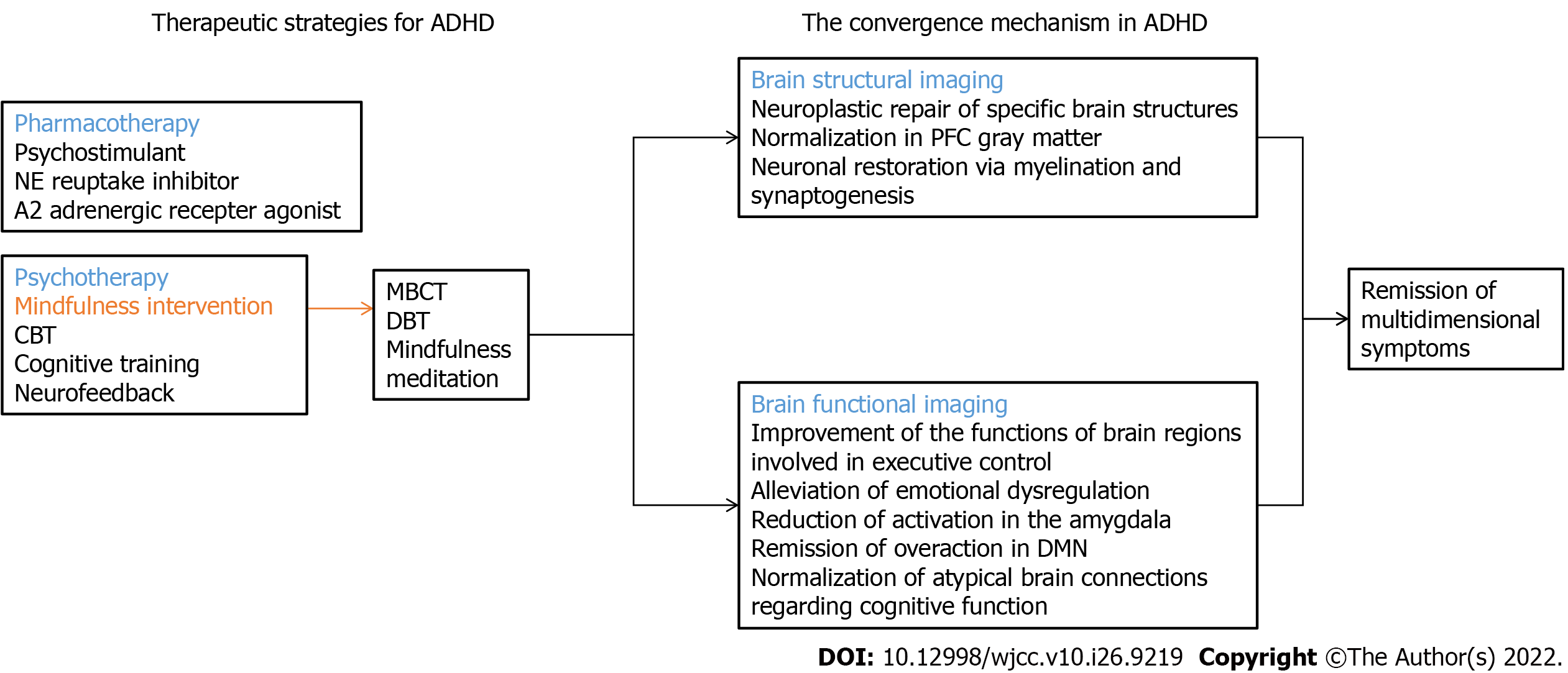
Although the clinical efficacy of mindfulness intervention has been extensively confirmed[52,53], there is still no unified consensus on the process of ADHD remission[54]. Understanding this process is key to the elucidation of the neurobiological mechanisms underlying ADHD remission/sustainability and may unveil candidate biomarkers for the development of more therapeutic subtypes of mindfulness intervention. For the moment, despite a number of clinical trials on the efficacy and safety of treatments for ADHD core symptoms[6], and that the underlying mechanism of pharmacological interventions is relatively fully elucidated, evidence synthesizing the imaging characteristics of the non-pharmacological interventions by means of fMRI is still limited[12]. Hence we keep our thought fastened on the mindfulness intervention in ADHD, so as to acquire a thorough comprehension of the convergence mechanism. Since the monitoring of imaging changes via fMRI, meanwhile, does not contain a sufficient number of studies that conformed to strict criteria of systematic review and meta-analysis, we ultimately choose the format of selective review. We searched for the terms ((mindfulness intervention) OR (mindfulness)) AND (ADHD) within the title/abstract of the relevant literature from the PubMed and Web of Science database on March 15, 2022. We also searched Google Scholar for additional articles that may have been missed on the initial search to control for publication bias. In total, 179 papers were retrieved (46 from PubMed, 131 from Web of Science, and 2 from Google Scholar). After checking out repetitions and themes, only 21 papers were perfectly appropriate in which explicit studies monitoring imaging changes associated with mindfulness interventions in ADHD were implemented or supporting evidence of mindfulness intervention in brain imaging was expounded. We speculate that mindfulness intervention in ADHD treatment may primarily work through the convergence mechanism. Mindfulness intervention may lead to a clinical course of symptom relief, which is mediated by the restoration of the neural network with specific deficits (as shown in Figure 1).
Neuroanatomical abnormalities in ADHD may be revealed by changes in total brain volume and cortical and subcortical multidimensional structural changes[14,23,55]. A recent large cohort study found that significant gray matter loss in adolescent ADHD patients is significantly associated with impaired concentration or working memory[18]. In particular, persistent reduction in the volume of the prefrontal cortex (PFC) may be an imaging feature that correlates with the persistence of symptoms into adulthood[56]. MBCT combines cognitive behavioral therapy and mindfulness meditation using top-down cognitive control and mental training of mindfulness meditation[57,58]. These may cause the neuroplastic repair of specific brain structures[59,60], thereby improving various aspects, including attention control and emotion regulation[41,61]. A meta-analysis of 21 studies involving mindfulness intervention found that mindfulness induces persistent structural changes in eight brain regions, including increases in PFC gray matter density and thickness[62]. These interesting findings shed light on the potential normalizing process of mindfulness intervention, which may enhance self-awareness in patients by restoring damaged regional structures such as the PFC. Although various mindfulness-based structural neuroimaging studies have shown that mindfulness intervention that mediates multiple complex aspects of mental function may involve large-scale modulation of brain network structure[63], evidence is lacking on the mechanisms by which mindfulness intervention affects brain structure in ADHD patients. It is thought that mindfulness meditation alters patients’ brain structure via myelination and synaptogenesis[63], and that it may positively impact neuronal preservation and restoration[64,65].
Fronto-basal ganglia network includes the rIFC, anterior cingulate cortex (ACC), anterior PFC, dorsolateral PFC (dlPFC), inferior parietal lobe, and striatum[66]. The network combines external information with internal representations, providing the flexibility of processing information with changing task requirements, ultimately contributing to goal-directed execution[67]. Its low activation may significantly contribute to executive dysfunction in adult ADHD patients[68]. After a 6-wk mindfulness intervention in healthy people, participants showed increased dlPFC activation on the emotional Stroop task[69]. Experienced mindfulness meditators also showed better ACC brain activity during meditation[70]. Studies of integrative body-mind training intervention in student populations have shown that in resting state after meditation, the activation of the ventral and/or rostral ACC, caudatum, and putamen was enhanced[64]. Combined with the above studies, we speculate that mindfulness intervention is likely to up-regulate the functions of brain regions involved in executive control and this activation not only benefits the normal population, but also increases function in ADHD patients. Frontal-striatal circuitry and other damaged brain regions gradually enhance original functions and approach normal levels. Studies have also shown that in a mindful state that only observes breathing, the activation of brain regions such as the striatum is enhanced and that this effect is consistent with the psychopharmacological treatment with stimulant drugs like methylphenidate. In this region, defects in dopaminergic and noradrenergic systems are alleviated, which improves the function of the corresponding brain region[71]. In children and adolescents with ADHD, weaker brain activation in the PFC and striatum is also believed to predict impaired inhibitory behavior and individual functioning of sustained attention[72]. Additionally, treatment of anxiety disorder patients with MBSR also revealed that the ventrolateral PFC response that had been reduced in the process of performing specific tasks was partially restored[73]. This observation also suggests that the convergence mechanism might play a major role.
Emotional dysregulation is thought to be an important comorbidity of ADHD, and there may be a singular neurobiological pathway of pathogenesis during the process[14]. Emotion regulation refers to strategies that influence the occurrence, experience, and expression of emotions[74]. Practitioners in mindfulness intervention are advised, as much as possible, not to act out their emotional states, but to treat them as passing events[42]. It is believed that in ADHD patients, emotional dysregulation may be alleviated by improved brain function in the area that caused the original defect[63]. For example, mindfulness meditation can improve affective responding through reduced amygdala reactivity, which may reduce abnormal emotional arousal in children with ADHD[75-77].
Default-mode network (DMN) includes the medial PFC (mPFC), ACC, and posterior cingulate cortex (PCC) and its dysfunction may be a key cause of ADHD. In healthy people, DMN activity is usually suppressed during the execution of tasks that require external attention and the more attention required, the less DMN activated[78]. In ADHD patients, the DMN network is overactive during task performance, which may disrupt cognitive performance and cause attention fluctuations[41]. Good mindfulness meditation may decrease brain activation in the DMN, thereby minimizing mind wandering. A study comparing experienced mindfulness meditators and healthy non-meditators found that during mindfulness meditation, DMN activation was relatively reduced, especially the main nodes mPFC and PCC, which were relatively inactivated[79].
In ADHD, an imbalance between neural excitation and inhibition may occur in early childhood development, which may lead to atypical brain connections within and between neural networks associated with cognitive function, leading to long-term persistence of symptoms[17]. Previous EEG studies of mindfulness indicated that in addition to mediating the normalization of brain function, it also promotes the normalization of damaged connections, which may also be a key mechanism by which mindfulness intervention promotes ADHD remission[80]. It is thought that mindfulness intervention might improve functional connectivity of the PFC, which may also be closely related to the normalization of neural regions that control top-down cognitive processes[42]. At the same time, there may also be atypical connectivity in the limbic cortex-striatal-thalamo-cortical loops in ADHD patients, suggesting that impaired affective motivational systems may underlie the neural basis of ADHD[14]. Mindfulness practice can reduce brain functional connectivity between the amygdala and the ACC, which are involved in the regulation of “fight or flight” stress responses, thereby inhibiting abnormal impulses[42]. Additionally, the persistence of ADHD symptoms into adulthood may be associated with reduced dynamic functional connectivity of the DMN to functional brain networks during active tasks[81]. A study on DMN functional connectivity in subjects during attention concentration meditation/ loving-kindness meditation/choiceless awareness meditation, found stronger functional connectivity between the PCC, dACC, and dlPFC in experienced subjects in these non-specific mindfulness meditations, which may lead to a reduction in attentional errors in cognitive measures[79]. This also provides indirect evidence that mindfulness intervention in ADHD may gradually restore impaired DMN external functional connectivity.
This article summarizes the underlying evidence for various aspects of convergence mechanism of mindfulness intervention for ADHD. Although evidence has accumulated on the convergence mechanism, its role in ADHD remission is not conclusively established. There may be compatibility among various ADHD remission models and the therapeutic mechanism of mindfulness intervention in ADHD may be mainly via the convergence mechanism, which may restore brain microstructure and functional networks.
Several limitations in current research are worth mentioning: (1) Discussions on mindfulness intervention in ADHD treatment are still focused on clinical indexes, such as its therapeutic effect[82], which has been adequately shown to be effective, accessible, and safe[7]. However, few studies have deeply explored the underlying neurobiological mechanisms[83]. In particular, neuroimaging-based analysis of the mechanisms of mindfulness intervention is lacking and there has been no major breakthrough in recent years; and (2) Mindfulness intervention emphasizes understanding the core; that is, different subtypes focus on training learners to grasp the psychological characteristics of more mindfulness, acceptance, and awareness. However, the common mechanisms corresponding to this feature at the neuroimaging level are still poorly understood. In contrast, differences in the efficacy of various subtypes of mindfulness intervention, and corresponding specific imaging changes need further investigation. With the development of brain imaging techniques of mindfulness in ADHD, we next plan to conduct a systematic review and meta-analysis based on sufficient independent primary studies where validated date or statistical information is available for generating an appropriate calculation of the imaging changes. Future research may focus on the neuroimaging features of specific mindfulness intervention subtypes as a key direction, especially focusing on pre- and post-treatment changes in key regions of the executive control loop and DMN. This may further elucidate the convergence mechanism and clarify the specific effects of neuropsychological techniques on associated brain regions and reliable imaging indicators, as well as identify clearer treatment objectives for personalized clinical care.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Byeon H, South Korea; Patel R, United States; Stoyanov D, Bulgaria S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Austerman J. ADHD and behavioral disorders: Assessment, management, and an update from DSM-5. Cleve Clin J Med. 2015;82:S2-S7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 2. | Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, Olesen J, Allgulander C, Alonso J, Faravelli C, Fratiglioni L, Jennum P, Lieb R, Maercker A, van Os J, Preisig M, Salvador-Carulla L, Simon R, Steinhausen HC. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:655-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2482] [Cited by in RCA: 2351] [Article Influence: 167.9] [Reference Citation Analysis (0)] |
| 3. | Reale L, Bartoli B, Cartabia M, Zanetti M, Costantino MA, Canevini MP, Termine C, Bonati M; Lombardy ADHD Group. Comorbidity prevalence and treatment outcome in children and adolescents with ADHD. Eur Child Adolesc Psychiatry. 2017;26:1443-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 228] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 4. | Farhat LC, Brentani H, de Toledo VHC, Shephard E, Mattos P, Baron-Cohen S, Thapar A, Casella E, Polanczyk GV. ADHD and autism symptoms in youth: a network analysis. J Child Psychol Psychiatry. 2022;63:143-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 5. | Pan PY, Bölte S. The association between ADHD and physical health: a co-twin control study. Sci Rep. 2020;10:22388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Caye A, Swanson JM, Coghill D, Rohde LA. Treatment strategies for ADHD: an evidence-based guide to select optimal treatment. Mol Psychiatry. 2019;24:390-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 161] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 7. | Correll CU, Cortese S, Croatto G, Monaco F, Krinitski D, Arrondo G, Ostinelli EG, Zangani C, Fornaro M, Estradé A, FUnited Statesr-Poli P, Carvalho AF, Solmi M. Efficacy and acceptability of pharmacological, psychosocial, and brain stimulation interventions in children and adolescents with mental disorders: an umbrella review. World Psychiatry. 2021;20:244-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 84] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 8. | Padilha SCOS, Virtuoso S, Tonin FS, Borba HHL, Pontarolo R. Efficacy and safety of drugs for attention deficit hyperactivity disorder in children and adolescents: a network meta-analysis. Eur Child Adolesc Psychiatry. 2018;27:1335-1345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Young JL, Goodman DW. Adult Attention-Deficit/Hyperactivity Disorder Diagnosis, Management, and Treatment in the DSM-5 Era. Prim Care Companion CNS Disord. 2016;18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Magnin E, Maurs C. Attention-deficit/hyperactivity disorder during adulthood. Rev Neurol (Paris). 2017;173:506-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Adler LA, Solanto M, Escobar R, Lipsius S, Upadhyaya H. Executive Functioning Outcomes Over 6 Months of Atomoxetine for Adults With ADHD: Relationship to Maintenance of Response and Relapse Over the Subsequent 6 Months After Treatment. J Atten Disord. 2020;24:363-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 12. | De Crescenzo F, Cortese S, Adamo N, Janiri L. Pharmacological and non-pharmacological treatment of adults with ADHD: a meta-review. Evid Based Ment Health. 2017;20:4-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 92] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 13. | Geller DA, Homayoun S, Johnson G. Developmental Considerations in Obsessive Compulsive Disorder: Comparing Pediatric and Adult-Onset Cases. Front Psychiatry. 2021;12:678538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 14. | Drechsler R, Brem S, Brandeis D, Grünblatt E, Berger G, Walitza S. ADHD: Current Concepts and Treatments in Children and Adolescents. Neuropediatrics. 2020;51:315-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 149] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 15. | Dam SA, Mostert JC, Szopinska-Tokov JW, Bloemendaal M, Amato M, Arias-Vasquez A. The Role of the Gut-Brain Axis in Attention-Deficit/Hyperactivity Disorder. Gastroenterol Clin North Am. 2019;48:407-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 16. | Hoekstra PJ. Attention-deficit/hyperactivity disorder: is there a connection with the immune system? Eur Child Adolesc Psychiatry. 2019;28:601-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Mamiya PC, Arnett AB, Stein MA. Precision Medicine Care in ADHD: The Case for Neural Excitation and Inhibition. Brain Sci. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 18. | Duan K, Jiang W, Rootes-Murdy K, Schoenmacker GH, Arias-Vasquez A, Buitelaar JK, Hoogman M, Oosterlaan J, Hoekstra PJ, Heslenfeld DJ, Hartman CA, Calhoun VD, Turner JA, Liu J. Gray matter networks associated with attention and working memory deficit in ADHD across adolescence and adulthood. Transl Psychiatry. 2021;11:184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Szejko N, Jakubczyk A, Janik P. Prevalence and Clinical Correlates of Self-Harm Behaviors in Gilles de la Tourette Syndrome. Front Psychiatry. 2019;10:638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Sibley MH, Arnold LE, Swanson JM, Hechtman LT, Kennedy TM, Owens E, Molina BSG, Jensen PS, Hinshaw SP, Roy A, Chronis-Tuscano A, Newcorn JH, Rohde LA; MTA Cooperative Group. Variable Patterns of Remission From ADHD in the Multimodal Treatment Study of ADHD. Am J Psychiatry. 2022;179:142-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 163] [Article Influence: 54.3] [Reference Citation Analysis (0)] |
| 21. | Mu, Y. , C. Cerritos, and F. Khan, Neural mechanisms underlying interpersonal coordination: A review of hyperscanning research. Social and Personality Psychology Compass. 2018;12:e12421. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Sudre G, Mangalmurti A, Shaw P. Growing out of attention deficit hyperactivity disorder: Insights from the 'remitted' brain. Neurosci Biobehav Rev. 2018;94:198-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 23. | Shaw P, Sudre G. Adolescent Attention-Deficit/Hyperactivity Disorder: Understanding Teenage Symptom Trajectories. Biol Psychiatry. 2021;89:152-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 24. | Criaud M, Wulff M, Alegria AA, Barker GJ, Giampietro V, Rubia K. Increased left inferior fronto-striatal activation during error monitoring after fMRI neurofeedback of right inferior frontal cortex in adolescents with attention deficit hyperactivity disorder. Neuroimage Clin. 2020;27:102311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Lam SL, Criaud M, Alegria A, Barker GJ, Giampietro V, Rubia K. Neurofunctional and behavioural measures associated with fMRI-neurofeedback learning in adolescents with Attention-Deficit/Hyperactivity Disorder. Neuroimage Clin. 2020;27:102291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 26. | Zhao X, Li H, Wang E, Luo X, Han C, Cao Q, Liu L, Chen J, Wang C, Johnstone SJ, Wang Y, Sun L. Neural Correlates of Working Memory Deficits in Different Adult Outcomes of ADHD: An Event-Related Potential Study. Front Psychiatry. 2020;11:348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Michelini G, Jurgiel J, Bakolis I, Cheung CHM, Asherson P, Loo SK, Kuntsi J, Mohammad-Rezazadeh I. Atypical functional connectivity in adolescents and adults with persistent and remitted ADHD during a cognitive control task. Transl Psychiatry. 2019;9:137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 28. | Wilens TE, Spencer TJ, Biederman J. A review of the pharmacotherapy of adults with attention-deficit/hyperactivity disorder. J Atten Disord. 2002;5:189-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 100] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 29. | Lamb YN. Viloxazine: Pediatric First Approval. Paediatr Drugs. 2021;23:403-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 30. | Lambez B, Harwood-Gross A, Golumbic EZ, Rassovsky Y. Non-pharmacological interventions for cognitive difficulties in ADHD: A systematic review and meta-analysis. J Psychiatr Res. 2020;120:40-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 98] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 31. | Eich D, Seifritz E, Eich P. Pharmakotherapie bei ADHS im Erwachsenenalter: Eine Bestandsaufnahme. Zeitschrift für Psychiatrie, Psychologie und Psychotherapie. 2015;63:15-24. [DOI] [Full Text] |
| 32. | Tamminga HGH, Reneman L, Schrantee A, Bottelier MA, Bouziane C, Geurts HM, Groenman AP. Do effects of methylphenidate on cognitive performance last beyond treatment? Eur Neuropsychopharmacol. 2021;46:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 33. | Cândido RCF, Menezes de Padua CA, Golder S, Junqueira DR. Immediate-release methylphenidate for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev. 2021;1:CD013011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 34. | Jaeschke RR, Sujkowska E, Sowa-Kućma M. Methylphenidate for attention-deficit/hyperactivity disorder in adults: a narrative review. Psychopharmacology (Berl). 2021;238:2667-2691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 35. | Weibel S, Menard O, Ionita A, Boumendjel M, Cabelguen C, Kraemer C, Micoulaud-Franchi JA, Bioulac S, Perroud N, Sauvaget A, Carton L, Gachet M, Lopez R. Practical considerations for the evaluation and management of Attention Deficit Hyperactivity Disorder (ADHD) in adults. Encephale. 2020;46:30-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 36. | Findling RL, Candler SA, Nasser AF, Schwabe S, Yu C, Garcia-Olivares J, O'Neal W, Newcorn JH. Viloxazine in the Management of CNS Disorders: A Historical Overview and Current Status. CNS Drugs. 2021;35:643-653. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 37. | Yu C, Garcia-Olivares J, Candler S, Schwabe S, Maletic V. New Insights into the Mechanism of Action of Viloxazine: Serotonin and Norepinephrine Modulating Properties. J Exp Pharmacol. 2020;12:285-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 38. | Cairncross M, Miller CJ. The Effectiveness of Mindfulness-Based Therapies for ADHD: A Meta-Analytic Review. J Atten Disord. 2020;24:627-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 98] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 39. | Muris P, Roodenrijs D, Kelgtermans L, Sliwinski S, Berlage U, Baillieux H, Deckers A, Gunther M, Paanakker B, Holterman I. No Medication for My Child! Child Psychiatry Hum Dev. 2018;49:974-992. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 40. | Young S, Amarasinghe JM. Practitioner review: Non-pharmacological treatments for ADHD: a lifespan approach. J Child Psychol Psychiatry. 2010;51:116-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 112] [Article Influence: 7.5] [Reference Citation Analysis (1)] |
| 41. | Bachmann K, Lam AP, Philipsen A. Mindfulness-Based Cognitive Therapy and the Adult ADHD Brain: A Neuropsychotherapeutic Perspective. Front Psychiatry. 2016;7:117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 42. | Creswell JD. Mindfulness Interventions. Annu Rev Psychol. 2017;68:491-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 542] [Cited by in RCA: 638] [Article Influence: 70.9] [Reference Citation Analysis (0)] |
| 43. | Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KM. Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther. 2016;45:5-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 582] [Cited by in RCA: 441] [Article Influence: 49.0] [Reference Citation Analysis (0)] |
| 44. | Niazi AK, Niazi SK. Mindfulness-based stress reduction: a non-pharmacological approach for chronic illnesses. N Am J Med Sci. 2011;3:20-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 45. | Lin J, Chadi N, Shrier L. Mindfulness-based interventions for adolescent health. Curr Opin Pediatr. 2019;31:469-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 46. | Hofmann SG, Gómez AF. Mindfulness-Based Interventions for Anxiety and Depression. Psychiatr Clin North Am. 2017;40:739-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 311] [Article Influence: 38.9] [Reference Citation Analysis (0)] |
| 47. | Hayes SC. Acceptance and Commitment Therapy, Relational Frame Theory, and the Third Wave of Behavioral and Cognitive Therapies - Republished Article. Behav Ther. 2016;47:869-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 420] [Article Influence: 46.7] [Reference Citation Analysis (0)] |
| 48. | Zylowska L, Ackerman DL, Yang MH, Futrell JL, Horton NL, Hale TS, Pataki C, Smalley SL. Mindfulness meditation training in adults and adolescents with ADHD: a feasibility study. J Atten Disord. 2008;11:737-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 290] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 49. | Bigelow H, Gottlieb MD, Ogrodnik M, Graham JD, Fenesi B. The Differential Impact of Acute Exercise and Mindfulness Meditation on Executive Functioning and Psycho-Emotional Well-Being in Children and Youth With ADHD. Front Psychol. 2021;12:660845. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 50. | Modesto-Lowe V, Farahmand P, Chaplin M, Sarro L. Does mindfulness meditation improve attention in attention deficit hyperactivity disorder? World J Psychiatry. 2015;5:397-403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (3)] |
| 51. | Champ RE, Adamou M, Tolchard B. The impact of psychological theory on the treatment of Attention Deficit Hyperactivity Disorder (ADHD) in adults: A scoping review. PLoS One. 2021;16:e0261247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 52. | Schmiedeler S. [Mindfulness-based intervention in attention-deficit-/hyperactivity disorder (ADHD)]. Z Kinder Jugendpsychiatr Psychother. 2015;43:123-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 53. | Xue J, Zhang Y, Huang Y. A meta-analytic investigation of the impact of mindfulness-based interventions on ADHD symptoms. Medicine (Baltimore). 2019;98:e15957. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 54. | Alsubaie M, Abbott R, Dunn B, Dickens C, Keil TF, Henley W, Kuyken W. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: A systematic review. Clin Psychol Rev. 2017;55:74-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 191] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 55. | Saad JF, Griffiths KR, Kohn MR, Clarke S, Williams LM, Korgaonkar MS. Regional brain network organization distinguishes the combined and inattentive subtypes of Attention Deficit Hyperactivity Disorder. Neuroimage Clin. 2017;15:383-390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 56. | Valera EM, Faraone SV, Murray KE, Seidman LJ. Meta-analysis of structural imaging findings in attention-deficit/hyperactivity disorder. Biol Psychiatry. 2007;61:1361-1369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 591] [Cited by in RCA: 573] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 57. | Auclair V, Harvey PO, Lepage M. [Cognitive Behavioral Therapy and the Treatment of ADHD in Adults]. Sante Ment Que. 41:291-311. [PubMed] |
| 58. | Hepark S, Janssen L, de Vries A, Schoenberg PLA, Donders R, Kan CC, Speckens AEM. The Efficacy of Adapted MBCT on Core Symptoms and Executive Functioning in Adults With ADHD: A Preliminary Randomized Controlled Trial. J Atten Disord. 2019;23:351-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 59. | McEwen BS. In pursuit of resilience: stress, epigenetics, and brain plasticity. Ann N Y Acad Sci. 2016;1373:56-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 186] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 60. | Williams JM, Teasdale JD, Segal ZV, Soulsby J. Mindfulness-based cognitive therapy reduces overgeneral autobiographical memory in formerly depressed patients. J Abnorm Psychol. 2000;109:150-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 61. | Bajaj B, Khoury B, Sengupta S. Resilience and Stress as Mediators in the Relationship of Mindfulness and Happiness. Front Psychol. 2022;13:771263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 62. | Fox KC, Nijeboer S, Dixon ML, Floman JL, Ellamil M, Rumak SP, Sedlmeier P, Christoff K. Is meditation associated with altered brain structure? Neurosci Biobehav Rev. 2014;43:48-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 591] [Cited by in RCA: 406] [Article Influence: 36.9] [Reference Citation Analysis (0)] |
| 63. | Tang YY, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015;16:213-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1175] [Cited by in RCA: 1219] [Article Influence: 121.9] [Reference Citation Analysis (0)] |
| 64. | Tang YY, Ma Y, Fan Y, Feng H, Wang J, Feng S, Lu Q, Hu B, Lin Y, Li J, Zhang Y, Wang Y, Zhou L, Fan M. Central and autonomic nervous system interaction is altered by short-term meditation. Proc Natl Acad Sci U S A. 2009;106:8865-8870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 436] [Cited by in RCA: 377] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 65. | Wielgosz J, Goldberg SB, Kral TRA, Dunne JD, Davidson RJ. Mindfulness Meditation and Psychopathology. Annu Rev Clin Psychol. 2019;15:285-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 182] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 66. | Dickstein SG, Bannon K, Castellanos FX, Milham MP. The neural correlates of attention deficit hyperactivity disorder: an ALE meta-analysis. J Child Psychol Psychiatry. 2006;47:1051-1062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 508] [Cited by in RCA: 492] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 67. | Castellanos FX, Proal E. Large-scale brain systems in ADHD: beyond the prefrontal-striatal model. Trends Cogn Sci. 2012;16:17-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 459] [Cited by in RCA: 493] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 68. | Cortese S, Kelly C, Chabernaud C, Proal E, Di Martino A, Milham MP, Castellanos FX. Toward systems neuroscience of ADHD: a meta-analysis of 55 fMRI studies. Am J Psychiatry. 2012;169:1038-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 645] [Cited by in RCA: 700] [Article Influence: 53.8] [Reference Citation Analysis (0)] |
| 69. | Allen M, Dietz M, Blair KS, van Beek M, Rees G, Vestergaard-Poulsen P, Lutz A, Roepstorff A. Cognitive-affective neural plasticity following active-controlled mindfulness intervention. J Neurosci. 2012;32:15601-15610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 217] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 70. | Hölzel BK, Ott U, Hempel H, Hackl A, Wolf K, Stark R, Vaitl D. Differential engagement of anterior cingulate and adjacent medial frontal cortex in adept meditators and non-meditators. Neurosci Lett. 2007;421:16-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 307] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 71. | Del Campo N, Chamberlain SR, Sahakian BJ, Robbins TW. The roles of dopamine and noradrenaline in the pathophysiology and treatment of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2011;69:e145-e157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 448] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 72. | Donsky A. Taking Charge of ADHD: The Complete Authoritative Guide for Parents. Revised Edition. The Canadian child and adolescent psychiatry review. 2003;12:124-124. |
| 73. | Hölzel BK, Hoge EA, Greve DN, Gard T, Creswell JD, Brown KW, Barrett LF, Schwartz C, Vaitl D, Lazar SW. Neural mechanisms of symptom improvements in generalized anxiety disorder following mindfulness training. Neuroimage Clin. 2013;2:448-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 172] [Cited by in RCA: 176] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 74. | Shaw P, Stringaris A, Nigg J, Leibenluft E. Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry. 2014;171:276-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 605] [Cited by in RCA: 699] [Article Influence: 63.5] [Reference Citation Analysis (0)] |
| 75. | Kral TRA, Schuyler BS, Mumford JA, Rosenkranz MA, Lutz A, Davidson RJ. Impact of short- and long-term mindfulness meditation training on amygdala reactivity to emotional stimuli. Neuroimage. 2018;181:301-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 136] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 76. | Ngô TL. [Review of the effects of mindfulness meditation on mental and physical health and its mechanisms of action]. Sante Ment Que. 2013;38:19-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 77. | Lutz J, Herwig U, Opialla S, Hittmeyer A, Jäncke L, Rufer M, Grosse Holtforth M, Brühl AB. Mindfulness and emotion regulation--an fMRI study. Soc Cogn Affect Neurosci. 2014;9:776-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 174] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 78. | Buckner RL, Andrews-Hanna JR, Schacter DL. The brain's default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci. 2008;1124:1-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6342] [Cited by in RCA: 6984] [Article Influence: 410.8] [Reference Citation Analysis (0)] |
| 79. | Brewer JA, Worhunsky PD, Gray JR, Tang YY, Weber J, Kober H. Meditation experience is associated with differences in default mode network activity and connectivity. Proc Natl Acad Sci U S A. 2011;108:20254-20259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 794] [Cited by in RCA: 698] [Article Influence: 49.9] [Reference Citation Analysis (0)] |
| 80. | Tang YY, Tang R, Rothbart MK, Posner MI. Frontal theta activity and white matter plasticity following mindfulness meditation. Curr Opin Psychol. 2019;28:294-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 81. | Shappell HM, Duffy KA, Rosch KS, Pekar JJ, Mostofsky SH, Lindquist MA, Cohen JR. Children with attention-deficit/hyperactivity disorder spend more time in hyperconnected network states and less time in segregated network states as revealed by dynamic connectivity analysis. Neuroimage. 2021;229:117753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 82. | Fu D, Wu DD, Guo HL, Hu YH, Xia Y, Ji X, Fang WR, Li YM, Xu J, Chen F, Liu QQ. The Mechanism, Clinical Efficacy, Safety, and Dosage Regimen of Atomoxetine for ADHD Therapy in Children: A Narrative Review. Front Psychiatry. 2021;12:780921. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 83. | Xi T, Wu J. A Review on the Mechanism Between Different Factors and the Occurrence of Autism and ADHD. Psychol Res Behav Manag. 2021;14:393-403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |