Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.9096
Peer-review started: April 3, 2022
First decision: May 30, 2022
Revised: June 7, 2022
Accepted: July 29, 2022
Article in press: July 29, 2022
Published online: September 6, 2022
Processing time: 144 Days and 23.5 Hours
Venous hemangioma is a benign and non-invasive type of tumor, which is rarely identified due to the absence of clinical manifestations. A retroperitoneal benign tumor is comparatively rare, and hemangioma is exceptional. Because of the different types and locations of hemangioma, presentations are varied; thus, establishing an accurate diagnosis before surgery is challenging.
A 45-year-old female patient visited our hospital with the complaint of a retroperitoneal mass without symptoms discovered during a medical exami
Venous hemangioma is rare in adults, and an accurate diagnosis before surgery is challenging. Surgery is the curative treatment for venous hemangioma, and the definitive diagnosis relies on pathology.
Core Tip: Venous hemangioma is a benign disease which is rarely reported as it lacks clinical manifestations. However, many cases have presented with abdominal symptoms. An accurate diagnosis before surgery is challenging due to non-specific manifestations and low incidence. Surgery is the first-line treatment for venous hemangioma, and the definitive diagnosis depends on pathology.
- Citation: Qin Y, Qiao P, Guan X, Zeng S, Hu XP, Wang B. Successful resection of a huge retroperitoneal venous hemangioma: A case report. World J Clin Cases 2022; 10(25): 9096-9103
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/9096.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.9096
Venous hemangioma is defined as a benign tumor consisting of vein-like vessels, and is a rare but clinically significant disease. The lesion may occur in various sites but is rarely found in the retroperitoneum[1,2]. Retroperitoneal hemangioma is extremely rare and accounts for less than 5% of all retroperitoneal tumors in adults[3]. Data indicate that abdominal distension and pain are the two most common manifestations. To the best of our knowledge, only a few isolated cases have been reported. Due to the different locations and varied manifestations of venous hemangioma, establishing an accurate diagnosis before surgery is challenging. We here report a case of giant venous hemangioma in the retroperitoneum and review the literature concerning the clinical and pathological features of this disease.
A 45-year-old female patient visited our hospital with the complaint of a retroperitoneal mass without symptoms discovered during a medical examination.
The patient was found to have a retroperitoneal mass during a physical examination at another hospital 5 mo previously, and ultrasonography revealed a large anechoic mass that occupied almost all of the right side of the peritoneal cavity.
A physical examination revealed no mass and tenderness in the abdomen.
Laboratory tests showed no abnormalities.
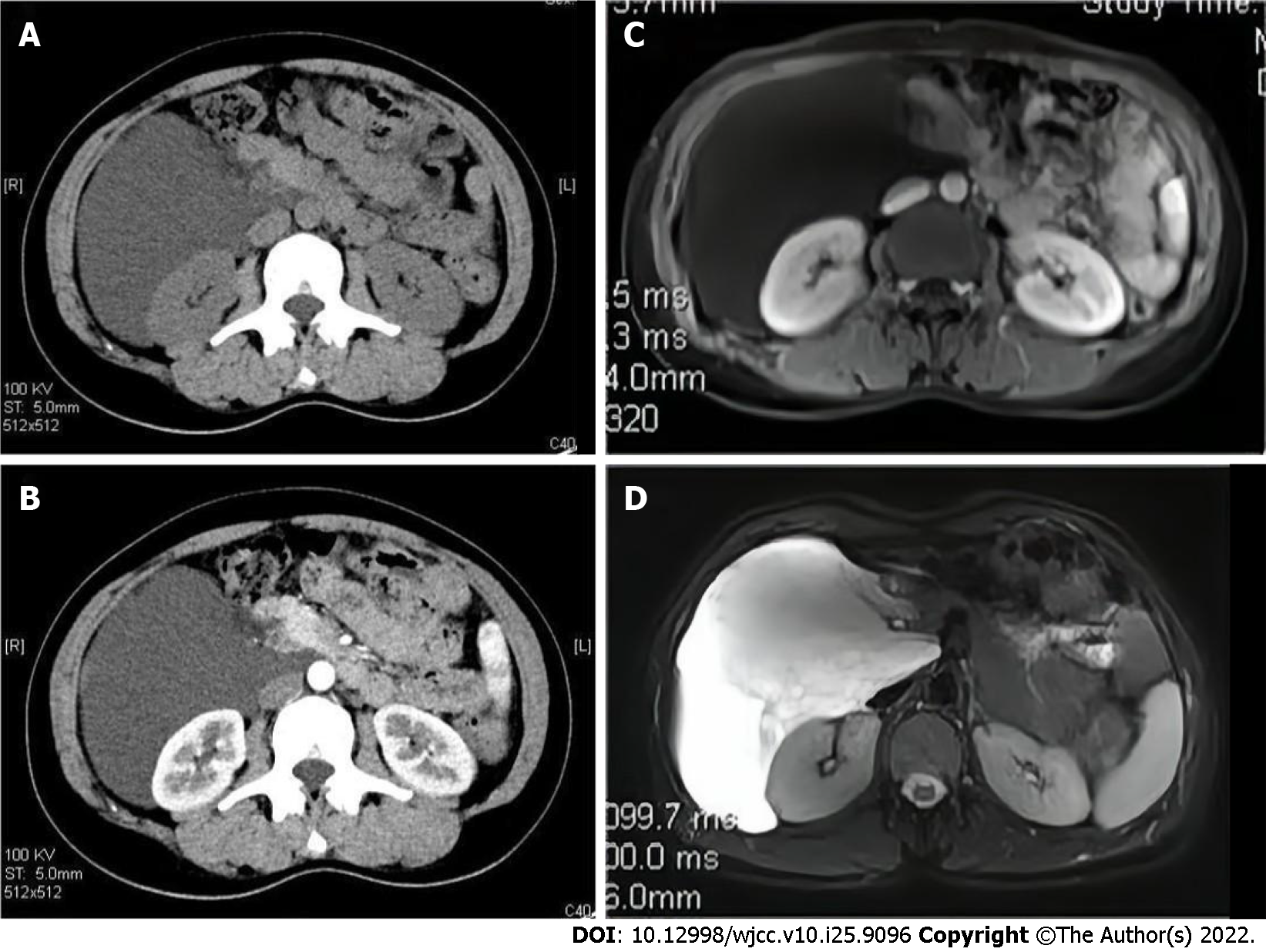
Abdominal computed tomography (CT) (Figure 1A and B) revealed an enormous hypodense mass extending from the lower edge of the liver down to the right groin, with a regular margin and without marked enhancement in the arterial phase of the enhanced CT, which suggested a benign tumor. Magnetic resonance imaging (MRI) (Figure 1C and D) revealed a retroperitoneal mass with low signal intensity on the T1-weighted image and high signal intensity on the T2-weighted image. A benign cyst in the right retroperitoneum was diagnosed based on these findings.
Retroperitoneal venous hemangioma.
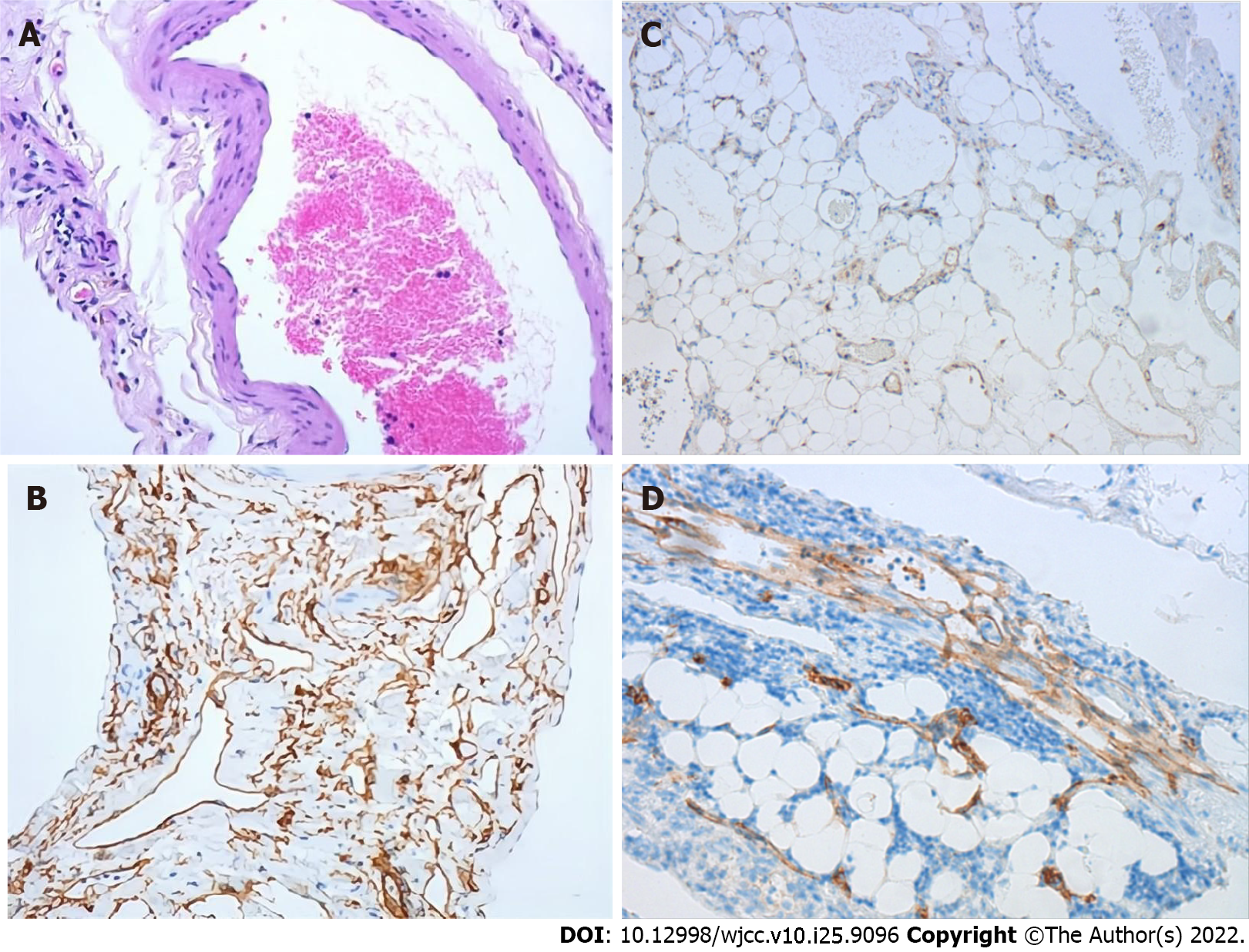
A laparoscopic exploration and cystectomy were performed. During the laparoscopic surgery, it was found that a milky white cystic neoplasm measuring approximately 20 cm was loosely attached to the muscular tissue. The tumor displaced the intestine and caused compression of the inferior vena cava, right kidney, as well as the bladder, without signs of infiltration. Moreover, the mass protruded from the retroperitoneal space into the duodenal wall, and was firmly attached to the wall of the second part of the duodenum and the head of the pancreas. Therefore, we chose to separate the loosely attached capsule wall initially, and milky liquid was noted during the separation process. The fluid was immediately taken for laboratory testing, and the results indicated that amylase was not elevated. About 2 L of milky white liquid was drained intraoperatively. Then to protect the duodenum and pancreas, the cystic wall which was tightly adhered to the duodenum was removed by laparotomy. There was no significant blood loss, and the entire capsule wall was completely resected (Figure 2). A 8 cm grayish specimen and a 5 cm fawn cystic specimen were obtained for pathological examination. Microscopic examination showed that the cystic wall was lined by a single layer of flattened cells, with smooth muscle cells and adipose tissue located around this layer. The immunohistochemical study showed that these cells stained positive for smooth muscle actin (SMA) and vascular marker CD34, and some endothelial cells were positive for CD31 and D2-40. No atypical cells with hyperproliferation or mitotic division were observed, and the proliferation marker (Ki-67 antigen) expression was less than 5 (Figure 3). In brief, these findings indicated that the retroperitoneal mass, which was derived from the vein, was a venous hemangioma.
The patient had an uneventful recovery, and no residual mass in the retroperitoneum was verified on CT scan 1 mo postoperatively. At the 6-mo follow-up evaluation, the patient was doing well without recurrence of hemangioma.
Venous hemangioma is a benign and non-invasive type of tumor, and is rarely identified due to the absence of clinical manifestations. A retroperitoneal benign tumor is comparatively rare, and hemangiomas are exceptional. Most hemangiomas are present at birth, some regress spontaneously, and others proliferate during puberty or pregnancy or following local trauma[4]. Hemangiomas may occur in any part of the body, but are extremely unusual in the retroperitoneum[5]. Almost all retroperitoneal hemangiomas are cavernous hemangiomas, and venous hemangioma is very rare[6].
A search was conducted in the PubMed database using the term "retroperitoneal hemangioma." The clinical characteristics of the disease in the relevant studies are shown in Table 1. Abdominal distension and pain were the two most common manifestations. In asymptomatic patients, the retroperitoneal mass was usually an incidental finding during a medical examination or emergent spontaneous bleeding. Tumors were removed entirely by means of laparoscopy or laparotomy in 13 patients who all had an uneventful recovery. However, subtotal resection was performed in one patient due to technical difficulties. Follow-up MRI seven months after surgery showed a reduction in size and no signs of recurrence.
| Ref. | Age | Sex | Complaints | Location | Treatment | Pathological types | Outcome |
| Powis and Rushton[18] | 26 | F | Abdominal swelling | Right abdomen | Total resection | Venous hemangioma | Uneventful |
| Igarashi and Hanazaki[6] | 28 | M | Hemangioma recurrence | Left lumbar | Total resection | Venous hemangioma | Uneventful |
| Martín-Fernández et al[5] | 39 | NM | Heartburn and abdominal pain | Right abdomen | Total resection | Venous hemangioma | Uneventful |
| Pérez Martín et al[4] | 26 | F | Dyspepsia and back pain | Left lumbar | Laparoscopy | Venous hemangioma | Uneventful |
| Tseng et al[19] | 61 | F | NM | Retroperitoneum | Subtotal resection | Venous hemangioma | Smaller residual |
| Forbes[11] | 75 | M | Abdominal and back pain | Left retroperitoneum | Laparotomy | Cavernous hemangioma | Uneventful |
| Choi and Oh[14] | 29 | F | Incidentally found | Right abdomen | Laparoscopy | Cavernous hemangioma | Uneventful |
| Kobayashi et al[13] | 54 | M | Left flank pain | Left Retroperitoneum | Laparoscopy | Venous hemangioma | Recurrence |
| He et al[7] | 38 | M | Dull epigastralgia | Right upper quadrant | Laparotomy | Cavernous hemangioma | Uneventful |
| Nakatsuka et al[8] | 65 | F | Abdominal fullnes | Right side of uterine | Total resection | Venous malformation | Uneventful |
| Hanaoka et al[10] | 36 | M | Right upper quadrant pain | Right retroperitoneum | Laparotomy | Cavernous hemangioma | Uneventful |
| Amati et al[20] | 20 | F | Abdominal distention and pain | Retroperitoneum | Laparotomy | Malformation | Uneventful |
| Chen et al[9] | 46 | F | Right waist pain | Near renal pelvis | Laparoscopy | Cavernous hemangioma | Uneventful |
| Laih et al[3] | 57 | F | Incidentally found | Right retroperitoneum | Laparotomy | Cavernous hemangiomas | Uneventful |
The manifestations of retroperitoneal hemangioma are non-specific, and include abdominal pain, heartburn, dyspepsia, back pain, epigastralgia, as well as abdominal distension[4,5,7-9]. Our patient was found to have a retroperitoneal mass without symptoms during a medical examination. Routine preoperative laboratory examinations were made, including blood, urine and serum amylase tests, and all were within the normal ranges, but tumor markers were not tested. We speculated that the mass was not discovered earlier due to the sizeable retroperitoneal space and slow development of the mass. Retroperitoneal hemangioma typically has no initial symptoms, and the appearance of clinical manifestations is usually caused by an increase in tumor size and its compression of other organs or spontaneous bleeding[10,11]. Due to the non-specific presentation and low incidence, an accurate diagnosis before surgery is extremely challenging.
Recurrence of hemangioma is very rare. Only one case has been reported previously[6], in a 28-year-old man who underwent resection of a left lumbar cavernous hemangioma. However, two years later, he was admitted to hospital with recurrence of the left lumbar hemangioma. Abdominal CT revealed a large retroperitoneal tumor with a papillary structure. The tumor was completely resected, and the pathologic diagnosis was retroperitoneal venous hemangioma. Moreover, no cases of malignancy arising from retroperitoneal hemangioma were reported. As a result, more attention should be paid to patients with recurrent hemangioma, and complete resection of the cyst wall of the tumor and postoperative follow-up are necessary.
There are many imaging findings are not specific, but can aid to categorize the lesion as probably benign. CT is the primary imaging method for diagnosing retroperitoneal hemangioma. Although it lacks the specificity of presentation, it is helpful in the initial identification of benign or malignant masses. Abdominal ultrasonography is also an important technique for differential diagnosis. The main imaging features of the disease in the relevant studies are shown in Table 2. Laih et al[3] reported a patient whose abdominal ultrasonography showed a heterogeneous hypoechoic mass in the right retroperitoneal cavity. Similarly, the present patient presented to our hospital with the abdominal ultrasonography result of a hypoechoic cystic mass in the right retroperitoneal cavity during a medical examination. Abdominal ultrasonography is conducive to differentiating solid and cystic masses. Furthermore, abdominal CT is a preliminary examination for hemangioma, which may reveal a hypodense mass without or with slight enhancement in the arterial phase[12,13]. For example, Choi and Oh[14] reported a patient in whom a mass with internal multiple small calcifications (phleboliths) was identified by abdominal CT, and the mass showed slightly increased enhancement. We speculated that this phenomenon was probably caused by internal phleboliths of the mass, which can occur with slight or marked enhancement. In our patient, abdominal CT revealed an enormous hypodense mass with a regular margin and without marked enhancement in the arterial phase of enhanced CT. In addition, MRI is an alternative technique, which is especially helpful in distinguishing the surrounding soft tissue structures. The mass was hypointense on the T1-weighted image, and was hyperintense on the T2-weighted image[10,15]. In our case, it was suggested that the patient should undergo further MRI examination, which revealed the retroperitoneal mass with low signal intensity on the T1-weighted image and high signal intensity on the T2-weighted image. However, accurate preoperative diagnosis of retroperitoneal venous hemangiomas is very difficult. Therefore, it is recommended that preoperative imaging be used to assess both the benignity and malignancy of the tumor and the location and proximity to organs and structures surrounding tissue structures.
| Ref. | Age | Sex | Location | Imaging studies |
| Powis and Rushton[18] | 26 | F | Right abdomen | Intravenous pyelography show a soft-tissue mass compressing and displacing the ureter |
| Igarashi and Hanazaki[6] | 28 | M | Left lumbar | CT show a papillary structured mass in the left peritoneum, and slight enhancement in the late phase of the enhanced CT. Ultrasonography show a hyperechoic mass lesion |
| Martín-Fernández[5] | 39 | NM | Right abdomen | Ultrasonography and CT show a solid-cystic mass with septations |
| Pérez Martín[4] | 26 | F | Left lumbar | Ultrasonography and CT show a retroperitoneal solid cystic polylobulated mass |
| Tseng et al[19] | 61 | F | Retroperitoneum | Ultrasonography and CT show heterogeneous mass |
| Forbes[11] | 75 | M | Left retroperitoneum | CT show left-sided retroperitoneal hemorrhage |
| Choi and Oh[14] | 29 | F | Right abdomen | Ultrasonography show a hypoechogenic mass, and CT show irregular shaped mass with internal multiple small calcifications (phleboliths) |
| Kobayashi et al[13] | 54 | M | Left Retroperitoneum | CT show a cystic mass with the thickened wall having a contrast enhancement |
| He et al[7] | 38 | M | Right upper quadrant | Ultrasonography showed a giant cystic mass, and CT show a low density mass with mild enhancement |
| Nakatsuka et al[8] | 65 | F | Right side of uterine | MRI show a cystic with high intensity on the T2-weighted image |
| Hanaoka et al[10] | 36 | M | Right retroperitoneum | CT show a tumor without marked contrast enhancement, MRI show the tumor with low intensity on the T1-weighted image and high intensity on the T2-weighted image |
| Amati et al[20] | 20 | F | retroperitoneum | CT show a low density mass with regular borders and contrast-enhanced septation |
| Chen et al[9] | 46 | F | Near renal pelvis | CT show an ill-defined soft tissue mass with unevenly enhanced and with calcified margins. MRI show significant and continuous uneven mass, limited diffusion weighted imaging (DWI), and high signal intensity on apparent diffusion coefficient (ADC) map |
| Laih et al[3] | 57 | F | Right retroperitoneum | Ultrasonography show a heterogeneous hypoechoic lesion, and CT show heterogeneous enhancement over the right retroperitoneum |
Surgical resection is the mainstay of treatment for retroperitoneal venous hemangioma. Even though retroperitoneal hemangioma is a benign tumor, the enlarged tumor may compress the surrounding organs and cause rupture and bleeding. In our patient, a mass approximately 20 cm was found in the right retroperitoneum following laparoscopic exploration. The tumor compressed the adjacent tissues and organs, and most importantly, the mass was firmly attached to both the wall of the second part of the duodenum and the head of the pancreas. Therefore, in order to completely remove the capsule wall of the mass and protect the surrounding organs, we chose to resect the tumor by laparotomy. Consequently, the patient had a successful postoperative recovery and follow-up was uneventful.
The pathological features of a venous hemangioma consist of positivity for the vascular markers CD34 and CD31, and the vascular wall contains smooth muscle and is lined with a single layer of endothelial cells[4,16,17]. In our case, microscopic examination showed that the cystic wall was lined by a single layer of flattened cells, smooth muscle cells, as well as adipose tissue. Immunohistochemistry was positive for SMA, CD34 and CD31. These findings were consistent with a typical venous hemangioma.
Although imaging has provided assistance in the diagnosis of retroperitoneal cysts, we did not focus on adhesion of the mass to the surrounding organs. Moreover, sufficient evidence to demonstrate the superiority of laparoscopy for the treatment of retroperitoneal venous hemangioma is lacking. It is suggested that the appropriate procedure should be chosen according to the patient's condition before surgery.
Venous hemangioma is a rare benign lesion in adults, and an accurate diagnosis before surgery is challenging due to non-specific manifestations, imaging features and low incidence. Retroperitoneal venous hemangiomas essentially involve no malignancy, but venous hemangiomas may grow and cause symptoms of compression as well as adhering to surrounding tissues. When symptomatic massive hemangiomas are present, surgery is considered. In addition, surgery is the curative treatment for venous hemangioma, and the definitive diagnosis relies on pathology. Attention should be paid to lesion residues after resection, and CT should be reviewed periodically during the follow-up period.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chae HB, South Korea; Dayan D, Israel; Tangsuwanaruk T, Thailand S-Editor: Wang DM L-Editor: A P-Editor: Wang DM
| 1. | St Leinung, Würl P, Frey A, Lochhaas L, Lotz I, Schönfelder M. [Monstrous venous hemangioma of the retroperitoneum. Problems in diagnosis]. Zentralbl Chir. 1999;124:843-847. [PubMed] |
| 2. | Shah M, Freeman LM, Chitkara M, Chun KJ. Retroperitoneal hemangioma demonstrated on blood pool scan. Clin Nucl Med. 2014;39:e265-e266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Laih CY, Hsieh PF, Chen GH, Chang H, Lin WC, Lai CM, Chang CH. A retroperitoneal cavernous hemangioma arising from the gonadal vein: A case report. Medicine (Baltimore). 2020;99:e22325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Pérez Martín RN, Estebanez Zarranz J, Velasco Fernández Mdel C, Conde Redondo C, Amón Sesmero J, Martinez-Sagarra J. Laparoscopic resection of retroperitoneal venous hemangioma. J Urol. 2004;171:336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Martín-Fernández J, López-Péréz R, Ramia-Angel JM, Padilla-Valverde D, López-Buenadicha A, Hernández-Calvo J. Soft-tissue images. Retroperitoneal venous angioma. Can J Surg. 2001;44:169. [PubMed] |
| 6. | Igarashi J, Hanazaki K. Retroperitoneal venous hemangioma. Am J Gastroenterol. 1998;93:2292-2293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | He H, Du Z, Hao S, Yao L, Yang F, Di Y, Li J, Jiang Y, Jin C, Fu D. Adult primary retroperitoneal cavernous hemangioma: a case report. World J Surg Oncol. 2012;10:261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Nakatsuka S, Shigeta N, Ojima Y, Kimura H, Nagano T, Ito K. A large retroperitoneal cystic venous malformation mimicking bilateral ovarian cystic tumors. Arch Gynecol Obstet. 2012;286:1011-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Chen ZJ, Wang D, Fan SD, Ren SQ, Zhou F, Nie Y, Lv Q, Tian JZ. DaVinci robotic-assisted laparoscopic resection of parapelvic cavernous hemangioma: a case report. BMC Surg. 2020;20:186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Hanaoka M, Hashimoto M, Sasaki K, Matsuda M, Fujii T, Ohashi K, Watanabe G. Retroperitoneal cavernous hemangioma resected by a pylorus preserving pancreaticoduodenectomy. World J Gastroenterol. 2013;19:4624-4629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Forbes TL. Retroperitoneal hemorrhage secondary to a ruptured cavernous hemangioma. Can J Surg. 2005;48:78-79. [PubMed] |
| 12. | Abe K, Akata S, Ohkubo Y, Park J, Kakizaki D, Simatani H, Furukawa K, Kato H, Serizawa H, Abe K. Venous hemangioma of the mediastinum. Eur Radiol. 2001;11:73-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Kobayashi H, Kaneko G, Uchida A. Retroperitoneal venous hemangioma. Int J Urol. 2010;17:585-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Choi YS, Oh HK. Laparoscopic resection of a retroperitoneal hemangioma arising from ovarian vessels. J Minim Invasive Gynecol. 2009;16:778-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Mossanen M, Dighe M, Gore J, Mann G. Large retroperitoneal hemangioma encompassing the renal vein. Can Urol Assoc J. 2015;9:E894-E896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Zhang C, Luo W, Ma L, Ni Y. Venous hemangioma of the azygos arch. Eur J Cardiothorac Surg. 2007;32:669-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Odaka M, Nakada T, Asano H, Yabe M, Kamiya N, Hirano J, Morikawa T. Thoracoscopic resection of a mediastinal venous hemangioma: Report of a case. Surg Today. 2011;41:1455-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Powis SJ, Rushton DI. A case of retroperitoneal haemangioma. Br J Surg. 1972;59:74-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Tseng TK, Lee RC, Chou YH, Chen WY, Su CH. Retroperitoneal venous hemangioma. J Formos Med Assoc. 2005;104:681-683. [PubMed] |
| 20. | Amati AL, Hecker A, Schwandner T, Ghanem H, Holler J, Reichert M, Padberg W. A hemangioma of the sigmoid colon mesentery presenting as a retroperitonealtumor: a case report and review. World J Surg Oncol. 2014;12:79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |