Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.9057
Peer-review started: April 13, 2022
First decision: May 12, 2022
Revised: May 25, 2022
Accepted: July 18, 2022
Article in press: July 18, 2022
Published online: September 6, 2022
Processing time: 135 Days and 5.3 Hours
The rupture of a splenic artery aneurysm (SAA) in pregnancy is an uncommon condition. However, it is associated with high mortality rates in pregnant women and fetuses even after surgical treatment. Though the endovascular treatment of SAAs is currently preferred as it can improve the outcomes even in emergent cases, the endovascular treatment of a ruptured SAA during pregnancy has not been reported until date.
We report a case of a 33-year-old woman with the sudden onset of epigastric pain due to a ruptured SAA at the mid-portion of the splenic artery at 18 wk of pregnancy. After emergent initial resuscitation, the patient was diagnosed with a ruptured SAA through digital angiography. Immediately upon diagnosis, she underwent emergent endovascular embolization of the splenic artery for the rupture on the spot. Next, surgery was performed to remove the hematoma under stable conditions. Although the fetus was found to be dead during resuscitation, the woman recovered without complications and was discharged 15 d postoperatively.
Endovascular treatment might be a valuable alternative to surgery/lead to safer surgery for selected pregnant patients with ruptured SAAs.
Core Tip: Though the endovascular treatment of a splenic artery aneurysm (SAA) is currently preferred as it can improve outcomes, endovascular treatment for a ruptured SAA during pregnancy has not been reported. It is still debatable whether a primary emergent laparotomy or angiographic embolization of an SAA followed by laparotomy is the best approach. However, similar to our case, when the patients whose vital signs are too unstable to wait for surgery or in hemodynamically unstable pregnant patients with a low chance of fetal survival, the endovascular treatment should be considered. This might be a valuable alternative to surgery/lead to safer surgery.
- Citation: Lee SH, Yang S, Park I, Im YC, Kim GY. Ruptured splenic artery aneurysms in pregnancy and usefulness of endovascular treatment in selective patients: A case report and review of literature. World J Clin Cases 2022; 10(25): 9057-9063
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/9057.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.9057
A splenic artery aneurysm (SAA) is a rare clinical entity during pregnancy. However, a ruptured SAA is associated with high mortality rates in pregnant women and fetuses[1-3]. Regardless of pregnancy, the high mortality rates might be attributable to the asymptomatic characteristics of the aneurysm, rapid deterioration after rupture, and misdiagnosis[2]. Therefore, it is essential to make an early and accurate diagnosis because if surgical treatment is not emergently performed for pregnant women with a ruptured SAA, the condition can become life-threatening. Generally, the classical therapy for a ruptured SAA has been surgical treatment. However, the postoperative mortality rate remains high even after the introduction of the laparotomy approach[4-6].
Recent practice guidelines recommend endovascular treatment as the standard tool for diagnosis as well as an emerging therapy that can continuously improve the outcomes of patients with SAA and other visceral aneurysms[7,8]. Although it is potentially hazardous to the fetus due to radiation and intravascular contrast media exposure, some authors recommend angiographic embolization via an endovascular approach as a useful diagnostic and therapeutic tool for pregnant patients with unruptured SAAs[9,10].
Classically, either ligation or resection with or without splenectomy has been performed for a ruptured SAA through laparotomy. Some authors recommend angiographic embolization via an endovascular approach for those with a ruptured SAA to stop hemorrhaging, even if the hemodynamic status of the patient is unstable[11,12].
It is still debatable whether a primary emergent laparotomy or angiographic embolization of an SAA followed by laparotomy is the best approach. Proponents of angiographic embolization via the endovascular approach think that it is better than primary laparoscopic surgery because it can provide superior visualization of the surgical field, thus reducing maternal mortality during surgery[13,14]. To the best of our knowledge, endovascular treatment for a ruptured SAA during pregnancy has not been reported yet.
Here we report the case of a 33-year-old pregnant woman with a ruptured SAA during the second gestational trimester that was successfully treated with angiographic embolization.
A 33-year-old woman visited the Emergency Department (ED) due to the sudden onset of epigastric pain that started several hours before arrival.
The patient was the first pregnant woman at 18 wk of gestation.
The patient had no past illness and was not on any medication.
The patient had no pertinent family history.
The patient's initial vital signs appeared stable, except for minor pallor of the conjunctiva. Blood pressure was 128/80 mmHg, heart rate was 80-105 beats/min with normal sinus rhythm, peripheral capillary oxygen saturation (SpO2) was 95%-98%, respiratory rate was 20 breaths/min, and the temperature was 36.5 ℃. She was fully conscious (Glasgow Coma Scale: E4V5M6). Physical examination revealed moderate tenderness in her epigastric region, normoactive bowel sounds, fullness in the epigastric region, and no abdominal guarding or rigidity were noted on examination. Also, there was no rebound tenderness. About 1 h after arrival, her vital signs became suddenly unstable, showing hypotension (BP = 70/40 mm/Hg) and tachycardia (HR = 130 beats/min). Her abdomen gradually expanded, and she finally lost consciousness. Resuscitative measures including intubation for a free airway, intravenous access, hydration with crystalloids, and blood transfusion for recovering decreased hemoglobin were performed.
Although the initial hemoglobin level was 7.9 g/dL and all other laboratory examinations were unremarkable, the laboratory workup after resuscitation showed severe anemia (hemoglobin, 3.5 g/dL), leukocytosis (white blood cell count, 20470 cells/mm³), and low platelets (platelet level, 68000 cells/mm³). Post-intubation blood gas analysis revealed a pH of 6.99, paO2 of 427 mmHg, pCO2 of 45 mmHg, and bicarbonate of 10.8 mmol/L/L.
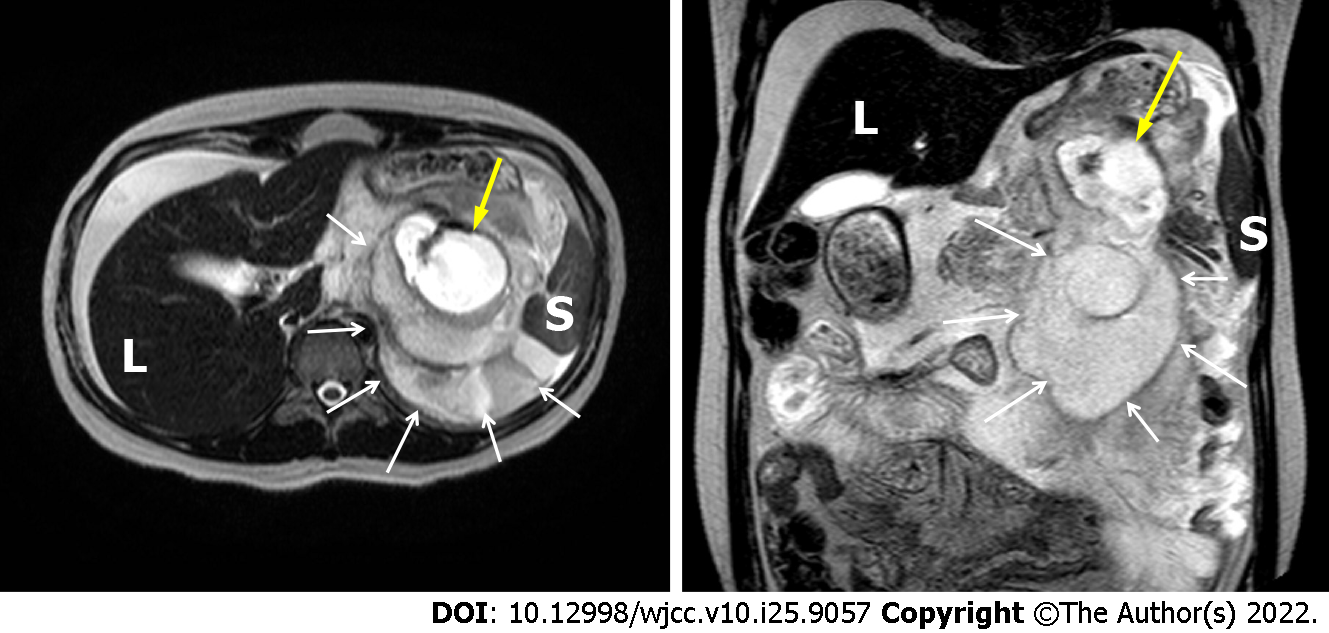
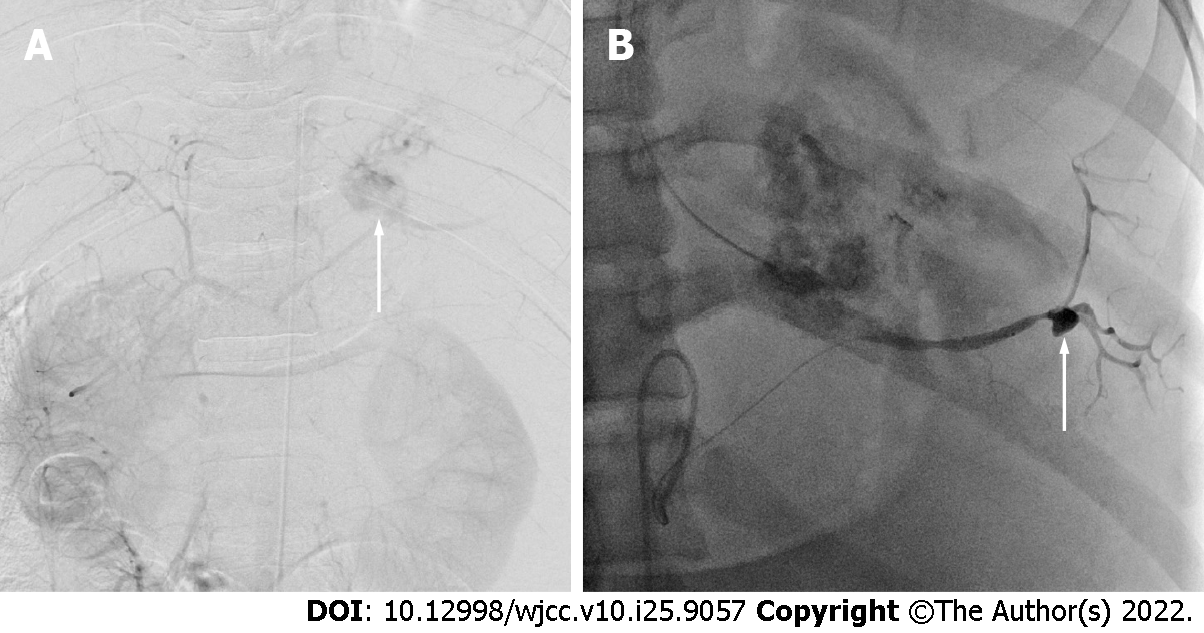
A focused assessment with sonography for trauma (FAST) scan was performed in the ED for further evaluation when the patient's vital signs were unstable; the scan showed no specific findings. When the maternal blood pressure and other vital signs improved briefly after resuscitation, urgent magnetic resonance imaging (MRI) was performed rather than computed tomography for a more accurate diagnosis due to the presence of the fetus. MRI indicated the presence of a huge retroperitoneal hematoma with the possibility of a ruptured SAA (Figure 1). In addition, digital angiography detected two SAAs. One was at the mid-portion of the splenic artery measuring 60 mm in size, showing the extravasation of contrast media. Another was at the hilum portion with a saccular type measuring 6 mm in size (Figure 2).
Based on the patient's symptoms, history of pregnancy, MRI, and digital angiography, the patient was finally diagnosed with a ruptured SAA.
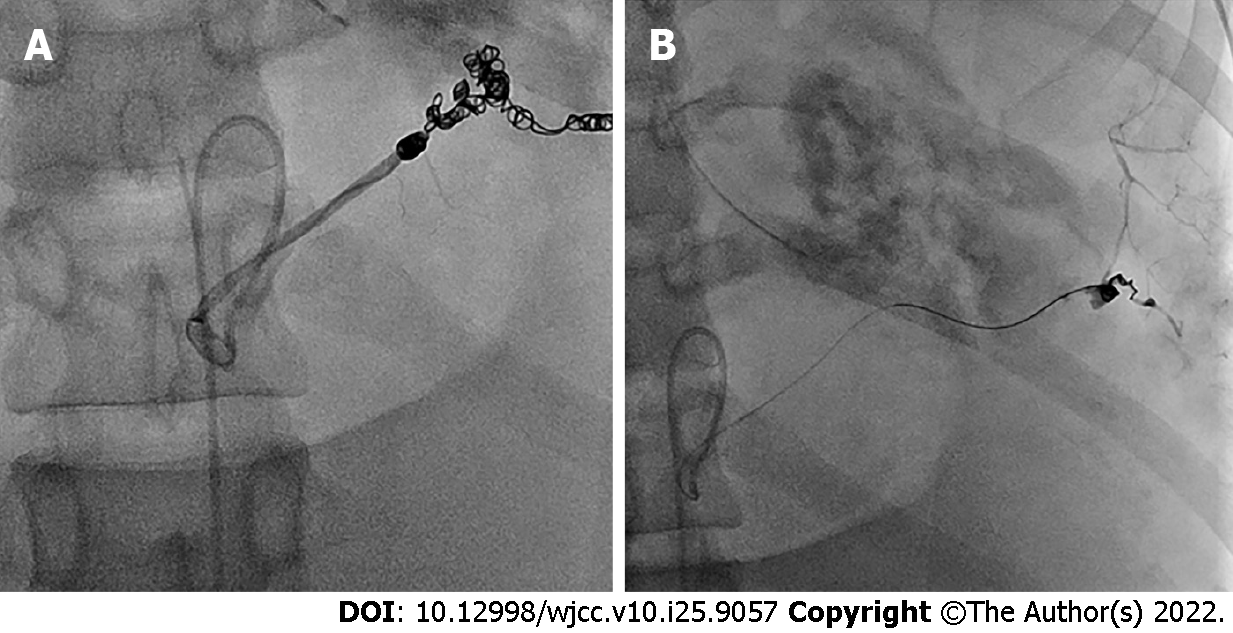
We decided to perform endovascular treatment and discussed it with the patient's caregiver because it was judged that the patient's vital signs would not remain stable until surgery. Two SAAs were identified through an urgent digital angiography, and they were all successfully embolized using an intraarterial coil (Figure 3). Although the procedure successfully embolized all the aneurysms and her vital signs became stable, she still had a tense abdomen. In addition, she complained of abdominal pain due to a large amount of preexisting hematoma. Her abdominal wall was too tense, and decreased wall compliance was seen. We worried about abdominal compartment syndrome. Therefore, we performed a laparotomy to evacuate the hematoma and remove the ruptured aneurysm with a splenectomy. During the laparotomy, a massive hematoma was identified in the left upper quadrant area. After evacuating the hematoma, we found the presence of a tiny amount of bleeding from the ruptured SAA, which was embolized by endovascular treatment. The splenic artery was ligated and divided at its origin. Because another aneurysm was identified at the hilar portion in the preoperative digital angiography, we subsequently removed all aneurysms and performed a splenectomy. During the surgery, the patient received 16 units of packed red blood cells, 19 units of fresh frozen plasma, 30 units of platelets, and ten units of cryoprecipitate. All procedures were performed while the patient was in a stable condition. The pathological examination showed one intact hilar aneurysm and a ruptured mid-portion aneurysm, the widest one measuring 5.9 cm with an intraluminal thrombus. Microscopic examination revealed very thin walls of the aneurysms and a lack of elastin with a large infarcted area. There was no evidence of vasculitis or neoplasm.
At postoperative three days, the obstetrician removed the dead fetus that was found to be dead at initial resuscitation. After six days of intensive care unit care, the patient was transferred to a general ward. The patient had an unremarkable recovery. She was discharged 15 d postoperatively in a stable condition.
In this first case report of angiographic embolization via an endovascular approach for a ruptured SAA during pregnancy, we have demonstrated that endovascular therapy could be particularly useful in quickly stabilizing vital signs and effectively improving hemodynamic instability.
Abdominal pain is one of the most common symptoms of pregnant women. When patients present with hemodynamic collapse, a clinician should expand the differential diagnosis. The common causes of hypotension in pregnant patients include dehydration, ruptured ectopic pregnancy, and uterine abnormalities. However, less common non-obstetrical etiologies such as pulmonary embolism, hepatic rupture, and ruptured abdominal and visceral artery aneurysms should also be considered[15]. Misdiagnosis of these intra-abdominal sources of bleeding is common, with potentially devastating outcomes[15].
An SAA during pregnancy was first reported in 1770[16]. The exact prevalence of SAAs during pregnancy remains unknown. SAAs occurs more frequently in women than in men. SAAs during pregnancy rupture in 50% of the cases[17]. Two-thirds of ruptured SAAs during pregnancy occurs in the third trimester of gestation, typically within the last two weeks of pregnancy. Sometimes it occurs in the second trimester, as in the present case[2,17,18].
The etiology of SAA rupture in pregnancy remains unclear. The influence of hormones such as estrogen, progesterone, and relaxin on the arterial wall might contribute to elastin disruption in the tunica media of the vasculature[19,20]. Pregnancy is the major precipitating factor that increases intra-abdominal pressure. SAA rupture during pregnancy can occur due to higher pressure within the splenic artery caused by increased intra-abdominal pressure with increasing gestational age[21,22].
The clinical symptoms of SAA are mostly asymptomatic. Regardless of pregnancy, it is difficult to diagnose ruptured SAA until it is clinically recognized. The clinical symptoms of a ruptured SAA are related to the abdomen and chest. Therefore, the early symptoms of ruptured SAA rupture during pregnancy are often misdiagnosed as placental abruption, uterine rupture, and pulmonary embolism[17,23].
According to the reported studies, about 70% of ruptured SAAs in pregnant women were initially misdiagnosed as uterine ruptures[17]. Therefore, obstetricians and gynecologists need to distinguish between obstetrical bleeding and non-obstetrical bleeding for optimal treatment. In our case, initially, we performed a FAST because the patient was suspected of having intra-abdominal bleeding associated with an obstetric origin. However, we did not find any cause of bleeding in the FAST. Finally, we detected the aneurysmal rupture by MRI and digital angiography.
Although a ruptured SAA is uncommon, it is often life-threatening. The mortality for a ruptured SAA in nonpregnant patients is approximately 25%-36%[4,24]. However, mortality is nearly doubled for pregnant patients, showing maternal mortality of 65%-75% and fetal mortality of more than 90%[3]. Such high rates of mortality can be associated with delayed diagnosis and treatment. Therefore, for a ruptured SAA during pregnancy, early diagnosis, immediate maternal resuscitation that will resuscitate the fetus, bleeding cessation, and definitive surgical intervention through laparotomy are essential. Splenectomy or splenopancreatectomy is usually employed in these cases with ligation of the splenic artery[25]. Nevertheless, surgery for a ruptured SAA can have a mortality rate of 10%-76%[3,26] and a perioperative complication rate of 9%-25% due to splenic or pancreatic injury[6,27].
Although surgery is still the standard gold treatment, a surgical intervention strategy might delay hemostasis. In the case of surgery, the surgical team must be organized, general anesthesia and the surgical approach should be performed, and the disease lesion must be identified.
However, minimally invasive endoluminal techniques including embolization and stent implantation via an endovascular approach have been used as emerging treatments for patients with SAAs and other visceral aneurysms because they can be diagnosed and treated simultaneously, thereby reflecting the trend of applying less invasive techniques as the first-line therapy in intravascular fields in the recent years[8,28,29]. Our case also showed that the ruptured arterial aneurysms were identified through an urgent digital angiography and were all successfully embolized simultaneously. In addition, endovascular treatment quickly stabilized the patient's hemodynamic status.
The success rate has been reported to range from 85% to 92% for intravascular therapy, including embolization and stent implantation in patients with SAAs[30]. Moreover, low postoperative mortality and morbidity rates are among the main advantage of embolization over surgery[5,8].
Based on previous studies and our case, the reasons for using an endovascular approach for a ruptured SAA during pregnancy are as follows: (1) It detects the existence of other asymptomatic aneurysms and provides an opportunity to treat them; (2) If surgical treatment is needed after endovascular treatment, this may lead to a safer surgery for a patient in a stable vital state as it can serve as a “bridge” between an unstable preoperative state and surgery[31]; (3) It provides a relatively less bloody operative field to reduce damage to the surrounding organs; and (4) It could be used to palpate coils in the splenic artery and aneurysmal sac, enabling the accurate identification of the location of the lesion. In highly selected pregnant patients, especially for the patients whose vital signs are too unstable to wait for surgery or hemodynamically unstable pregnant patients with a low chance of fetal survival, it might be a useful treatment.
We report a case of a ruptured SAA successfully treated by angiographic embolization in a patient at 18 wk of pregnancy. Endovascular treatment might be a valuable alternative to surgery or lead to safer surgery as it can improve the outcome of selected pregnant patients with ruptured SAAs.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ding X, China; Shekouhi R, Iran S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Kalof AN, Fuller B, Harmon M. Splenic pregnancy: a case report and review of the literature. Arch Pathol Lab Med. 2004;128:e146-e148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Sadat U, Dar O, Walsh S, Varty K. Splenic artery aneurysms in pregnancy--a systematic review. Int J Surg. 2008;6:261-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 115] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Lee PC, Rhee RY, Gordon RY, Fung JJ, Webster MW. Management of splenic artery aneurysms: the significance of portal and essential hypertension. J Am Coll Surg. 1999;189:483-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 100] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Akbulut S, Otan E. Management of Giant Splenic Artery Aneurysm: Comprehensive Literature Review. Medicine (Baltimore). 2015;94:e1016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Hogendoorn W, Lavida A, Hunink MG, Moll FL, Geroulakos G, Muhs BE, Sumpio BE. Open repair, endovascular repair, and conservative management of true splenic artery aneurysms. J Vasc Surg. 2014;60:1667-76.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Pulli R, Dorigo W, Troisi N, Pratesi G, Innocenti AA, Pratesi C. Surgical treatment of visceral artery aneurysms: A 25-year experience. J Vasc Surg. 2008;48:334-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 228] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 7. | Mariúba JVO. Splenic aneurysms: natural history and treatment techniques. J Vasc Bras. 2019;19:e20190058. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Lakin RO, Bena JF, Sarac TP, Shah S, Krajewski LP, Srivastava SD, Clair DG, Kashyap VS. The contemporary management of splenic artery aneurysms. J Vasc Surg. 2011;53:958-64; discussion 965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Ikenaga S, Yunaiyama D, Saguchi T, Otaka J, Yamada T, Ito H, Sugimoto K, Itoi T, Saito K. A case of a patient who underwent transcatheter arterial embolization for unruptured splenic aneurysm during pregnancy. Radiol Case Rep. 2021;16:78-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Parrish J, Maxwell C, Beecroft JR. Splenic Artery Aneurysm in Pregnancy. J Obstet Gynaecol Can. 2015;37:816-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Nincheri Kunz M, Pantalone D, Borri A, Paolucci R, Pernice LM, Taruffi F, Andreoli F. Management of true splenic artery aneurysms. Two case reports and review of the literature. Minerva Chir. 2003;58:247-256. [PubMed] |
| 12. | Huang YK, Hsieh HC, Tsai FC, Chang SH, Lu MS, Ko PJ. Visceral artery aneurysm: risk factor analysis and therapeutic opinion. Eur J Vasc Endovasc Surg. 2007;33:293-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Ologun G, Sharpton K, Granet P. Successful use of resuscitative endovascular balloon occlusion of the aorta in the treatment of ruptured 8.5-cm splenic artery aneurysm. J Vasc Surg. 2017;66:1873-1875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Yamashita H, Ohuchida J, Shimura H, Aibe H, Honda H, Kuroki S, Chijiiwa K, Tanaka M. Laparoscopic splenectomy aided by balloon occlusion of the splenic artery: report of a case. Surg Laparosc Endosc. 1996;6:326-329. [PubMed] |
| 15. | Jackson HT, Diaconu SC, Maluso PJ, Abell B, Lee J. Ruptured splenic artery aneurysms and the use of an adapted fast protocol in reproductive age women with hemodynamic collapse: case series. Case Rep Emerg Med. 2014;2014:454923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Beaussier M. Sur un anévrisme de l'artère splénique: Dont les parois se sont ossifiées. J Med Clin Pharm Paris. 1770;2:157. |
| 17. | Barrett JM, Van Hooydonk JE, Boehm FH. Pregnancy-related rupture of arterial aneurysms. Obstet Gynecol Surv. 1982;37:557-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 194] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Sam CE, Rabl M, Joura EA. [Aneurysm of the splenic artery: rupture in pregnancy]. Wien Klin Wochenschr. 2000;112:896-898. [PubMed] |
| 19. | Al-Habbal Y, Christophi C, Muralidharan V. Aneurysms of the splenic artery - a review. Surgeon. 2010;8:223-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 115] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 20. | Gourgiotis S, Alfaras P, Salemis NS. Spontaneous rupture of splenic artery aneurysm in pregnancy: a case report. Adv Med Sci. 2008;53:341-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Khurana J, Spinello IM. Splenic artery aneurysm rupture: a rare but fatal cause for peripartum collapse. J Intensive Care Med. 2013;28:131-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Oakley E, Ho JD, Johnson V, Vancamp J, Melson T, Hick JL. Splenic artery aneurysm: an important cause of hemoperitoneum and shock. J Emerg Med. 2014;46:e65-e67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Richardson AJ, Bahlool S, Knight J. Ruptured splenic artery aneurysm in pregnancy presenting in a manner similar to pulmonary embolus. Anaesthesia. 2006;61:187-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Shanley CJ, Shah NL, Messina LM. Common splanchnic artery aneurysms: splenic, hepatic, and celiac. Ann Vasc Surg. 1996;10:315-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 179] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 25. | de Perrot M, Bühler L, Deléaval J, Borisch B, Mentha G, Morel P. Management of true aneurysms of the splenic artery. Am J Surg. 1998;175:466-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | McDermott VG, Shlansky-Goldberg R, Cope C. Endovascular management of splenic artery aneurysms and pseudoaneurysms. Cardiovasc Intervent Radiol. 1994;17:179-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 120] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 27. | Trastek VF, Pairolero PC, Bernatz PE. Splenic artery aneurysms. World J Surg. 1985;9:378-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 77] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Sessa C, Tinelli G, Porcu P, Aubert A, Thony F, Magne JL. Treatment of visceral artery aneurysms: description of a retrospective series of 42 aneurysms in 34 patients. Ann Vasc Surg. 2004;18:695-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 156] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 29. | Varnagy D, Sendzischew M, Hertz JA, Sendzischew H. Endovascular management of a ruptured splenic artery aneurysm. Vasc Endovascular Surg. 2007;41:68-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Jesinger RA, Thoreson AA, Lamba R. Abdominal and pelvic aneurysms and pseudoaneurysms: imaging review with clinical, radiologic, and treatment correlation. Radiographics. 2013;33:E71-E96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 31. | Gabelmann A, Görich J, Merkle EM. Endovascular treatment of visceral artery aneurysms. J Endovasc Ther. 2002;9:38-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 107] [Article Influence: 4.7] [Reference Citation Analysis (0)] |