Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.9050
Peer-review started: March 29, 2022
First decision: May 30, 2022
Revised: June 7, 2022
Accepted: August 1, 2022
Article in press: August 1, 2022
Published online: September 6, 2022
Processing time: 150 Days and 23.5 Hours
Intradural anesthesia caused by anesthetic drug leakage during percutaneous vertebroplasty (PVP) has rarely been reported. We here report a 71-year-old woman who suffered this rare and life-threatening complication during PVP.
A 71-year-old woman, who suffered from 2 wk of severe back pain with a visual analog score of 8, came to our outpatient clinic. She was later diagnosed with a newly compressed L1 fracture and was then admitted in our department. PVP was initially attempted again under local anesthesia. However, serendipitous intradural anesthesia leading to total spinal anesthesia happened. Fortunately, after successful resuscitation of the patient, PVP was safely and smoothly performed. Great pain relief was achieved postoperatively, and she was safely discharged on postoperative day 4. The patient recovered normally at 3-mo follow-up.
Total spinal anesthesia secondary to PVP by anesthetic drug leakage rarely occurs. In cases of inadvertent wrong puncture leading to drug leakage when performing it under local anesthesia, surgeons should be highly vigilant during the whole procedure. Electrocardiogram monitoring, oxygen inhalation, intravenous cannula set prior to surgery, regular checking of motor activity and a meticulous imaging monitoring with slower pushing of anesthetic drugs, etc. should be highly recommended.
Core Tip: Total spinal anesthesia secondary to percutaneous vertebroplasty (PVP) rarely occurs. In our case, we encountered this phenomenon when performing PVP under local anesthesia. Fortunately, with our prompt interventions, the patient received a satisfactory outcome. From our experience, it is fundamentally important that electrocardiogram monitoring, oxygen inhalation, intravenous cannula set prior to surgery, regular checking of motor activity and a meticulous imaging monitoring with slower pushing of anesthetic drugs, etc. should be highly recommended.
- Citation: Wang YF, Bian ZY, Li XX, Hu YX, Jiang L. Total spinal anesthesia caused by lidocaine during unilateral percutaneous vertebroplasty performed under local anesthesia: A case report. World J Clin Cases 2022; 10(25): 9050-9056
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/9050.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.9050
Osteoporosis is a degenerative disease with a gradually deteriorated bone density and bone microarchitecture, which increases the risk of fracture[1]. As people gradually age, the incidence rate increases rapidly. One of the most common complications to elderly patients is osteoporotic vertebral com
Percutaneous vertebroplasty (PVP) was first applied in the 1980s and was used in OVCF shortly thereafter. PVP has been validated to be effective in consolidating a fractured vertebral body and relieving pain. Apparently, it greatly and immediately improves the patient’s quality of life[3,4]. Currently, a unilateral approach has also been widely accepted and regarded as a safer and much quicker way[5]. The most frequently reported complication is cement leakage. It has been reported that the rate occurring in OVCF ranges from 30% to 65%[6,7]. Rare and life-threatening cement leakage complications, such as permanent paraplegia[8], pulmonary embolism and perforation of the heart[9,10], of PVP have been sporadically reported. There are also only a few case reports discussing other complications caused by PVP, such as local bleeding at the puncture site, spinal infection and cement leakage in the vertebral canal and intervertebral foramen[11]. In addition, lumbar artery pseudoaneurysm[12] and adjacent segmental diseases[13] were also noted.
While complications of intradural anesthesia rarely occur, it could be induced in other spine surgery, such as in surgery of percutaneous endoscopic cervical discectomy and percutaneous vertebral augmentation[14,15]. Based on the literature reviewed, intradural anesthesia leading to total spinal anesthesia caused by anesthetic leakage during PVP has rarely been reported. We herein report a rare and life-threatening complication during unilateral PVP.
A 71-year-old woman who suffered from 2 wk of severe back pain (visual analog scale: 8) came to our outpatient clinic.
This patient suffered from severe back patient with no specific predisposing reasons for almost 2 wk. She was later suspected with a newly compressed lumbar fracture and was then admitted in our department.
The patient had a history of T12, L2 and L3 fracture caused by osteoporosis, which was safely treated by PVP without any complications 1 year ago.
No other remarkable past history was mentioned except PVP performed 1 year ago.
The patient’s body weight was 52 kg, height was 162 cm, and body mass index was 19.8 kg/m2. Physical examination showed: intensified pain induced when bending or twisting her spine, visual analog score of back pain was 8, and neurological deficit was not detected.
No remarkable laboratory results were found. Dual X-ray bone absorptimetry T < -3.5.
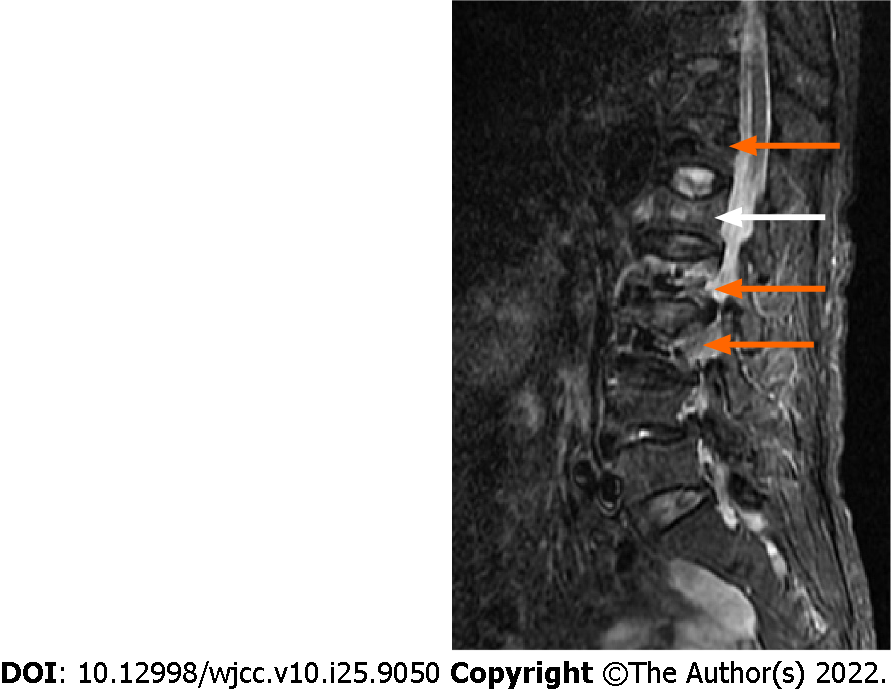
Inpatient magnetic resonance imaging showed fractured T12, L2 and L3, which was successfully treated with PVP 1 year ago. A L1 osteoporotic vertebral compression fracture was newly diagnosed (Figure 1).
Newly compressed L1 fracture.
After full examination and preoperative preparations, the patient was prepared for surgery in the prone position with electrocardiogram monitoring and oxygen inhalation of 3 L/min. Her blood pressure was 140/85 mmHg, pulse was 82 beats/min, respiration was 20/min, and SpO2 was 98%. Fluid supplementation with 0.9% sodium chloride (500 mL) was given through intravenous cannula set up prior to surgery. During the operation, we used a 20 mL syringe with a needle diameter of 0.7 mm containing 200 mg lidocaine plus 10 mL sodium chloride for local anesthesia. We injected it progressively from skin to facet joint level.
Meanwhile, we regularly checked the motor activity of the lower extremities. A puncture needle with a diameter of 3 mm was engaged to puncture. However, after 30-45 s needle puncture, we suddenly found out that our patient could not move her legs and sensation disappeared. Subsequently, the patient developed paraplegia, shortly after she lost her consciousness. Then we immediately stopped the operation. Using C-armed X-ray to recheck our patient (both anteroposteriorly and laterally), it was confirmed that the puncture needle was in a safe position, which was not into the spinal canal. We then pulled out the puncture needle and turned our patient into the supine position. Promptly, the patient’s vital signs started decreasing with a blood pressure of 60/35 mmHg, pulse of 35 beats/min, respiration of 10/min and SpO2 of 45%. For fear of a lidocaine allergic reaction, 10 mg of dexamethasone and 1 mg adrenaline were given intravenously. Fluid supplementation of sodium chloride was given with maximum speed (6 mL/min), and mask oxygen inhalation with 8 L/min was given. Fortunately, after 15 min resuscitation, the patient’s vital signs gradually recovered.
After the discussion of our surgeons and anesthesiologists, intradural anesthesia leading to total spinal anesthesia induced by lidocaine leakage during local anesthesia was suspected. Meanwhile, we also hypothesized other possible reasons: (1) Allergic reaction of lidocaine. The prevalence of true IgE-mediated allergy to local anesthetics is estimated to be lower than 1%, immediate systemic hypersensitivity reaction (anaphylaxis) symptoms are observed in the first 30 min after the exposure to the anesthetic. Symptoms include dyspnea, cough, wheezing, hypotension and tachycardia, which are mostly inconsistent with our case; (2) Lidocaine overdose and poisoning. It occurs when the plasmatic level in the anesthetic rises to concentrations above the recommended amount. Although potentially severe, the systemic toxicity is extremely rare, and the patient’s present signs of central nervous system activation tend to progress to perioral paresthesia, facial paresthesia, dysarthria, metallic taste, diplopia, auditory disturbances and seizures. High blood pressure and tachycardia can also be associated with such activation[16]. In our case, 200 mg lidocaine is theoretically safe. Furthermore, symptoms presented in our patient were largely inconsistent; (3) Extensively abnormal spinal nerve block, defined as a complication of epidural anesthesia. It sometimes can be very difficult to differentiate. However, it generally takes longer to cause conscious instability, and it is generally feasible to identify the spine level being anesthetized through symptoms[17]. In our case this patient went to unconsciousness in a short time, and it was inapplicable to identify the anesthetized level; and (4) Anterior spinal artery syndrome. It is an extremely rare cause of acute ischemic cord infarction, which usually presents as an acute and painful myelopathy. Symptoms of our patient were inconsistent. It is generally caused by occlusion or hypoperfusion of the anterior spinal artery[18]. It might be caused by iatrogenic reasons, causing irreversible damage.
Fortunately, in our case, after about 15 min resuscitation, the patient started moving her legs and sensations came back again, with a blood pressure of 135/85 mmHg, pulse of 68 beats/min, respiration of 18/min and SpO2 of 96%. Therefore, anterior spinal artery syndrome was excluded, while intradural anesthesia leading to total spinal anesthesia was eventually confirmed.
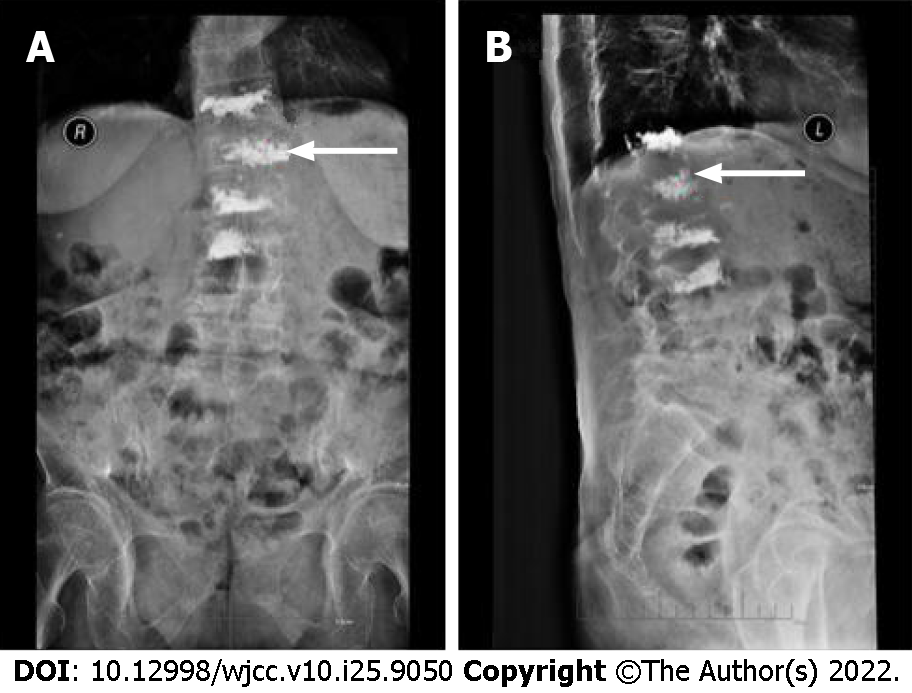
When the patient was stabilized (blood pressure: 135/85 mmHg, pulse: 68/min, respiration: 18/min, SpO2 96%) we decided to finish the surgery. We carefully and correctly reinserted the puncture needle. PVP was again safely and smoothly performed with 3.5 mL cement injected (Figure 2). The patient was sent back to the ward for monitoring. Significant pain relief was achieved postoperatively (visual analog scale: 2), and she was safely discharged on postoperative day 4. The patient recovered normally at the 3-mo follow-up.
Vertebral compression fracture is one of the most common complications of patients with osteoporosis. Conservative and nonoperative treatments like various analgesics, long-term bed rest, anti-osteoporotic medications, thoracolumbar bracing and other conventional therapies might be useful in acute fractures. Sometimes, patients with severe pain do not receive relief with conservative treatments. It is worthwhile to implement some aggressive or invasive procedures to reduce pain[19]. Among these invasive therapies, PVP and percutaneous kyphoplasty are commonly selected.
PVP is a minimally invasive procedure widely applied in patients with OVCF, vertebral angioma, tumors, etc. since it was first performed by Galibert et al[20] in 1987. Previous studies showed that PVP using local anesthesia can stabilize the spine, reduce pain and improve quality of life[21]. There are reported complications; however, to our knowledge, temporary paraplegia and unstable vital signs or total spinal anesthesia caused by local anesthetic drug leakage during PVP was never mentioned in the literature. Intradural anesthesia is more common in gynecology and obstetrics surgeries, which are mostly performed under epidural anesthesia[22].
Wu et al[14] reported two cases of intradural anesthesia during posterior percutaneous endoscopic cervical discectomy performed under local anesthesia. Albi-Feldzer et al[23] and Beyaz et al[24] reported total spinal anesthesia as a complication of thoracic paravertebral block. Dogan et al[25] reported total spinal anesthesia after lumbar plexus block. There were several reports of total spinal anesthesia after intercostal nerve block[26,27]. Similar to our case, Shi et al[15] analyzed 12 cases of total spinal anesthesia during percutaneous vertebral augmentation performed under local anesthesia. Conventionally, intradural anesthesia is usually seen spontaneously or as a complication in patients after medical procedures like lumbar puncture[28]. Common symptoms of intradural anesthesia include paraplegia, vomiting, decreased blood pressure, depressed respiration and arrhythmia, uncon
There are different diagnostic criteria of spontaneous intradural anesthesia. One of the most effective and direct ways is to observe the movement of the patient’s legs during the procedure. Confirmation of the needle placement using C-arm is also helpful in differentiating. Electrocardiogram monitoring plays an essential part in detecting abnormal conditions. As for treatment, once detected, surgery should be promptly ceased, and the patient should be monitored carefully. As demonstrated in our case, oxygen inhalation, fluid supplementation and most importantly resuscitation medicines like adrenaline, etc. were all implemented. If recovery does not occur, then we would have recommended cardiopulmonary resuscitation, endotracheal intubation and mechanical ventilation to sustain basic life signs.
One of the reasons increasing the chance of accidental subarachnoid injection of lidocaine is that our patient had a history of PVP procedure, which might induce pathological proliferation of granulation tissue and arachnoid abnormality around the target area. Fortunately, in our case, with a successful resuscitation, we decided to finish the surgery. We were more careful during local anesthesia in case of inadvertent wrong puncture and lidocaine leakage. PVP was again safely and smoothly performed. Significant pain relief was achieved postoperatively, and she was safely discharged on postoperative day 4. The patient recovered normally at the 3-mo follow-up.
Total spinal anesthesia secondary to PVP rarely occurs. In cases of inadvertent intradural anesthesia when performing it under local anesthesia, surgeons should be highly vigilant during the whole procedure. Electrocardiogram monitoring, oxygen inhalation, intravenous cannula set prior to surgery, regular checking of motor activity and meticulous imaging monitoring with slower pushing of anesthetics, etc. should be highly recommended.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Amornyotin S, Thailand; Nisi F, Italy; Singh A, India; Tsuchiya M, Japan S-Editor: Wang DM L-Editor: Filipodia P-Editor: Wang DM
| 1. | Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine (Phila Pa 1976). 2000;25:923-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 620] [Cited by in RCA: 504] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 2. | Qi L, Li C, Wang N, Lian H, Lian M, He B, Bao G. Efficacy of percutaneous vertebroplasty treatment of spinal tumors: A meta-analysis. Medicine (Baltimore). 2018;97:e9575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976). 2001;26:1511-1515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 821] [Cited by in RCA: 718] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 4. | Kobayashi K, Shimoyama K, Nakamura K, Murata K. Percutaneous vertebroplasty immediately relieves pain of osteoporotic vertebral compression fractures and prevents prolonged immobilization of patients. Eur Radiol. 2005;15:360-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 84] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Chen Y, Zhang H, Chen H, Ou Z, Fu Y, Zhang J. Comparison of the effectiveness and safety of unilateral and bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021;100:e28453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Dudeney S, Lieberman I. Percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures: an open prospective study. J Rheumatol. 2000;27:2526. [PubMed] |
| 7. | Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol. 1997;18:1897-1904. [PubMed] |
| 8. | Lee BJ, Lee SR, Yoo TY. Paraplegia as a complication of percutaneous vertebroplasty with polymethylmethacrylate: a case report. Spine (Phila Pa 1976). 2002;27:E419-E422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 173] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 9. | Naud R, Guinde J, Astoul P. Pulmonary cement embolism complicating percutaneous kyphoplasty: A case report. Respir Med Case Rep. 2020;31:101188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Kim SP, Son BS, Lee SK, Kim DH. Cardiac perforation due to intracardiac bone cement after percutaneous vertebroplasty. J Card Surg. 2014;29:499-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Laredo JD, Hamze B. Complications of percutaneous vertebroplasty and their prevention. Semin Ultrasound CT MR. 2005;26:65-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Puri AS, Colen RR, Reddy AS, Groff MW, DiNobile D, Killoran T, Nikolic B, Thomas AJ. Lumbar artery pseudoaneurysm after percutaneous vertebroplasty: a unique vascular complication. J Neurosurg Spine. 2011;14:296-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Kim MH, Lee AS, Min SH, Yoon SH. Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty. Asian Spine J. 2011;5:180-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Wu W, Yan Z. Intraoperative total spinal anesthesia as a complication of posterior percutaneous endoscopic cervical discectomy. Eur Spine J. 2018;27:431-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Shi G, Feng F, Hao C, Pu J, Li B, Tang H. An analysis of the causes of transient paraplegia during percutaneous vertebral augmentation under local anesthesia: A case series of 12 patients. J Orthop Surg (Hong Kong). 2019;27:2309499019861879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Cherobin ACFP, Tavares GT. Safety of local anesthetics. An Bras Dermatol. 2020;95:82-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 17. | Asfaw G, Eshetie A. A case of total spinal anesthesia. Int J Surg Case Rep. 2020;76:237-239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Peng T, Zhang ZF. Anterior Spinal Artery Syndrome in a Patient with Cervical Spondylosis Demonstrated by CT Angiography. Orthop Surg. 2019;11:1220-1223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | En X, Hao DJ. Percutaneous Kyphoplasty vs Conservative Treatment in Acute and Subacute Osteoporotic Vertebral Compression Fractures (OVCF): A Double-Blinded, Randomized Controlled Clinical Trial (RCT) in the Population of Western China. Spine J. 2013;13:S90-S91. |
| 20. | Galibert P, Deramond H, Rosat P, Le Gars D. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty]. Neurochirurgie. 1987;33:166-168. [PubMed] |
| 21. | Lamy O, Uebelhart B, Aubry-Rozier B. Risks and benefits of percutaneous vertebroplasty or kyphoplasty in the management of osteoporotic vertebral fractures. Osteoporos Int. 2014;25:807-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 22. | Ting HY, Tsui BC. Reversal of high spinal anesthesia with cerebrospinal lavage after inadvertent intrathecal injection of local anesthetic in an obstetric patient. Can J Anaesth. 2014;61:1004-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Albi-Feldzer A, Duceau B, Nguessom W, Jayr C. A severe complication after ultrasound-guided thoracic paravertebral block for breast cancer surgery: total spinal anaesthesia: A case report. Eur J Anaesthesiol. 2016;33:949-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Beyaz SG, Özocak H, Ergönenç T, Erdem AF, Palabıyık O. Total Spinal Block after Thoracic Paravertebral Block. Turk J Anaesthesiol Reanim. 2014;42:43-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Dogan Z, Bakan M, Idin K, Esen A, Uslu FB, Ozturk E. Total spinal block after lumbar plexus block: a case report. Braz J Anesthesiol. 2014;64:121-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Chaudhri BB, Macfie A, Kirk AJ. Inadvertent total spinal anesthesia after intercostal nerve block placement during lung resection. Ann Thorac Surg. 2009;88:283-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Friesen D, Robinson RH. Total spinal anesthesia--a complication of intercostal nerve block. Kans Med. 1987;88:84-96. [PubMed] |
| 28. | Jong D, Rudolph H. Lumbar puncture and spinal analgesia: intradural and extradural. JAMA. 1985;242:76-77. |
| 29. | Navarro JL, Soria A, Herrera P, Montero R. [Cauda equina syndrome after intradural anesthesia with bupivacaine]. Rev Esp Anestesiol Reanim. 2001;48:337-339. [PubMed] |