Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.9036
Peer-review started: March 26, 2022
First decision: April 13, 2022
Revised: April 22, 2022
Accepted: July 29, 2022
Article in press: July 29, 2022
Published online: September 6, 2022
Processing time: 152 Days and 20.4 Hours
Ochronotic arthropathy (OcA) is a rare disease, which is caused by the accumulation of homogentisic acid in the joint. Patients with OcA have obvious joint pain and the disease progresses rapidly, eventually resulting in disability. Arthroplasty is an efficacious treatment in patients with OcA. However, when OcA patients have joint infection, is joint replacement an option? In the present report, we performed total knee arthroplasty in a patient with OcA and knee infection under the guidance of one-stage revision theory.
A 64-year-old male was referred to our hospital due to severe left knee pain with limited mobility for 2 years. On physical examination, the patient was found to have dark brown pigmentation of the sclera and auricle. Laboratory test results showed elevations in C-reactive protein level (65.79 mg/L) and erythrocyte sedimentation rate (90.00 mm/h). The patient underwent debridement of the left knee joint, during which the cartilage surface of the knee joint was found to be black-brown in color. Bacterial culture of synovial fluid revealed Achromobacter xylosoxidans. We then carried out arthroplasty under the guidance of the theory of one-stage revision. After surgery, the patient's left knee joint pain disappeared and function recovered without joint infection.
OcA accompanied by joint infection is rare. One-stage revision arthroplasty may be a treatment option for this disease.
Core Tip: Ochronotic arthropathy (OcA) is a rare disease caused by the accumulation of homogentisic acid in the joint. Compared with general arthritis patients, patients with OcA have severe pain, poor function, and high disability rate. Arthroplasty is an effective treatment for patients with end-stage OcA. However, it is unknown how to select treatment when the OcA patient has joint infection. Under guidance of the one-stage revision theory, we treated a patient with OcA accompanied by knee infection with arthroplasty. Postoperation, the patient's knee joint pain disappeared and function recovered without joint infection. One-stage revision can be a treatment for this disease.
- Citation: Wang XC, Zhang XM, Cai WL, Li Z, Ma C, Liu YH, He QL, Yan TS, Cao XW. One-stage revision arthroplasty in a patient with ochronotic arthropathy accompanied by joint infection: A case report. World J Clin Cases 2022; 10(25): 9036-9043
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/9036.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.9036
Alkaptonuria (AKU) is a rare autosomal recessive hereditary metabolic disease[1], resulting from the absence of homogentisate 1,2-dioxygenase (HGD). HGD, an intermediate in the tyrosine degradation pathway, is responsible for the breakdown of homogentisic acid (HGA). As a result of this defect, a large amount of HGA cannot be metabolized normally and accumulates in the body over a long period, resulting in the formation of pigment-like polymers, which are deposited in connective tissue and cause ochronosis[2]. In patients with AKU, some HGA is excreted in the urine. Characteristically, excess HGA causes sufferers to pass dark urine, which upon standing turns black. Some HGA is also deposited in a variety of connective tissues, such as cartilage, sclera, and tendons, resulting in blue-black tissue changes, causing local lesions. Typically, the pigment is clearly seen in the sclera and auricle of patients. The disease usually progresses from simple AKU to alkaptonuric ochronosis and finally to ochronotic arthropathy (OcA)[3]. With advancing age, renal excretion of HGA decreases, and the accumulation of HGA gradually increases in the body. HGA can damage articular cartilage and cause joint degeneration, leading to OcA. The disease first affects the spine and then the peripheral joints. The patient’s symptoms usually begin around the third or fourth decade with low back pain and stiffness[4]. In the peripheral joints, the knee is most commonly involved, followed by the hip and shoulder[5]. OcA develops rapidly and tends to result in disability within a short time.
A literature review showed that arthroplasty in patients with OcA can be a good treatment choice[6]. However, arthroplasty for the treatment of OcA with joint infection has not been reported in the literature. Periprosthetic infection (PJI) is a catastrophic complication after arthroplasty, and two-stage exchange arthroplasty is the most common operation for patients with PJI[7]. However, the cost of this treatment is high[8,9], the mortality and morbidity rates are high, and the long-term function is poor[10]. A study found that by selecting appropriate patients and optimizing surgical procedures, one-stage exchange arthroplasty has significant benefits for patients with joint infection[11]. Zahar et al[12] found that the success rate of one-stage exchange arthroplasty was approximately 85%-90%. Based on the theory of one-stage revision, we treated a patient with OcA accompanied by knee infection with arthroplasty, and achieved satisfactory clinical results.
A 64-year-old man was admitted due to left knee pain and limited mobility.
The patient presented with left knee pain and limited mobility 2 years ago. He visited a local hospital several times and was diagnosed with left knee osteoarthritis. His left knee pain was only relieved by oral analgesics. His symptoms improved with medication, and relapsed when the analgesics were stopped. During the past 2 years, his symptoms gradually progressed. The patient was admitted to our department 4 mo prior with severe pain in the left knee and limited knee motion.
The patient had hypertension, but he did not take medicine regularly in the last month.
The patient had no relevant personal or family history.
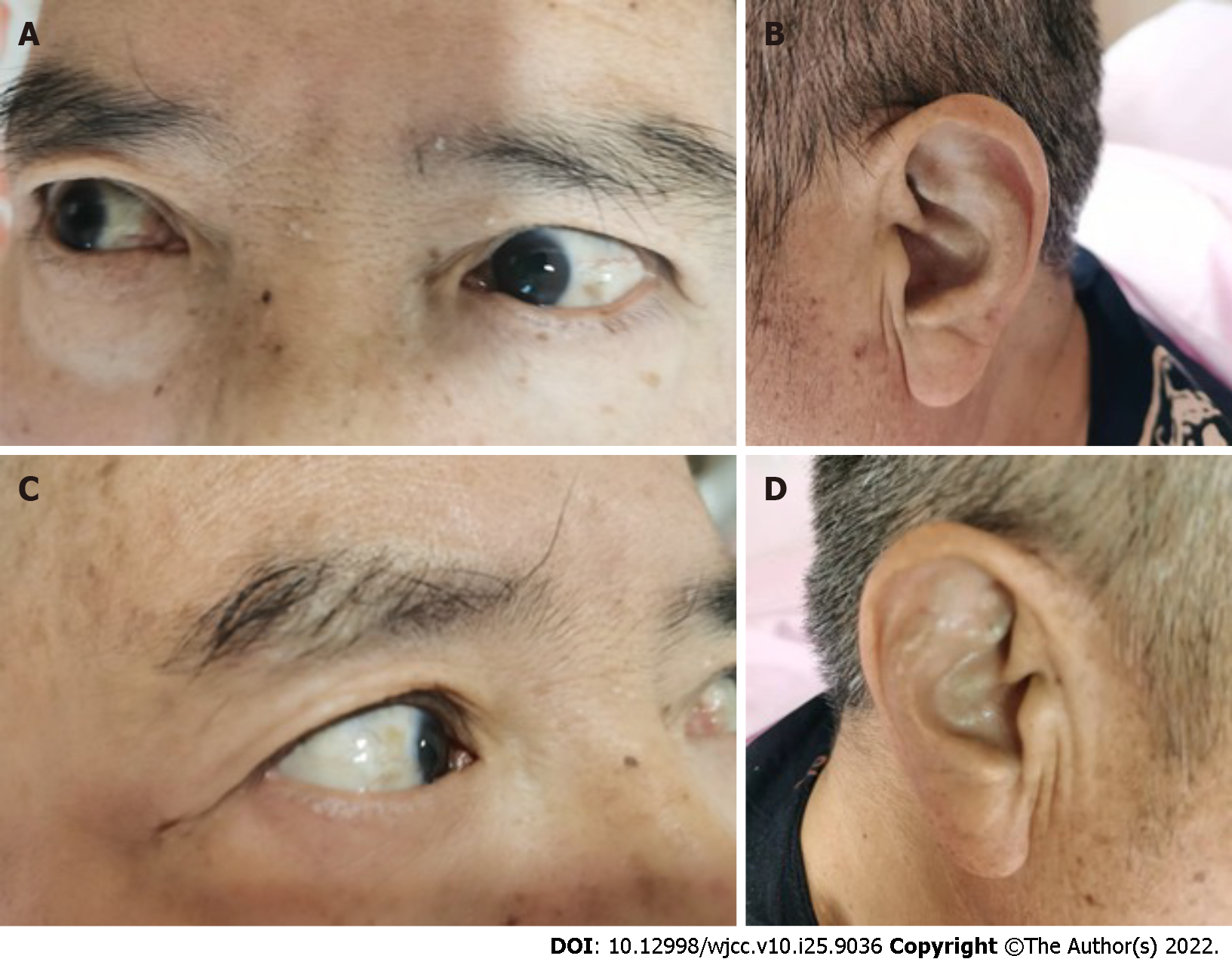
Dark-brown pigment was clearly seen in the sclera and ears of the patient (Figure 1). The patient's spine was stiff, and a major reduction in movement of the vertebral column was noted. Atrophy of the left quadriceps femoris and slight swelling of the left knee were observed. The left knee had a flexion contracture of 10°, and the range of motion of the left knee was 10° (extension) to 90° (flexion). The left knee patella grinding test and McMurray sign were positive.
Routine blood tests were normal and showed the following results: White blood cell count: 6.14 × 109/L; neutrophils: 63.9%; hemoglobin: 104 g/L; platelet count: 310 × 109/L. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were elevated at 65.79 mg/L and 90.00 mm/h, respectively.
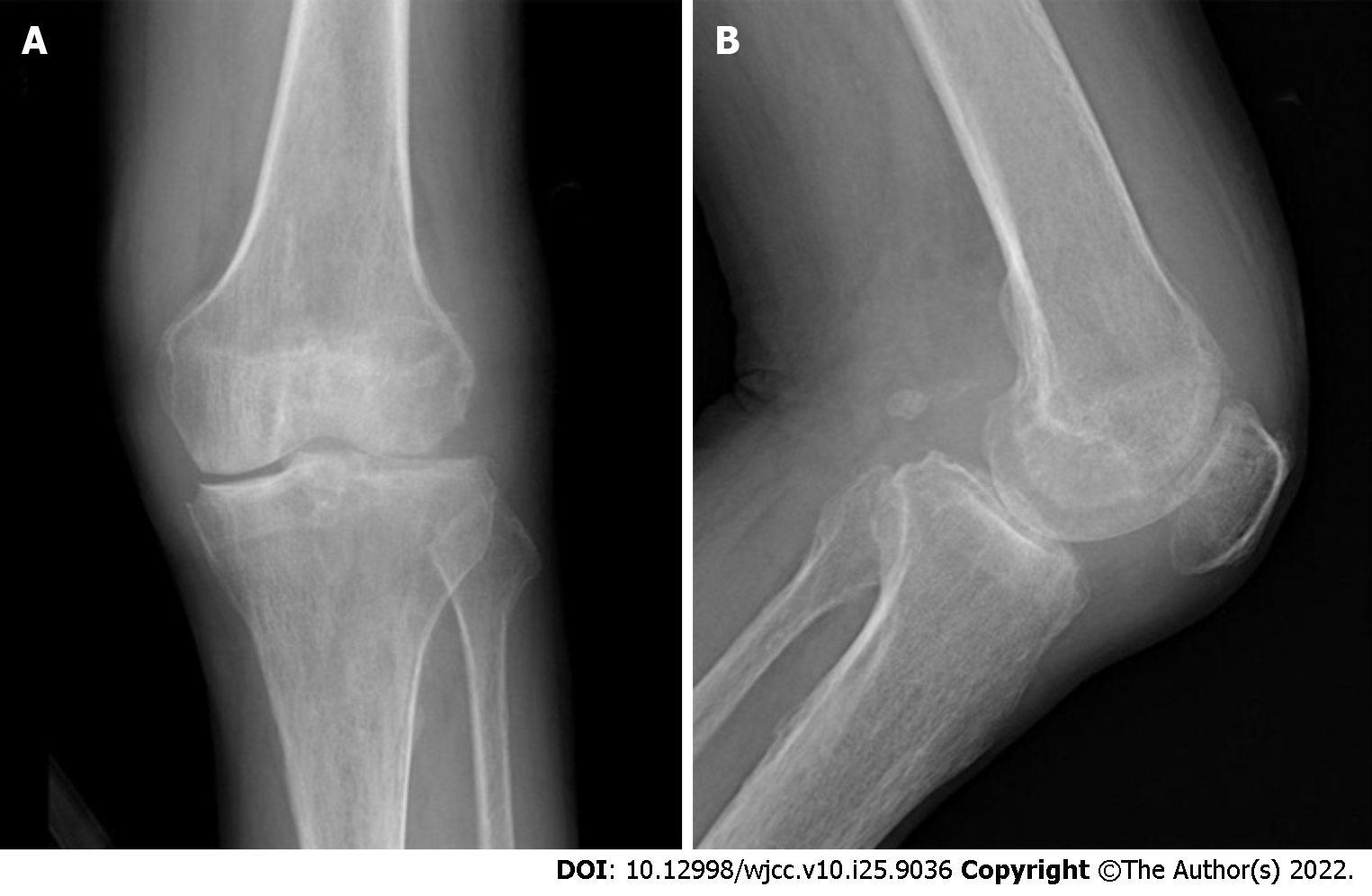
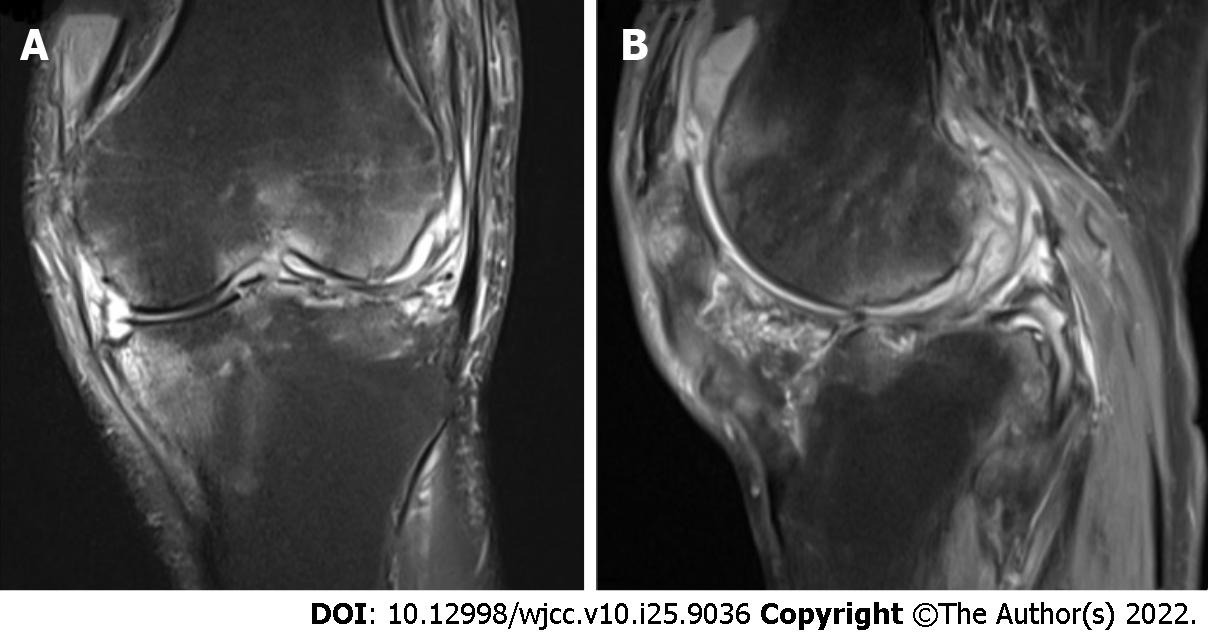
Radiographic evaluation revealed that the patient's left knee joint showed a similar appearance to that of osteoarthritis, such as joint space stenosis and osteophyte formation (Figure 2). Magnetic resonance imaging of the knee showed bone marrow edema (Figure 3).
We first carried out debridement of the left knee. During surgery, it was found that the cartilage of the knee joint was black-brown in color and there was a lot of synovial fluid in the joint cavity. We collected the synovial fluid for bacterial culture and the results showed the presence of Achromobacter xylosoxidans (A. xylosoxidans) in synovial fluid.
The final diagnosis in this patient was OcA and left knee infection.
We decided to carry out arthroplasty immediately under the guidance of the theory of one-stage revision. The patient underwent left cementless total knee replacement. During the operation, we found that all cartilage surfaces of the patient's left knee joint were black-brown (Figure 4), and a large amount of normal saline and iodophor were used to wash the joint cavity. Postoperatively, based on the results of bacterial culture, the patient received intravenous injections of ceftazidime and intrarticular injections of meropenem for 2 wk. This was followed by oral administration of sulfamethoxazole tablets and rifampicin for 4 wk.
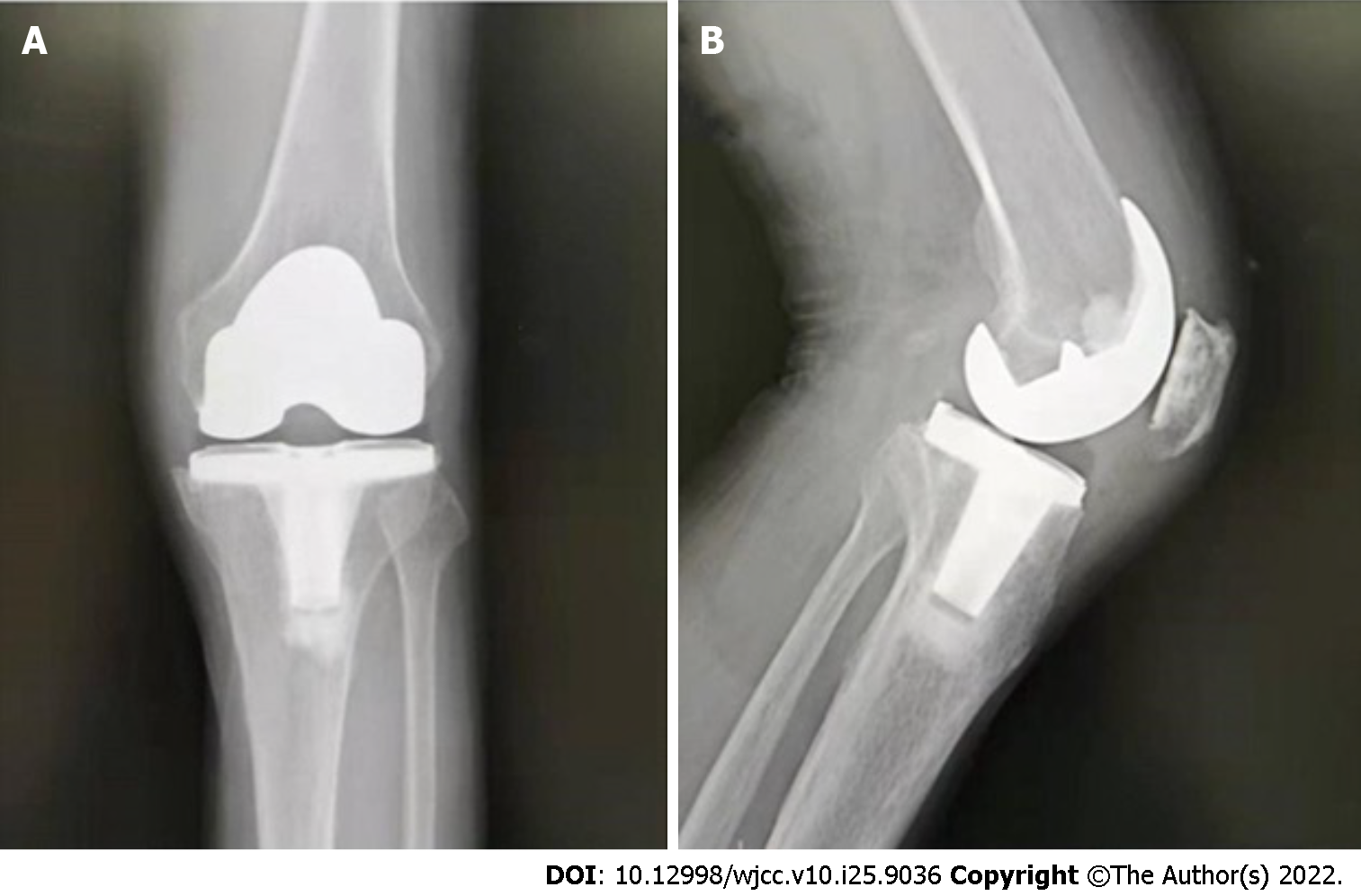
The patient's left knee pain was considerably relieved after surgery, and he was able to walk the day after surgery. One week postoperatively, the anteroposterior and lateral radiographs of the left knee joint showed that the prosthesis was in a good position (Figure 5). Routine blood tests, CRP and ESR were monitored after surgery. Both ESR and CRP decreased gradually, and eventually returned to normal. After 4 mo of postoperative follow-up, the patient's left knee joint function was normal without pain, and both ESR and CRP were normal.
AKU is an extremely rare disease that most clinicians have not seen before. The worldwide prevalence of AKU is 1 case in 250000-1000000 births[13]. It has three distinct clinical features: homogentisic aciduria, ochronosis, and ochronotic osteoarthropathy[14]. Patients initially have asymptomatic black urine, which has no significant impact on their life. They are usually over 40 years old when joint symptoms develop[15]. At this time, it is easy to misdiagnose OcA as osteoarthritis. The pathological changes due to knee osteoarthritis are characterized by degeneration of articular cartilage and periarticular hyperosteogeny. Inflammatory indicators such as ESR and CRP are generally normal. The main symptoms are knee pain and limited mobility. The pain is often dull, involving the whole knee or more localized, increases with joint use, and abates with rest[16]. Rheumatoid arthritis, which is a chronic, systemic inflammatory disease, frequently causes knee joint lesions. The most prominent feature is symmetric pain and swelling of the hands, wrists, feet, and knees (polyarthritis)[17]. Knee joint lesions are often accompanied by systemic symptoms such as low-grade fever, anemia, and weight loss.
Arthroplasty is an effective treatment in patients with OcA[18]. Ozmanevra et al[6] reviewed 13 studies on OcA. In the study, 21 cases of OcA were treated with arthroplasty, and achieved excellent clinical efficacy. However, no study has reported the use of arthroplasty in the treatment of patients with OcA and knee infection. A. xylosoxidans is a gram-negative aerobic bacterium that was first described in 1971[19]. This bacterium has been identified as the cause of meningitis, pneumonia, central catheter infection, sepsis, mediastinitis, and other diseases[20,21]. It was found in our patient's knee joint, which is rare. This species is drug-resistant and widely distributed in both indoor and outdoor environments, especially in humid areas[22]. Elderly people living at home can be affected by the bacterium. The patient's infection with A. xylosoxidans may have been related to living in an old neighborhood.
PJI is a common complication after joint replacement, which is difficult to treat. There are many surgical strategies for the treatment of PJI, including surgical debridement and retention of a prosthesis, one-stage exchange arthroplasty or two-stage exchange arthroplasty. One-stage exchange arthroplasty is a method used to treat patients with a joint infection. This method resolves the patient's problem with only one operation, avoiding a second operation. This surgical method has many advantages for patients, such as early walking, avoiding multiple surgical trauma, cost savings, and resuming daily life at an early date. In patients with OcA, not all have only joint degeneration, and inflammatory indicators such as ESR and CRP can also be elevated[23]. A study found that the production of HGA products may lead to the activation of inflammatory pathways in patients and an increase in inflammatory factors above normal levels[24]. Compared to patients with osteoarthritis, if examination results in OcA patients show increased inflammatory factors, then the possibility of infection is greatly increased. Our patient with OcA had left knee joint infection, and combined with the theory of one-stage revision, total knee arthroplasty was performed in this patient. Postoperative inflammatory indicators such as white blood cell count, ESR, and CRP decreased gradually, and finally returned to normal. At the patient's review 4 mo after surgery, we observed that the left knee joint incision had healed well, local skin temperature was normal, and the range of motion of the left knee joint was 0°-110°. In addition, pain in the left knee joint had disappeared.
In this case, the short-term effect after operation was satisfactory. However, the follow-up period was short, and additional long-term follow-up is needed to clarify the long-term efficacy of this treatment.
We report a patient who developed OcA and left knee joint infection. This disease is rare, but should not be overlooked by clinicians. It is easily misdiagnosed as osteoarthritis, but it has clinical manifestations different from arthritis. Under the guidance of the one-stage revision theory, we treated a patient with OcA accompanied by knee infection with arthroplasty, and achieved satisfactory clinical results. This approach can be applied in patients with OcA and joint infection.
We would like to appreciate our patient for consenting to have his case presented and published.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Al-Ani RM, Iraq; Tajiri K, Japan; Vyshka G, Albania S-Editor: Yan JP L-Editor: Filipodia P-Editor: Yan JP
| 1. | Ranganath LR, Cox TF. Natural history of alkaptonuria revisited: analyses based on scoring systems. J Inherit Metab Dis. 2011;34:1141-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Braconi D, Bernardini G, Bianchini C, Laschi M, Millucci L, Amato L, Tinti L, Serchi T, Chellini F, Spreafico A, Santucci A. Biochemical and proteomic characterization of alkaptonuric chondrocytes. J Cell Physiol. 2012;227:3333-3343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Zhao BH, Chen BC, Shao de C, Zhang Q. Osteoarthritis? Knee Surg Sports Traumatol Arthrosc. 2009;17:778-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Gómez-Lechón Quirós L, Hidalgo Calleja C, Acosta de la Vega ME, Compán Fernández O, Pastor Navarro S, Montilla Morales C. Family history of ochronotic arthropathy. Rheumatol Int. 2021;41:1869-1874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Gowda N, Kumar MJ, Kumar AK. Black hip: a rare case treated by total hip replacement. Ann Saudi Med. 2013;33:368-371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Ozmanevra R, Güran O, Karatosun V, Günal I. Total knee arthroplasty in ochronosis: a case report and critical review of the literature. Eklem Hastalik Cerrahisi. 2013;24:169-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA. Periprosthetic joint infection. Lancet. 2016;387:386-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 471] [Cited by in RCA: 623] [Article Influence: 69.2] [Reference Citation Analysis (0)] |
| 8. | Oduwole KO, Molony DC, Walls RJ, Bashir SP, Mulhall KJ. Increasing financial burden of revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2010;18:945-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 89] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 9. | Hernández-Vaquero D, Fernández-Fairen M, Torres A, Menzie AM, Fernández-Carreira JM, Murcia-Mazon A, Guerado E, Merzthal L. Treatment of periprosthetic infections: an economic analysis. ScientificWorldJournal. 2013;2013:821650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Haddad FS, Sukeik M, Alazzawi S. Is single-stage revision according to a strict protocol effective in treatment of chronic knee arthroplasty infections? Clin Orthop Relat Res. 2015;473:8-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 181] [Cited by in RCA: 157] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 11. | Nagra NS, Hamilton TW, Ganatra S, Murray DW, Pandit H. One-stage versus two-stage exchange arthroplasty for infected total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24:3106-3114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 92] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 12. | Zahar A, Webb J, Gehrke T, Kendoff D. One-stage exchange for prosthetic joint infection of the hip. Hip Int. 2015;25:301-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL, Anderson PD, Huizing M, Anikster Y, Gerber LH, Gahl WA. Natural history of alkaptonuria. N Engl J Med. 2002;347:2111-2121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 428] [Cited by in RCA: 390] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 14. | Mistry JB, Bukhari M, Taylor AM. Alkaptonuria. Rare Dis. 2013;1:e27475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | Demir S. Alkaptonuric ochronosis: a case with multiple joint replacement arthroplasties. Clin Rheumatol. 2003;22:437-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Sharma L. Osteoarthritis of the Knee. N Engl J Med. 2021;384:51-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 588] [Article Influence: 147.0] [Reference Citation Analysis (0)] |
| 17. | Sparks JA. Rheumatoid Arthritis. Ann Intern Med. 2019;170:ITC1-ITC16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 538] [Article Influence: 89.7] [Reference Citation Analysis (0)] |
| 18. | Karaoğlu S, Karaaslan F, Mermerkaya MU. Long-term result of arthroplasty in the treatment of a case of ochronotic arthropathy. Acta Orthop Traumatol Turc. 2016;50:584-586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Yabuuchi E, Oyama A. Achromobacter xylosoxidans n. sp. from human ear discharge. Jpn J Microbiol. 1971;15:477-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 108] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Kengni Tameze J, Korpak K, Compagnie M, Levie H, Cherifi S, Lali SE. Mitral endocarditis caused by Achromobacter xylosoxidans in an older patient: Case report and literature review. IDCases. 2022;27:e01421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Marion-Sanchez K, Lion F, Olive C, Cailleaux G, Roques F. Mediastinitis superinfected by Achromobacter xylosoxidans. A case report. J Infect Chemother. 2018;24:987-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Nakamoto S, Sakamoto M, Sugimura K, Honmura Y, Yamamoto Y, Goda N, Tamaki H, Burioka N. Environmental Distribution and Drug Susceptibility of Achromobacter Xylosoxidans Isolated from Outdoor and Indoor Environments. Yonago Acta Med. 2017;60:67-70. [PubMed] |
| 23. | Mannoni A, Selvi E, Lorenzini S, Giorgi M, Airó P, Cammelli D, Andreotti L, Marcolongo R, Porfirio B. Alkaptonuria, ochronosis, and ochronotic arthropathy. Semin Arthritis Rheum. 2004;33:239-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 62] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Yuce Inel T, Kisa PT, Balci A, Uslu S, Arslan Z, Hismi BO, Ucar U, Arslan N, Onen F, Sari I. Inflammatory rheumatic diseases in patients with ochronotic arthropathy. Mod Rheumatol. 2021;31:1031-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |