Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.8998
Peer-review started: March 13, 2022
First decision: April 8, 2022
Revised: April 13, 2022
Accepted: July 21, 2022
Article in press: July 21, 2022
Published online: September 6, 2022
Processing time: 166 Days and 3.4 Hours
Intradural cement leakage following percutaneous vertebroplasty is a rare but acute and devastating complication that usually requires emergent treatment. Here, we report a delayed complication of intradural leakage after percutaneous vertebroplasty.
A 71-year-old female patient with an L1 osteoporotic compression fracture underwent percutaneous vertebroplasty in 2014. She was referred to our hospital 5 years later due to complaints of progressive weakness and numbness in both legs combined with urinary incontinence and constipation. Initially, she was suspected to have a spinal meningioma at the level of L1 according to imaging examinations. Postoperative pathological tests confirmed that cement had leaked into the dura during the first percutaneous vertebroplasty.
Guideline adherence is essential to prevent cement from leaking into the spinal canal or even the dura. Once leakage occurs, urgent evaluation and decom
Core Tip: Intradural cement leakage following percutaneous vertebroplasty is a rare complication. Usually, it causes acute neurological deficit and require emergent decompression. Here presents a case who did not suffer acute neurologic impairment when cement leaked into intradural space, but gradually developed neurological symptom 5 years after the first vertebroplasty. This case highlights the ultimate importance of adherence to operation specification to avoid such complications.
- Citation: Ma QH, Liu GP, Sun Q, Li JG. Delayed complications of intradural cement leakage after percutaneous vertebroplasty: A case report . World J Clin Cases 2022; 10(25): 8998-9003
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/8998.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.8998
Percutaneous vertebroplasty is widely used for the treatment of osteoporotic vertebral compression fractures and certain pathological vertebral fractures, but it is not without complications, including adjacent fractures, radiculopathy, spinal cord compression, pulmonary embolism, infection and rib fractures, typically related to cement leakage[1]. Although most complications are asymptomatic or clinically insignificant, extravasation of cement into the dura can be disastrous. Fortunately, the rate of this complication is extremely low, with only 6 reported cases to date[2-7]. In all reported cases, the associated neurological deficits developed after vertebroplasty, and the patients lived with residual functional impairment even after timely decompression surgery. Usually, intradural cement leakage is an urgent condition requiring timely intervention. This report describes 1 case of delayed intradural leakage that occurred at another hospital; 5 years later, the patient was referred to us for further management.
A 71-year-old woman was referred to our hospital complaining of progressive weakness and numbness of both legs combined with urinary incontinence and constipation.
The patient’s symptoms started 2 mo before admission to our hospital. Initially she felt weak and numb of both legs. After taking medicine and rest, the symptoms did not relieve but progressively aggravated. In the last 2 wk, she could not stand and walk on her own. She also developed urinary incontinence and constipation at this time.
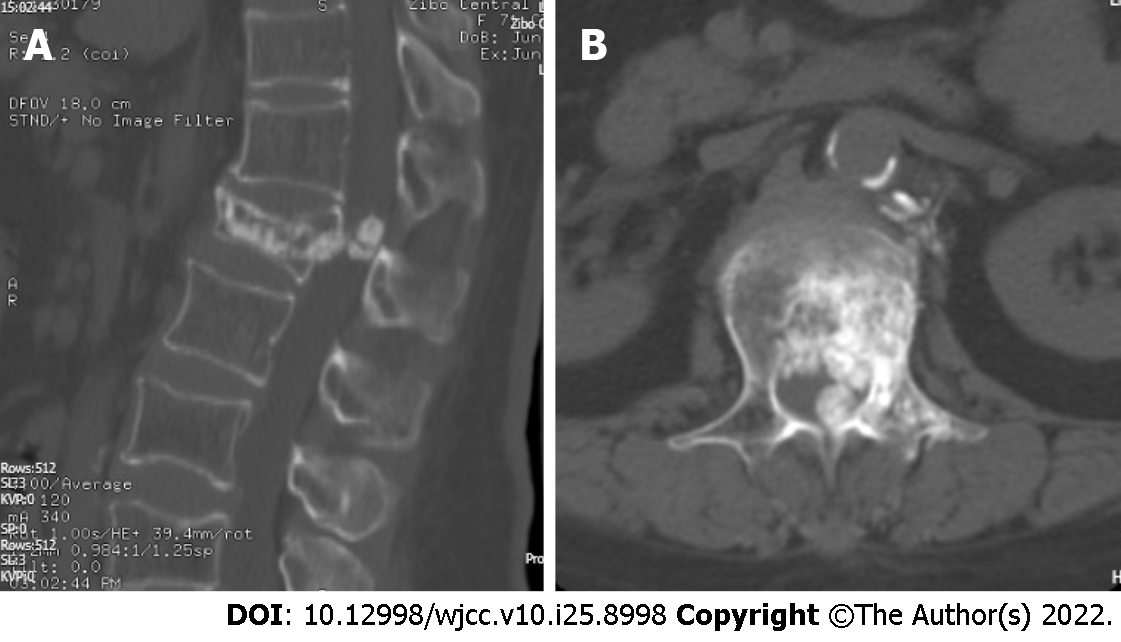
The patient underwent percutaneous vertebroplasty due to an L1 osteoporotic vertebral compression fracture at another hospital in 2014 (Figure 1).
The patient has no relevant family history.
Physical examination revealed atrophy of the left quadriceps, bilateral hypoesthesia below the level of the inguen, loose anal tone and diffuse weakness in both legs (grade 3).
Blood analysis, serum C-reactive protein, and urine analysis were normal.
X-ray imaging showed the L1 vertebroplasty with cement only on the left side of the vertebral body. Magnetic resonance imaging (MRI) demonstrated the presence of an intradural mass, which caused the majority of the cauda equina to deviate to the right (Figure 2). A computed tomography (CT) scan revealed calcification of the mass, which, however, was connected to the cement that had extravasated into the anterior space of the spinal canal (Figure 3). This abnormality led us to suspect that the intradural mass might be cement that leaked into the dura during the vertebroplasty procedure.
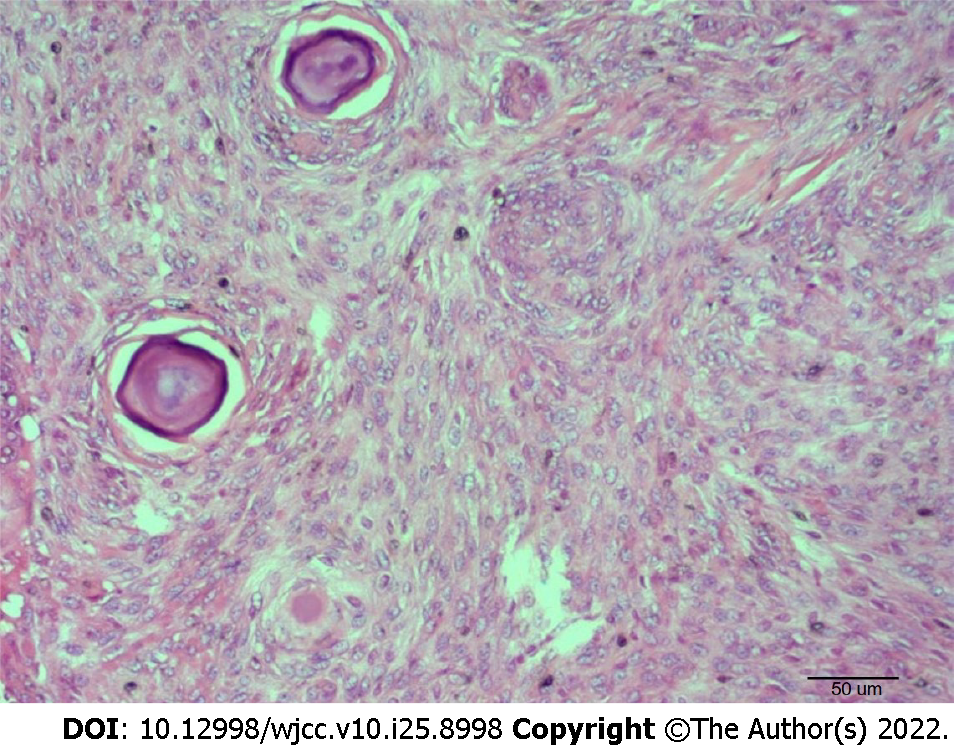
Pathologic examination proved our suspicion, showing focal chronic inflammatory cell infiltration on the cement surface (Figure 4).
L1 Laminectomy, mass resection and instrumentation from T11 to L3 with pedicle screws augmented with cement were performed. Upon inspection, the left lateral epidural space had adhered to the posterior wall of the vertebra. A midline durotomy was made. Two pieces of the intradural mass that had caused the majority of the cauda equina to deviate to the right were identified (Figure 5). Soft tissue-like scars covered the surface and had adhered to the arachnoid and nerve. A microscope was used to separate and resect the mass completely.
After the operation, the patient was referred to the rehabilitation department. After 2 years of follow-up, she began to walk with assistance. Her urinary incontinence improved but had not completely resolved.
It has been reported that the rate of cement leakage following vertebroplasty ranges from 38% to 87.9%[8]. Cement can leak into the paravertebral, intradiscal, epidural, foraminal and venous areas. A small amount of leakage is usually nonneurological and transitory, but large amounts may cause local or radicular pain and severe neurologic complications[9]. Leakage into the spinal canal is potentially associated with neurologic deficits. The most common location of intraspinal leakage is the epidural space. Epidural leaks may be more common than expected if careful postoperative CT is performed. Ryu et al[10] found leakage of cement into the epidural space in 40.3% of patients according to postoperative CT. However, cement leakage into the intradural space has rarely been reported. No cases of intradural cement leakage were reported during percutaneous vertebroplasty until 2003[2]. To date, only 6 incidents of intradural leakage have been described in the literature. The case presented here marks the seventh. The essential condition underlying this rare complication is rupture of the dura. Typically, cement leakage occurs through the basivertebral plexus, bone defect or posterior wall of the vertebra into the epidural space. If the dura, cement can subsequently extravasate into the subdural area through the perforation. This complication could be explained by medial wall perforation and dura penetration during needle insertion through the pedicle, especially when a unilateral approach is used[5,7]. To avoid this technical error, the needle tip should not cross the medial border of the pedicle on the anteroposterior view before it has reached the posterior cortex of the vertebral body on the lateral view[4,7]. Surgical expertise should be emphasized to decrease the risk of cement leakage into the spinal canal. First, adequate opacification of the cement enables immediate monitoring of the distribution by fluoroscopy[3]. In the present case, the cement was not sufficiently radiopaque and may have been injected in liquid mobile form, making it difficult to detect leakage into the spinal channel. Second, from our experience, cement should be injected into the anterior 2/3 of the vertebral body and must be stopped when flow of cement into the posterior 1/3 of the vertebral body is observed. Zhang et al[11] suggested that cement should not reach the posterior 1/6 of the body in the middle and lower thoracic regions because of the concave structure of the posterior wall of this region. In the literature, all patients with leakage into the dura undoubtedly developed varying degrees of neurologic deficits in the lower extremities and urinary and stool disturbances. Fortunately, they all received timely decompression surgery, except for one patient due to poor physical condition. This is the only case in which salvage surgery was delayed for an extended period. Once new-onset neurologic deficits occur during the procedure, immediate surgical removal of the cement should be considered. Surgery under local, rather than general, anesthesia has been recommended for the early detection of neurologic compromise during the procedure[12]. Direct mass effects and thermal injury are the main causes of neurological deficits[4,6,13]. Early surgery probably improves new-onset neurological deficits and is not difficult to perform. If surgery is delayed, it becomes difficult to remove the cement due to adhesions caused by the late thermal effect of chronic inflammation and fibrosis, which may cause further damage to the nerve. In the present case, the gross surgical and microscopic findings of fibrosis and adhesion on the cement surface were indicative of the delayed effects of the thermal injury.
To increase safety, surgery should be performed by well-trained, experienced surgeons. Good quality image monitoring, clear visualization of the cement, avoidance of a medial wall breach and cessation of injection once the cement reaches the posterior one-third of the vertebral body are recommended. Prompt CT or MRI exploration and urgent surgical decompression are necessary if cement leakage is detected due to neurological deficits that develop during the procedure.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Darbari A, India; Ghannam WM, Egypt; Lin X, China S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Hu KZ, Chen SC, Xu L. Comparison of percutaneous balloon dilation kyphoplasty and percutaneous vertebroplasty in treatment for thoracolumbar vertebral compression fractures. Eur Rev Med Pharmacol Sci. 2018;22:96-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 2. | Shapiro S, Abel T, Purvines S. Surgical removal of epidural and intradural polymethylmethacrylate extravasation complicating percutaneous vertebroplasty for an osteoporotic lumbar compression fracture. Case report. J Neurosurg. 2003;98:90-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Chen YJ, Tan TS, Chen WH, Chen CC, Lee TS. Intradural cement leakage: a devastatingly rare complication of vertebroplasty. Spine (Phila Pa 1976). 2006;31:E379-E382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Teng MM, Cheng H, Ho DM, Chang CY. Intraspinal leakage of bone cement after vertebroplasty: a report of 3 cases. AJNR Am J Neuroradiol. 2006;27:224-229. [PubMed] |
| 5. | Sabuncuoğlu H, Dinçer D, Güçlü B, Erdoğan E, Hatipoğlu HG, Ozdoğan S, Timurkaynak E. Intradural cement leakage: a rare complication of percutaneous vertebroplasty. Acta Neurochir (Wien). 2008;150:811-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Kulkarni AG, Shah SP, Deopujari CE. Epidural and intradural cement leakage following percutaneous vertebroplasty: a case report. J Orthop Surg (Hong Kong). 2013;21:365-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Lin BJ, Li CC, Ma HI. Intradural Cement Leakage After Percutaneous Vertebroplasty. Turk Neurosurg. 2015;25:940-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Wang B, Zhao CP, Song LX, Zhu L. Balloon kyphoplasty versus percutaneous vertebroplasty for osteoporotic vertebral compression fracture: a meta-analysis and systematic review. J Orthop Surg Res. 2018;13:264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 85] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 9. | Cosar M, Sasani M, Oktenoglu T, Kaner T, Ercelen O, Kose KC, Ozer AF. The major complications of transpedicular vertebroplasty. J Neurosurg Spine. 2009;11:607-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Ryu KS, Park CK, Kim MC, Kang JK. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg. 2002;96:56-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 84] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Zhang S, Wang GJ, Wang Q, Yang J, Xu S, Yang CH. A mysterious risk factor for bone cement leakage into the spinal canal through the Batson vein during percutaneous kyphoplasty: a case control study. BMC Musculoskelet Disord. 2019;20:423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Harrington KD. Major neurological complications following percutaneous vertebroplasty with polymethylmethacrylate : a case report. J Bone Joint Surg Am. 2001;83:1070-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 172] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 13. | Verlaan JJ, Oner FC. Re: Belkoff SM, Molloy S. Temperature measurement during polymerization of polymethyl methacrylate cement used for vertebroplasty. Spine. 2003; 28:1555-9. Spine (Phila Pa 1976). 2004;29:1161; author reply 1161-1161; author reply 1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |