Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.8968
Peer-review started: February 6, 2022
First decision: April 10, 2022
Revised: April 19, 2022
Accepted: July 20, 2022
Article in press: July 20, 2022
Published online: September 6, 2022
Processing time: 200 Days and 17.4 Hours
Gallstone disease (GD) can have prolonged, subacute inflammatory period before biliary events. The intricate relationship between GD and inflammatory processes can possible lead to prothrombotic tendency that can result in confusing clinical course before diagnosis.
A 51-year-old man, presented with a 1-year history of self-relief occasional postprandial upper abdominal pain, had sudden onset severe left upper quadrant pain and visited our emergency room. Contrast enhanced computed tomography (CECT) showed filling defect in celiac trunk, common hepatic, part of splenic arteries and wedge-shaped hypo-enhancing region of spleen, consistent with splenic infarction secondary to splenic arterial occlusion. No convincing predisposing factors were found during first hospitalization. Abdominal pain mildly subsided after low molecular weight heparin and bridge to oral anticoagulant use. However, in the following six months, the patient was admitted twice due to acute cholangitis and finally cholecystitis. Second CECT revealed biliary impacted stone was adjacent to poor dissoluble thrombus. The abdominal pain did not achieve a clinical full remission until endoscopic retrograde cholangiopancreatography stone removal and series laparoscopic cholecystectomy was performed.
This is the first case to present serious thrombotic complication due to inflammation status in chronic GD. It could be a rare, confusing and difficult recognizing cause of a celiac trunk thro
Core Tip: We present a case of a gallstone-associated thromboembolic event and highlight the clinical course with difficulty of recognizing the predisposing factor. Recent studies have shown a bidirectional relationship between inflammation and perturbation of the coagulation process. This case highlights that gallstone-related local inflammation, even asymptomatic, can cause serious thromboembolic complications.
- Citation: Wu CY, Su CC, Huang HH, Wang YT, Wang CC. Gallstone associated celiac trunk thromboembolisms complicated with splenic infarction: A case report. World J Clin Cases 2022; 10(25): 8968-8973
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/8968.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.8968
Celiac trunk thromboembolisms complicated with splenic infarction is an uncommon clinical entity associated with variable symptoms and signs. In previous case studies, missed diagnosis or misdiagnosis are common if base on only clinical clues and etiology[1]. However, currently availability of contrast enhanced computed tomography (CECT) scanning poses an appropriate instrumental for diagnosis of splenic infarction, comparing to abdominal sonography[2]. It is well advised for clinicians to consider possible underlying etiology when dealing with splenic infarction.
Gallstone disease (GD) is reported higher in Western (10% in America, 6%–19.5% in European) and lower in Asia (2.3%-5.4%)[3]. Recently, GD has been proved associated with cardiovascular diseases[4], thromboembolic venous disease, including deep vein thrombosis and pulmonary embolism[5].
To our knowledge, this is the first case to highlights that a thromboembolic event without evident predisposing risk should be consider as a prothrombotic tendency due to inflammation status in chronic calculous biliary events with a high clinical consequence.
A 51-year-old man had sudden onset, severe left upper quadrant pain accompanied with cold sweating and nausea.
The patient had a 1-year history of intermittent postprandial pain over upper quadrant abdomen, which can subside itself, without seeking medical treatment before this admission. He suffered from sudden onset, severe left upper quadrant abdominal pain radiating to the epigastrium was accompanied with cold sweating and nausea. Initially he came to our outpatient department for help. However, due to intolerable pain and hypertension urgency, he was referred to our emergency department for immediate management. He denied fever, cough, dyspnea, weight loss, recent bowel habit change nor urinary symptoms.
The patient had hypertension for more than ten years under regular medication control.
The patient drink beer occasionally without addiction. He also smokes one pack per day for over 30 years. There was no remarkable family medical history.
At emergency department, he was apyrexial with a temperature of 36.0 °C, hypertensive with a blood pressure of 176/109 mmHg and a pulse of 85 beats/min. There were local tenderness and muscle guarding over the left upper quadrant of abdomen without rebounding tenderness.
Laboratory investigations showed Hb of 16.4 g/dL (n = 13–17 g/dL), white blood cell count of 12.64 × 109/L (n = 4–11 × 109/L) and a platelet count of 251 × 103/L (n = 150–400 × 103/L). Inflammatory markers elevated with a C-reactive protein of 1.36 mg/dL (UNL = 0.748 mg/dL). Serum alanine aminotransferase 40 IU/L (n = 10-40 IU/L), total bilirubin, 0.90 mg/dL. However D-dimer levels (2737.72 ng/mL, UNL= 500 ng/mL) were much elevated.
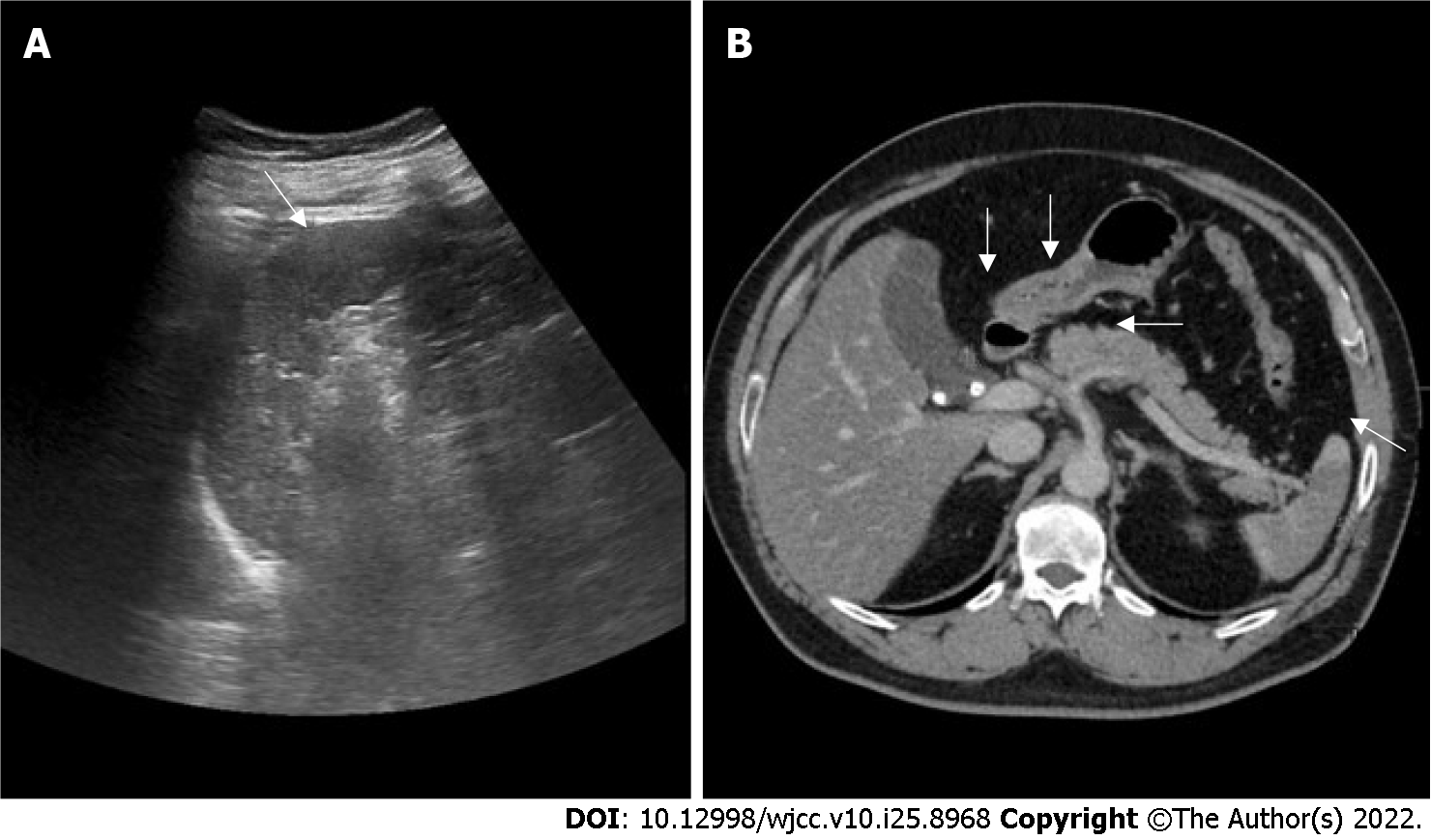
Abdominal ultrasound showed a hypoechoic area of spleen. CECT revealed filling defects in celiac trunk, common hepatic and part of splenic arteries along with fat stranding. Wedge-shaped low density region of spleen consistent with standard pattern of splenic infarction suggesting secondary to splenic artery occlusion. The hyperdense gallstone and cystic duct stone are also visualized at CT without biliary tract dilatation (Figure 1).
The final diagnosis of the presented case is gallstone disease associated celiac trunk thromboembolism complicated with splenic infarction.
Low molecular weight heparin (enoxaparin) 6000 IU per 12 h was given. After 3 d of administration, according to hematology and rheumatologist on board, with improved symptoms and lack of predisposing risk factors, we switched to non-vitamin. K antagonist oral-anticoagulant (NOAC) - Apixaban 5 mg twice daily and continued after discharge.
After discharged, he had been regular followed up in our gastroenterology outpatient department on a monthly basis. During his follow-up period, he complained only acid regurgitation sensation accompanied with mild epigastric bloating.
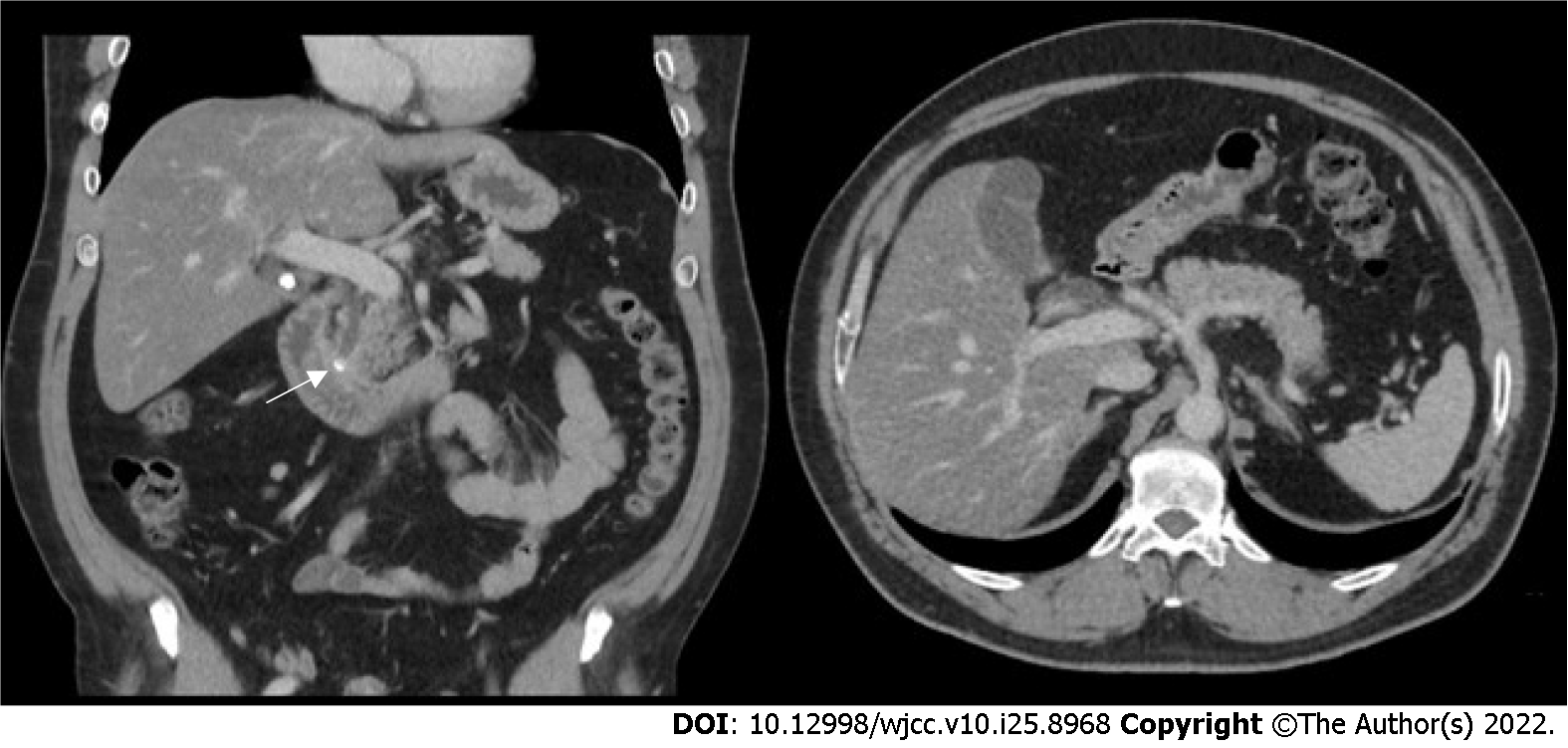
Six weeks later, the patient was re-admitted due to another episode of severe abdominal pain for three days associated with post-prandial vomiting. There were icteric sclera and tenderness over right upper quadrant of abdomen. Laboratory data at emergency room showed elevated biliary enzymes, such as serum aspartate transferase, alanine transaminase, r-GT, alkaline phosphatase, and total bilirubin level. Cystic duct stone become lodged in the lower common bile duct and return homogenous contrast enhancement of splenic parenchyma at following CT scan (Figure 2). Acute cholangitis was diagnosed therefore endoscopic retrograde cholangiopancreatography stone removal was achieved smoothly and the episode of cholangitis resolved in the second hospital course. He refused interval cholecystectomy (CCY) initially, but refractory biliary event happened. Not until after laparoscopic CCY did the patient achieve a clinical full remission.
Splenic infarction is a relatively uncommon diagnosis. Symptoms can represent with left upper quadrant pain, left flank pain, nausea, fever or even asymptomatic. Predisposing etiology including atherosclerosis, emboli (either cardiogenic or from aortic plagues), hematological disorders, and autoimmune disease (antiphospholipid syndrome, vasculitis, etc.)[2,6]. In our case, however, during first evaluation in hospitalization, we did not observe any convincing predisposing factor that could possibility results in extensive thrombus causing a splenic infraction. Until the following admissions, GD related thrombotic event gained our concern.
In previous studies, over 80% of patients with gallstones remain asymptomatic[7] and symptomatic biliary complications include cholecystitis, cholangitis and even biliary tract cancers. However numerous epidemiological studies demonstrated that even asymptomatic gallstones increase risk of stroke[8], cardiovascular disease[4,9] and thromboembolic venous disease[5]. Although, vascular disease shared common risk factor with biliary events, such as high fat diet, obesity, diabetes mellitus and age, most studies still present significant correlation after adjusted for these common risk factors. Two studies using nationwide population base studies in Taiwan even showed higher risk among younger GD patients[8,9], who shared less risk factors of cardiovascular disease.
Tracing back to the patient’s history, there was intermittent mild epigastric discomfort for a year. Besides, the time interval between thrombosis formation and the following refractory GD raised our concern. Compatible to clinical symptoms and hospital course, chronic biliary events may serve as a cause of local inflammation which was masked by thromboembolic event. The symptoms were not fully resolved and further lead to cholangitis and finally cholecystitis in the following 6 months. The patient had no other predisposing factors and after CCY, the patient is finally symptom free on following examination after discontinue NOAC treatment.
Local inflammation was not first recognized as a predisposing factor for thrombus formation.
Recent studies already demonstrated a bidirectional relationship between local or systematic inflammation[10] which is an intricately related processes. In molecular analysis, chronic calculous cho
Perivascular inflammation can develop secondary to trauma or inflammation due to adjacent local inflammatory reaction, causing thrombosis of vasa vasorum with pseudo-aneurysms formation or true artery aneurysms[13]. Gallbladder with gallstones also showed increase oxidative stress[14] which plays a role in the pathogenesis of abnormal coagulation and impaired vasodilatation[15].
Despite biliary events being common, the rarity of splenic infarction can only be explained by a prolonged inflammatory process without acute cholecystitis or cholangitis in our case. Ours is the first report of a case of GD associated thromboembolic event in celiac trunk, which induced splenic infarction. Taken all together, GD should be considered as a risk factor of celiac trunk thrombosis or spleen infarction by future clinicians if no prothrombotic tendency nor cardiac risk were found. Further scientific evidence worth large-scaled study confirmation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: The Gastroenterological Society of Taiwan.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mishra TS, India; Moshref L, Saudi Arabia S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Li Y, Liu H, Shi Y. Splenic infarction associated with obstructive sleep apnoea/hypopnoea syndrome: a case report. J Int Med Res. 2020;48:300060520954691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Schattner A, Adi M, Kitroser E, Klepfish A. Acute Splenic Infarction at an Academic General Hospital Over 10 Years: Presentation, Etiology, and Outcome. Medicine (Baltimore). 2015;94:e1363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Chen CH, Huang MH, Yang JC, Nien CK, Etheredge GD, Yang CC, Yeh YH, Wu HS, Chou DA, Yueh SK. Prevalence and risk factors of gallstone disease in an adult population of Taiwan: an epidemiological survey. J Gastroenterol Hepatol. 2006;21:1737-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 117] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 4. | Fan LL, Chen BH, Dai ZJ. The relation between gallstone disease and cardiovascular disease. Sci Rep. 2017;7:15104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Chen CH, Lin CL, Kao CH. The Risk of Venous Thromboembolism in Patients with Gallstones. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Wand O, Tayer-Shifman OE, Khoury S, Hershko AY. A practical approach to infarction of the spleen as a rare manifestation of multiple common diseases. Ann Med. 2018;50:494-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Friedman GD. Natural history of asymptomatic and symptomatic gallstones. Am J Surg. 1993;165:399-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 251] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Wei CY, Chung TC, Chen CH, Lin CC, Sung FC, Chung WT, Kung WM, Hsu CY, Yeh YH. Gallstone disease and the risk of stroke: a nationwide population-based study. J Stroke Cerebrovasc Dis. 2014;23:1813-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Olaiya MT, Chiou HY, Jeng JS, Lien LM, Hsieh FI. Significantly increased risk of cardiovascular disease among patients with gallstone disease: a population-based cohort study. PLoS One. 2013;8:e76448. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Levi M, van der Poll T, Büller HR. Bidirectional relation between inflammation and coagulation. Circulation. 2004;109:2698-2704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 637] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 11. | Levi M, van der Poll T, ten Cate H, van Deventer SJ. The cytokine-mediated imbalance between coagulant and anticoagulant mechanisms in sepsis and endotoxaemia. Eur J Clin Invest. 1997;27:3-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 208] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 12. | Kasprzak A, Szmyt M, Malkowski W, Przybyszewska W, Helak-Łapaj C, Seraszek-Jaros A, Surdacka A, Małkowska-Lanzafame A, Kaczmarek E. Analysis of immunohistochemical expression of proinflammatory cytokines (IL-1α, IL-6, and TNF-α) in gallbladder mucosa: comparative study in acute and chronic calculous cholecystitis. Folia Morphol (Warsz). 2015;74:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Kulkarni V, Deshmukh H, Gupta R. Pseudoaneurysm of anomalous cystic artery due to calculous cholecystitis. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Geetha A. Evidence for oxidative stress in the gall bladder mucosa of gall stone patients. J Biochem Mol Biol Biophys. 2002;6:427-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Saghazadeh A, Hafizi S, Rezaei N. Inflammation in venous thromboembolism: Cause or consequence? Int Immunopharmacol. 2015;28:655-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 93] [Article Influence: 9.3] [Reference Citation Analysis (0)] |