Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.8939
Peer-review started: October 7, 2021
First decision: January 11, 2022
Revised: January 24, 2022
Accepted: July 24, 2022
Article in press: July 24, 2022
Published online: September 6, 2022
Processing time: 323 Days and 3.7 Hours
Post-polypectomy electrocoagulation syndrome (PPES) can occur after colonoscopic polypectomy and is usually treated conservatively with a positive prognosis. Nevertheless, there can be cases with complications developing.
A 58-year-old woman, who had no previous medical history, visited the Emergency Department of another hospital with symptoms of abdominal pain and fever, 1 d after multiple colonoscopic polypectomies. An abdominopelvic computed tomography (CT) scan demonstrated colo-colonic intussusception, and she was transferred to our hospital to consider an operation. CT showed colo-colonic intussusception with PPES and no evidence of obstruction. The physical examination showed localized mild tenderness on the right sided abdomen. The patient fasted and was admitted for treatment with intravenous antibiotics (piperacillin/tazobactam 4.5 g each 8 h, ornidazole 500 mg each 12 h). After admission, the symptoms got better and a follow-up CT scan demonstrated resolution of the PPES and intussusception. The patient was discharged on hospital day 9.
Colo-colic intussusception can occur with PPES, and it can be properly treated conservatively.
Core Tip: Post-polypectomy electrocoagulation syndrome (PPES) can occur after colonoscopic poly
- Citation: Moon JY, Lee MR, Yim SK, Ha GW. Colo-colonic intussusception with post-polypectomy electrocoagulation syndrome: A case report. World J Clin Cases 2022; 10(25): 8939-8944
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/8939.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.8939
Colonoscopy is the golden standard for colorectal cancer screening. Polypectomies performed during colonoscopies are generally safe. Post-polypectomy electrocoagulation syndrome (PPES) is an infrequent complication after endoscopic polypectomy. PPES is additionally an electrocoagulation injury of the colonic wall that causes a transmural burn and localized peritonitis[1]. Patients with PPES can develop abdominal pain and/or signs of peritoneal irritations, fever, and leukocytosis, which are like bowel perforation; however, no perforation was seen on imaging study of the abdomen[2-5]. Most cases of PPES are associated with a good prognosis. Patients with less severe symptoms can be treated on an outpatient basis and rarely develop advanced complications[6-8].
A 58-year-old woman visited the Emergency Department of another hospital with abdominal pain and fever. Her abdominopelvic computed tomography (CT) scan demonstrated colo-colonic intussusception, and she was transferred to our hospital for considering an operation.
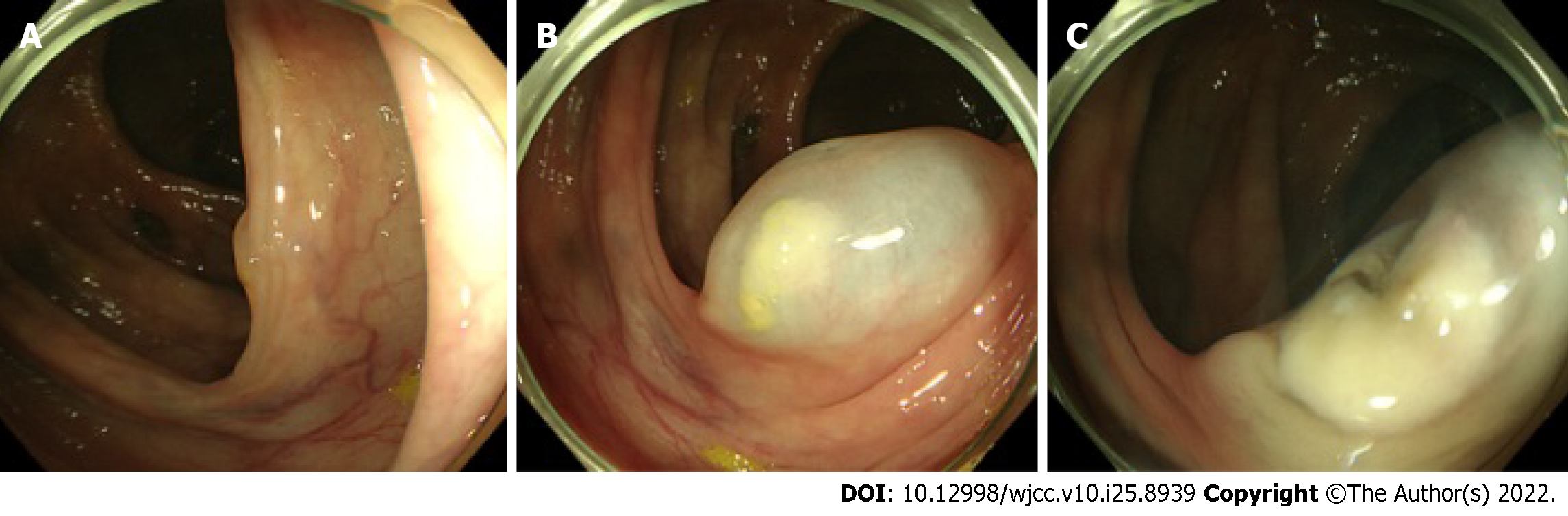
The patient had multiple colonoscopic polypectomies in the right sided colon, especially in the hepatic flexure colon. A polyp was lifted by submucosal saline injection, a polypectomy was done by electrocoagulation polypectomy (Figure 1) at another hospital 1 d before admittance, and symptoms started that night.
The patient had no medical history.
The patient had no personal and family history.
The body temperature was 38 °C, heart rate was 70 bpm, respiratory rate was 20 breaths per minute, and blood pressure was 123/76 mmHg. The abdominal physical examination of the patient showed mild tenderness in the abdomen on the right side.
Routine laboratory data demonstrated an elevated white blood cell count (11.84 × 103/L) with a predominance of neutrophils (83%). The erythrocyte sedimentation rate was normal at 10 mm/h, and the serum C-reactive protein was elevated at 66.18 mg/L. The blood biochemistries were normal.
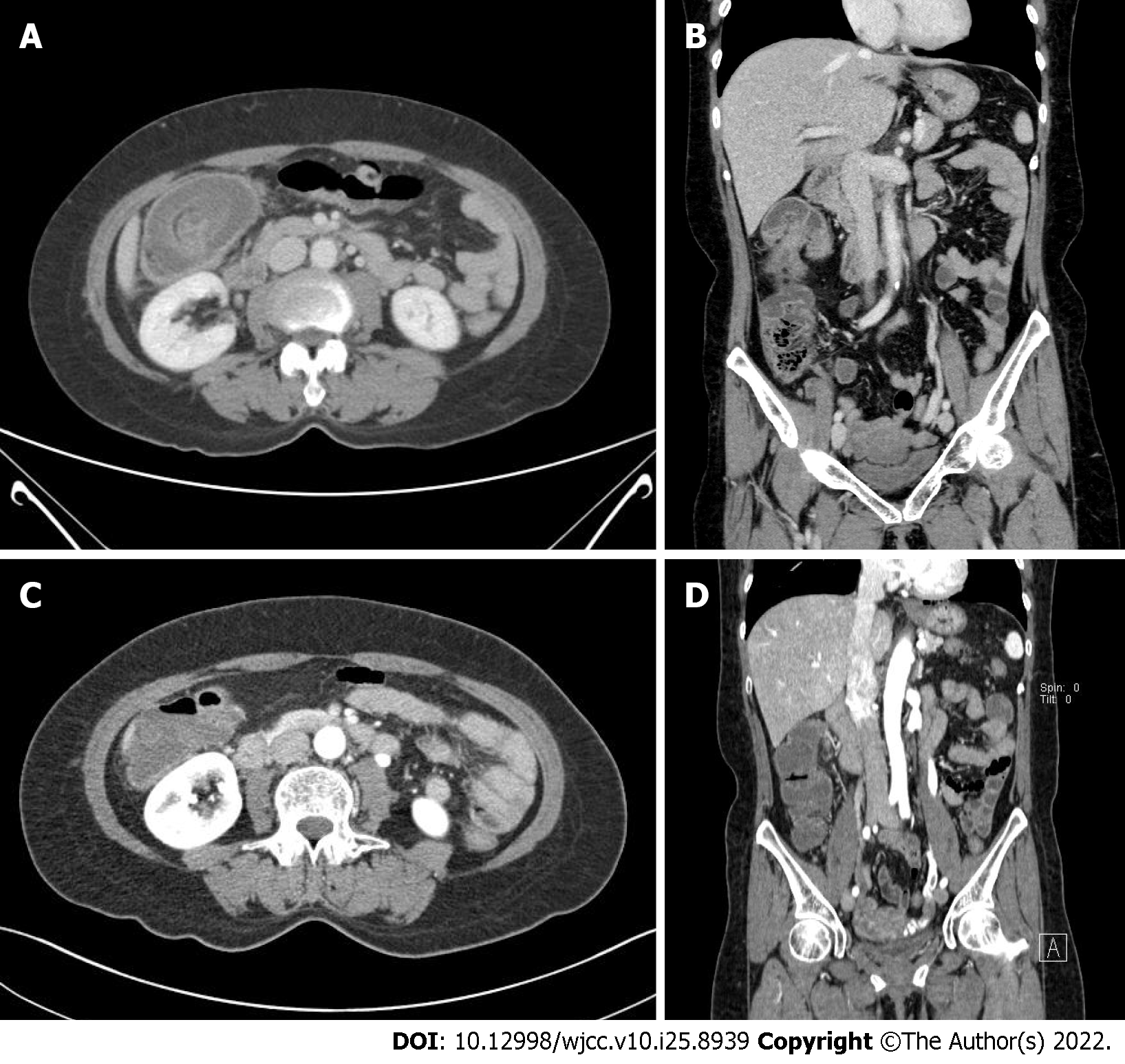
An initial imaging evaluation by abdominopelvic CT revealed a target-like lesion in the right-side colon with bowel and fatty mesentery inside, which indicated colo-colonic intussusception. The lesion and proximal colon showed wall thickening with submucosal swelling and highly attenuated infiltration of adjacent pericolic fat. A transmural air bubble was in the wall of a lesion. There was no definite leading point (Figure 2A and B).
The colon lesion was further evaluated by abdominopelvic CT at hospital day (HD) 5 after the initial one, which revealed no evidence of colo-colonic intussusception. There was no colon wall thickening and no air bubble in the colon wall (Figure 2C and D).
The final diagnosis for the current case was colo-colonic intussusception with PPES.
The patient was started on intravenous antibiotics therapy with piperacillin/tazobactam 4.5 g every 8 h, and ornidazole 500 mg every 12 h. The patient fasted and was admitted to the general surgery department.
After follow-up CT at HD 5, the patient started sips of water at HD 6. A soft-blended diet started at HD 7. The patient had no discomfort after starting the diet, and she was discharged to home at HD 9.
The patient was transferred to our hospital for consideration of an operation but had no surgical treatment. At a follow-up visit 2 wk after discharge, the patient was asymptomatic and had no complaints.
PPES, also known as post-polypectomy syndrome or post-polypectomy coagulation syndrome, is a relatively rare complication of polypectomy with electrocoagulation that may cause perforation or bleeding. Transmural thermal injury can happen after electrocoagulation polypectomy when electrical current is applied during polypectomy which extends into the serosa and muscularis propria. As a result, a transmural burn and localized peritoneal inflammation can occur. CT is the gold-standard imaging for PPES patients, as it shows focal mural thickening with a stratified enhancement pattern, low attenuation with perilesional submucosal edema, and high attenuated infiltration of adjacent pericolic fat without extralunminal air[9]. Up to 5 d after the colonoscopic procedure, patients can develop localized abdominal pain, fever, signs of peritoneal irritation, and leukocytosis without perforation[10].
The rate of PPES ranges from 0.003% to 0.100%, while the incidence of perforation and hemorrhage is 0.3% and 0.6%, respectively[11]. In a large multicenter study, risk factors correlated with PPES included large size of lesion (> 2 cm), non-polypoidal lesions, lesions on the right sided colon (attributed to decreased thickness of bowel wall), and hypertension[8,10]. Our patient’s multiple right-sided treated lesions featured high-risk factors. Lacking information about the shape and size of lesions, we could not find other risk factors.
There was a specific finding in our case that should be noted. Colo-colonic intussusception was present in our case without definite evidence of obstruction. A review of the literature showed that in 1214 adult patients with intussusception, 63% of adult intussusceptions were related to a tumor, where 50% of which were malignant. Further, a malignant tumor was demonstrated to be the etiology in 48% of patients with colo-colonic intussusception[12]. But our patient had a full colonoscopy and had no evidence of a remnant tumor lesion that could be a leading point. Colon wall thickening due to PPES might induce colo-colonic intussusception.
There are several ways to prevent PPES during an endoscopic procedure. First, during hot snare polypectomy, we pull the polyp toward the central area of the lumen immediately before electrocoagulation so that the submucosa is pulled away from the muscularis propria and serosa as the current is applied[13]. In addition, a hot snare, not hot biopsy forceps, is used because the hot biopsy technique increases the risk of thermal injury to the submucosa[14,15]. Second, submucosal fluid injections are used for large polyps. Elevating a large polyp by injecting saline (or an alternative solution) into the submucosa before polyp transection may reduce the incidence of PPES, but there are no large studies to substantiate this hypothesis[10,16,17]. A submucosal fluid injection before polypectomy should theoretically decrease the incidence of transmural burn by enlarging the submucosal layer[2]. Third, we could use alternative polypectomy techniques. Cold snare polypectomy is not associated with PPES, and the available data suggest that the cold snare technique may be a safe and effective option for lesions that are ≥ 1 cm, located in the right colon, or have a non-polypoid shape[18,19].
Similar to this case, Kedia et al[13] reported a case of PPES with a radiology report suggesting ileocolic intussusception. In that case, the patient’s clinical signs worsened after 24 h and the patient underwent unnecessary diagnostic laparoscopy and was, as a result, exposed to possible operation related complications unnecessarily[20]. In this case, the patient’s clinical signs got better and showed no sign of obstruction, and we managed the patient conservatively and did not consider surgical intervention. This case demonstrates the necessity of combining the clinical scenario with radiologic findings to reach a differential diagnosis and optimal management plan.
Colo-colic intussusception can occur with PPES, and it can be properly treated conservatively.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): E
P-Reviewer: Chiu CC, Taiwan; Farid K, Egypt; Yu SP, China S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL
| 1. | Kim HW. What Is Different between Postpolypectomy Fever and Postpolypectomy Coagulation Syndrome? Clin Endosc. 2014;47:205-206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Hirasawa K, Sato C, Makazu M, Kaneko H, Kobayashi R, Kokawa A, Maeda S. Coagulation syndrome: Delayed perforation after colorectal endoscopic treatments. World J Gastrointest Endosc. 2015;7:1055-1061. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 60] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 3. | Nelson DB, McQuaid KR, Bond JH, Lieberman DA, Weiss DG, Johnston TK. Procedural success and complications of large-scale screening colonoscopy. Gastrointest Endosc. 2002;55:307-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 279] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 4. | Waye JD, Kahn O, Auerbach ME. Complications of colonoscopy and flexible sigmoidoscopy. Gastrointest Endosc Clin N Am. 1996;6:343-377. [PubMed] |
| 5. | Waye JD, Lewis BS, Yessayan S. Colonoscopy: a prospective report of complications. J Clin Gastroenterol. 1992;15:347-351. [PubMed] |
| 6. | Anderloni A, Jovani M, Hassan C, Repici A. Advances, problems, and complications of polypectomy. Clin Exp Gastroenterol. 2014;7:285-296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Benson BC, Myers JJ, Laczek JT. Postpolypectomy electrocoagulation syndrome: a mimicker of colonic perforation. Case Rep Emerg Med. 2013;2013:687931. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Cha JM, Lim KS, Lee SH, Joo YE, Hong SP, Kim TI, Kim HG, Park DI, Kim SE, Yang DH, Shin JE. Clinical outcomes and risk factors of post-polypectomy coagulation syndrome: a multicenter, retrospective, case-control study. Endoscopy. 2013;45:202-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 99] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 9. | Shin YJ, Kim YH, Lee KH, Lee YJ, Park JH. CT findings of post-polypectomy coagulation syndrome and colonic perforation in patients who underwent colonoscopic polypectomy. Clin Radiol. 2016;71:1030-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Sethi A, Song LM. Adverse events related to colonic endoscopic mucosal resection and polypectomy. Gastrointest Endosc Clin N Am. 2015;25:55-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Ko CW, Dominitz JA. Complications of colonoscopy: magnitude and management. Gastrointest Endosc Clin N Am. 2010;20:659-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 134] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 12. | Felix EL, Cohen MH, Bernstein AD, Schwartz JH. Adult intussusception; case report of recurrent intussusception and review of the literature. Am J Surg. 1976;131:758-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 126] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Kedia P, Waye JD. Colon polypectomy: a review of routine and advanced techniques. J Clin Gastroenterol. 2013;47:657-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Ferlitsch M, Moss A, Hassan C, Bhandari P, Dumonceau JM, Paspatis G, Jover R, Langner C, Bronzwaer M, Nalankilli K, Fockens P, Hazzan R, Gralnek IM, Gschwantler M, Waldmann E, Jeschek P, Penz D, Heresbach D, Moons L, Lemmers A, Paraskeva K, Pohl J, Ponchon T, Regula J, Repici A, Rutter MD, Burgess NG, Bourke MJ. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017;49:270-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 766] [Article Influence: 95.8] [Reference Citation Analysis (0)] |
| 15. | Metz AJ, Moss A, McLeod D, Tran K, Godfrey C, Chandra A, Bourke MJ. A blinded comparison of the safety and efficacy of hot biopsy forceps electrocauterization and conventional snare polypectomy for diminutive colonic polypectomy in a porcine model. Gastrointest Endosc. 2013;77:484-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Ferrara F, Luigiano C, Ghersi S, Fabbri C, Bassi M, Landi P, Polifemo AM, Billi P, Cennamo V, Consolo P, Alibrandi A, D'Imperio N. Efficacy, safety and outcomes of 'inject and cut' endoscopic mucosal resection for large sessile and flat colorectal polyps. Digestion. 2010;82:213-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Luigiano C, Consolo P, Scaffidi MG, Strangio G, Giacobbe G, Alibrandi A, Pallio S, Tortora A, Melita G, Familiari L. Endoscopic mucosal resection for large and giant sessile and flat colorectal polyps: a single-center experience with long-term follow-up. Endoscopy. 2009;41:829-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 18. | Gessl I, Waldmann E, Penz D, Majcher B, Dokladanska A, Hinterberger A, Szymanska A, Trauner M, Ferlitsch M. Resection rates and safety profile of cold vs. hot snare polypectomy in polyps sized 5-10 mm and 11-20 mm. Dig Liver Dis. 2019;51:536-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 19. | Suzuki S, Gotoda T, Kusano C, Ikehara H, Sugita A, Yamauchi M, Moriyama M. Width and depth of resection for small colorectal polyps: hot versus cold snare polypectomy. Gastrointest Endosc. 2018;87:1095-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 117] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 20. | Plumptre I, Tolppa T, Jawad ZAR, Zafar N. Donut rush to laparoscopy: post-polypectomy electrocoagulation syndrome and the 'pseudo-donut' sign. BJR Case Rep. 2020;6:20190023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |