Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.8893
Peer-review started: September 29, 2021
First decision: November 11, 2021
Revised: July 27, 2022
Article in press: July 27, 2022
Published online: September 6, 2022
Processing time: 330 Days and 16.9 Hours
Recently, the use of ligament advanced reinforcement system (LARS) artificial ligament, a new graft which has several unique advantages such as no donor-site morbidity, early recovery and no risk of disease transmission which has been a significant breakthrough for anatomical ligament reconstruction. Growing studies suggested that the special design of the LARS ligament with open fibers in its intra-articular part was believed to be more resistant to torsional fatigue and wearing. However, the safety and efficacy of LARS artificial ligament for ankle joint lateral collateral ankle ligament reconstruction has not been defined to date.
To evaluate the clinical results of all-arthroscopic anatomical reconstruction of ankle joint lateral collateral ligaments with the LARS artificial ligament for chronic ankle instability.
Twenty-two patients with chronic lateral instability underwent anatomical reconstruction of the lateral collateral ligaments of ankle with LARS artificial ligament. The visual analogue score (VAS), American Orthopaedic Foot and Ankle Society score (AOFAS score) and Karlsson score were used to evaluate the clinical results before and after surgery.
A total of 22 patients (22 ankles) were followed up for a mean of 12 mo. All patients reported significant improvement compared to their preoperative status. The mean AOFAS score improved from 42.3 ± 4.9 preoperatively to 90.4 ± 6.7 postoperatively. The mean Karlsson score improved from 38.5 ± 3.2 preoperatively to 90.1 ± 7.8 postoperatively. The mean VAS score improved from 1.9 ± 2.5 preoperatively to 0.8 ± 1.7 postoperatively.
All-arthroscopic anatomical reconstruction of the lateral collateral ligaments with LARS artificial ligament achieved a satisfactory surgical outcome for chronic ankle instability.
Core Tip: Chronic lateral ankle instability is usually caused directly by lateral collateral ligament injury. The ligament advanced reinforcement system (LARS) is a new graft with unique advantages such as low postoperative complication rates, early rehabilitation and its design makes it more resistant to torsional fatigue and wearing. However, the safety and efficacy of LARS artificial ligament for ankle joint lateral collateral ankle ligament reconstruction have not been determined to date. The purpose of this study was to evaluate this anatomical reconstructive surgery for chronic ankle instability by using LARS artificial ligament under all-arthroscopic conditions.
- Citation: Wang Y, Zhu JX. Arthroscopic anatomical reconstruction of lateral collateral ligaments with ligament advanced reinforcement system artificial ligament for chronic ankle instability. World J Clin Cases 2022; 10(25): 8893-8905
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/8893.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.8893
Ankle sprains are the most common sports injury and account for 10%-15% of such injuries[1,2]. Although the majority of patients have successful results after conservative treatment, up to 20%-40% have chronic mechanical instability requiring operative intervention[3].
There are various operative procedures to treat chronic lateral ankle instability including ligament repair and reconstruction. Ligament repair can be performed in patients with mild ankle instability and possess good quality of the remnant of the lateral collateral ligament. Anatomical reconstruction of the lateral collateral ligament is always suggested if the patient has the following conditions: high ankle instability, weak remnant of the lateral collateral ligament, generalized joint laxity, previous failed ligament repair for lateral ankle instability[4]. Ankle ligament reconstruction includes anatomical and non-anatomical reconstruction. Anatomical ligament reconstruction is the mainstream procedure at present[5] and is steadily gaining ground as a means of avoiding the risk of traumatic arthritis after ligament reconstruction[6]. The possibility of failure has been reported in different periods after direct repair with or without tissue augmentation[6], which has a series of complications such as increased infection rate caused by large incision, delayed healing of the incision, superficial peroneal nerve injury and deep venous thrombosis caused by long-term external fixation[7]. Therefore, ligament recon
A variety of different grafts are used for anatomical ligament reconstruction. Compared to autografts or allografts, artificial ligaments possess unique advantages such as no donor-site morbidity, early recovery and no risk of disease transmission. During recent years, with the development of ced biomaterials and the progress of refined surgical techniques, a novel artificial ligament scaffold—[the ligament advanced reinforcement system (LARS)—Surgical Implants and Devices, Arc-sur-Tille, France] has been developed[8]. LARS artificial ligament is a bio mimic scaffold of artificial ligament made of polyester [polyethylene terephthalate (PET)] fibers. In vitro cell culture indicates that fibroblasts adhere to and encapsulate LARS artificial ligament[9], and in vivo, LARS artificial ligament induces growth of autologous collagen tissue and neoligament formation[10]. The biomechanics of resisting tension, flexion and torsion load of LARS artificial ligaments are good[11]. LARS, due to its mechanical properties, biocompatibility, and unique weaving method, showed good clinical performance with low postoperative complication rates, early rehabilitation and has long been held in good regard by orthopedists in China[12]. At present, it is widely used in the reconstruction of anterior and posterior cruciate ligaments and some clinical studies have reported that the application of LARS artificial ligament is effective in patch repair of massive rotator cuff tears[13].
To date, there have been few reports about the use of artificial ligament for lateral collateral ligament reconstruction of the ankle. The purpose of this study was to evaluate reconstructive surgery using LARS artificial ligament.
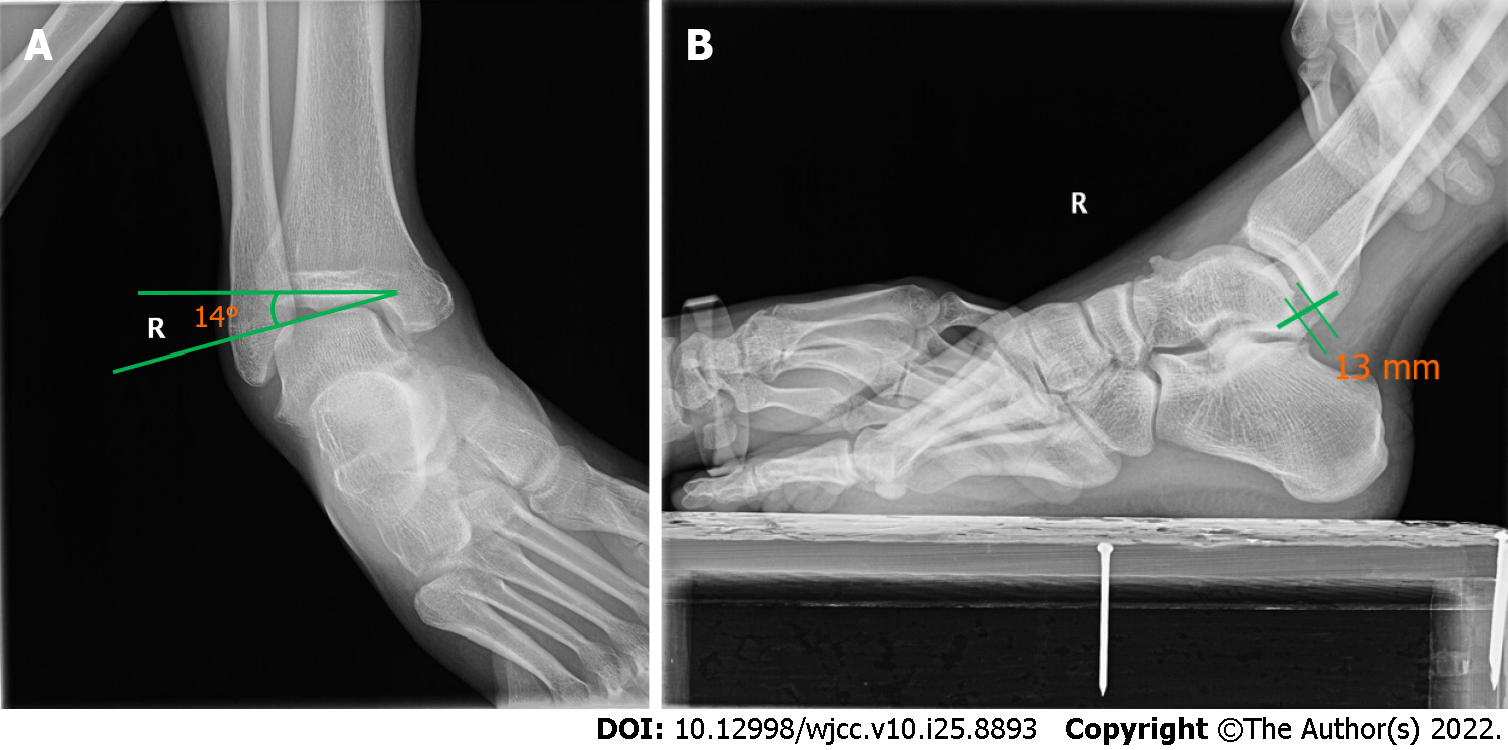
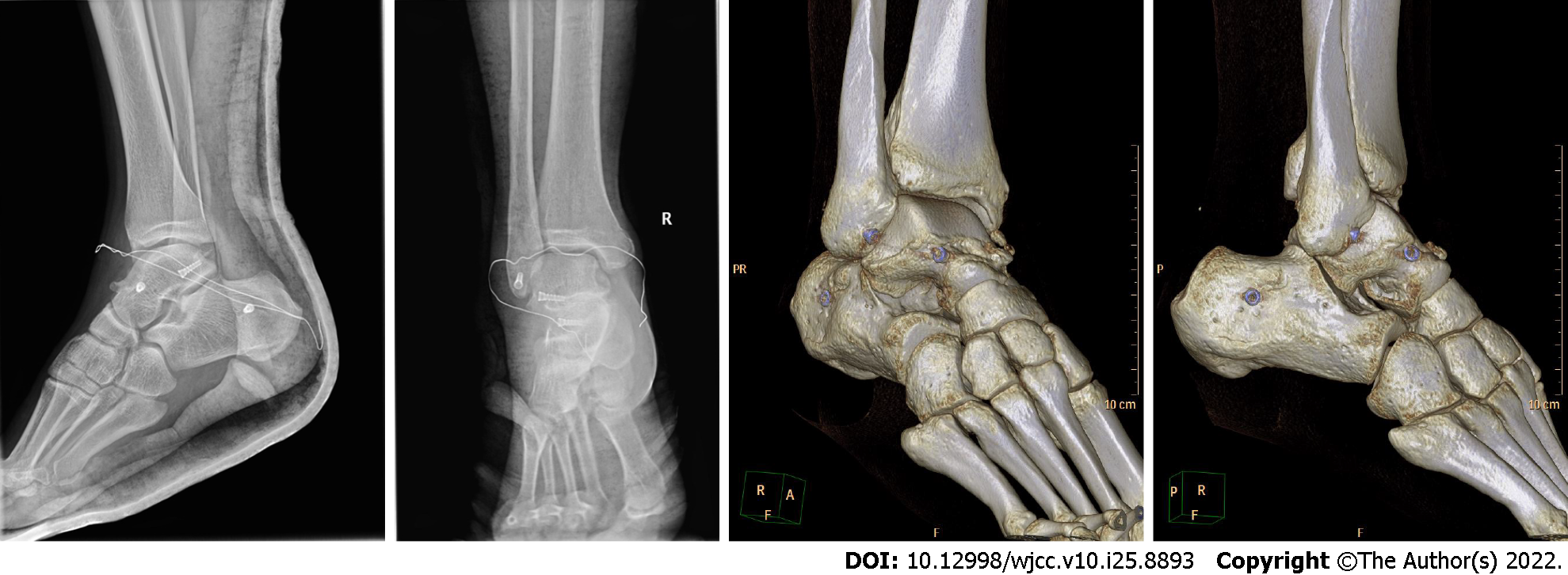
From July 2018 to September 2020, 22 patients (22 ankles) who were diagnosed with chronic lateral ankle instability underwent anatomical lateral collateral ligament reconstruction using LARS artificial ligament. There were 16 male patients (16 ankles) and 6 female patients (6 ankles) with a mean age of 27 years (range: 18-45 years). The mean time from initial injury to surgery was 9 mo (range: 6-12 mo). These patients had ankle instability or repetitive ankle sprain injuries despite a minimum of 6 mo of nonoperative treatment with a rehabilitation program. Clinical examination revealed in every case a positive anterior drawer and talar tilt test. Before surgery, standard plain radiographs including classical comparative weight-bearing anteroposterior and lateral are useful, which is helpful to assess hindfoot alignment[14]. Comparative stress radiographic views (Figure 1) including anterior drawer test and talar tilt test may be performed, although, it should be recognized that these have a high rate of false-negative results[15]. Radiographic instability is defined by a talar tilt angle > 10° or > 10° difference with the other side and/or an anterior drawer > 8 mm or > 3 mm difference with the contralateral ankle[14]. Magnetic resonance imaging may be helpful in the presence of deep pain to assess for osteochondral lesions and tendon injuries and it also confirms the presence of chronic ligamentous injury.
Surgical indications include chronic ankle instability associated with[16]: (1) Overweight patients (BMI > 25); (2) Heavy occupation or sports requirement; (3) Congenital ligament laxity (Beighton scale > 8); (4) Nonviable remnant ligament tissue; and (5) Previously failed repair procedure.
All patients with the following surgical contraindications were excluded: (1) Ankle infection; (2) Fracture; (3) Ankle arthritis grade > 2 according to Morrey and Wiedeman classification; and (4) Functional instability without mechanical instability on stress radiographs.
All clinical examinations and surgery were performed by the same surgeon and the first author served as first assistant. The study received ethical approval from the Human Ethics Research Board of our hospital.
The surgery was performed under spinal anesthesia. The patients were placed in the supine position. No tourniquet was required at the thigh. A standard 4.0-mm 30° arthroscope and a 4.5-mm bone/soft tissue shaver blade were used. Three or four portals were made (Figure 2): An anteromedial portal (portal 1), an anterolateral portal (portal 2) and a sinus tarsi portal that was the lateral portal (portal 3). The arthroscopic technique was performed in four steps.
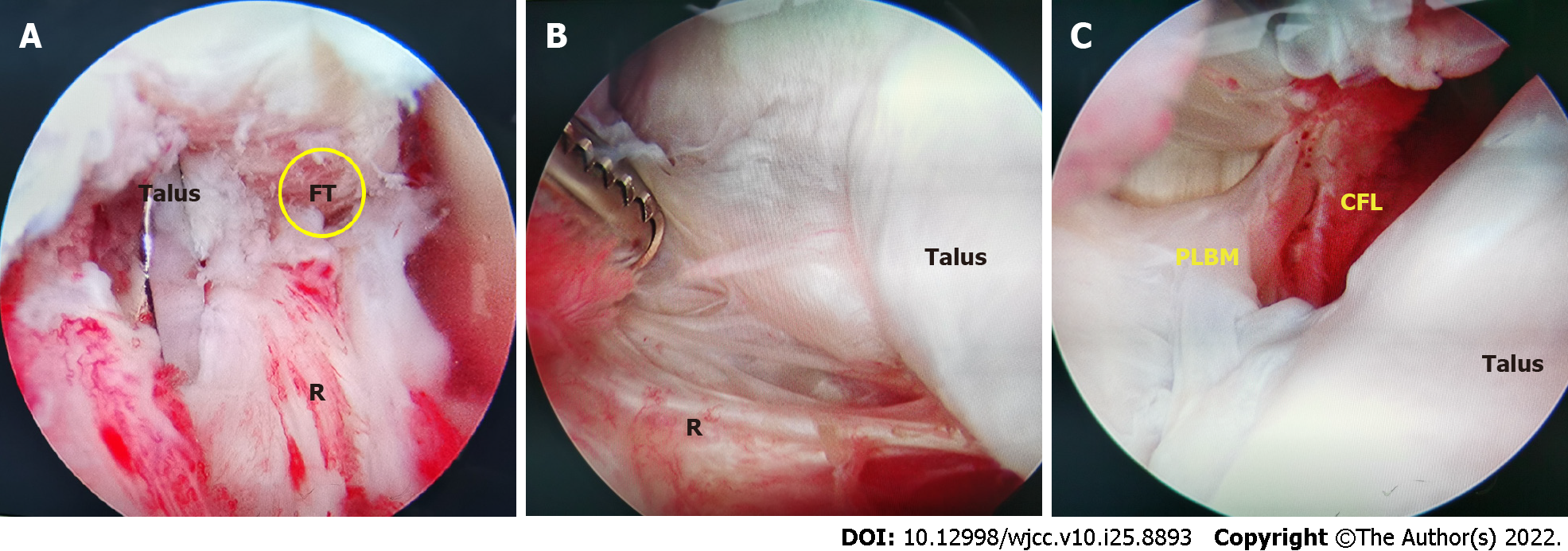
The first step was anterior routine medial and lateral arthroscopy. An anteromedial portal was used as a viewing portal and the routine anterolateral portal was made using its transillumination feature. Through these two portals, the ankle joint was inspected and any intra-articular disorders were assessed and managed by shaving off of inflamed synovial membrane, microfracture for cartilage injuries and excision of the osteophytes[17]. The anterior tibiofibular ligament was used as a first landmark to estimate the remnant of the anterior talofibular ligament (ATFL) and find the insertion of the ATFL. Its distal adjacent was the proximal insertion of the calcaneo-fibular ligament (CFL) (Figure 3).
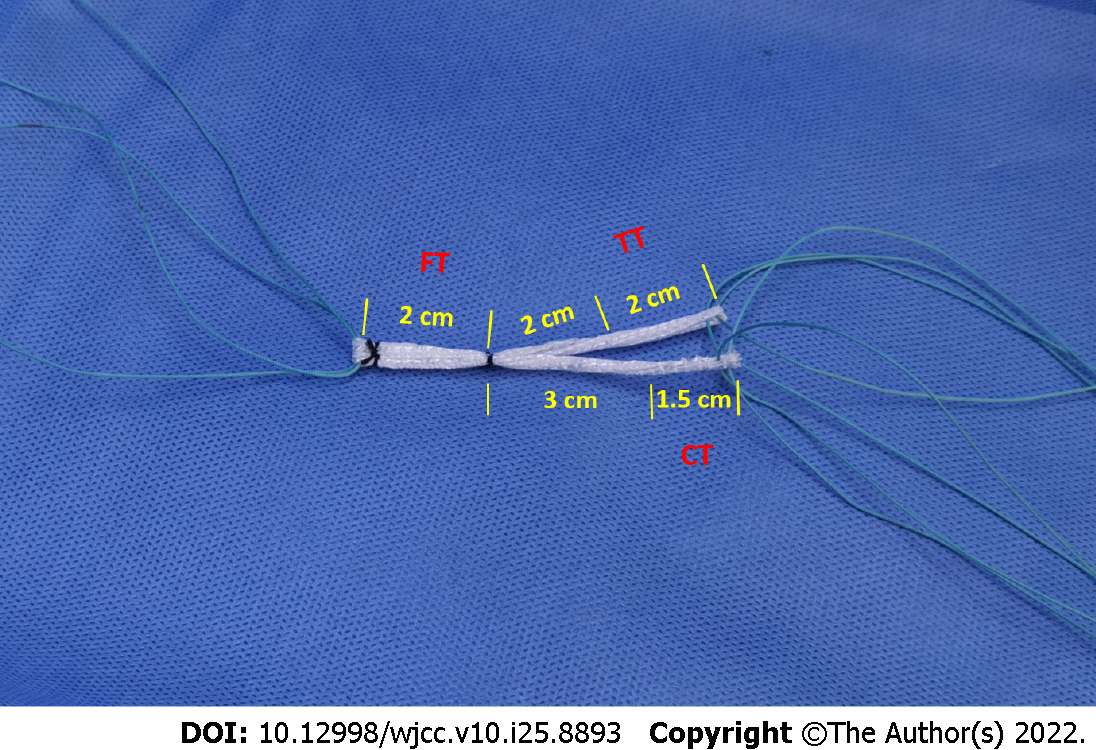
The second step was preparing the LARS artificial ligament after determining the poor quality of the ATFL remnant and that the ligament reconstruction should be performed. The intraosseous part of the LARS artificial ligament tumor strip patch (LARS, CR30) was used to construct an anatomical Y configuration with a diameter of approximately 3 mm and an intraosseous and intra-articular length of 20 mm. High-strength sutures were at all three ends of the Y-graft to maintain the tension of the graft traction[18]. The fibular section of the Y-graft was reserved to a length of 20 mm. The calcaneal section was constructed to a total length of 45 mm to ensure an intra-articular length of 30 mm and a length of 15 mm in the calcaneal tunnel. The talar section was constructed to a total length of 40 mm to ensure an intra-articular length of 20 mm and a length of 20 mm in the talar tunnel (Figure 4). The Y-graft was submerged in sterile saline with antibiotics when it was ready.
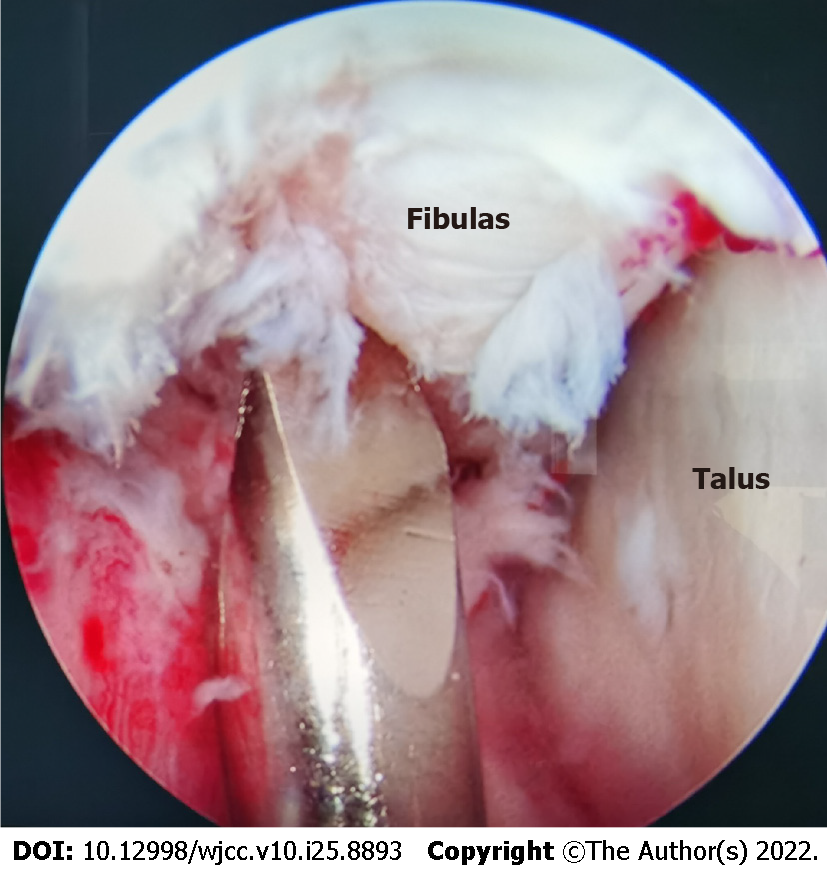
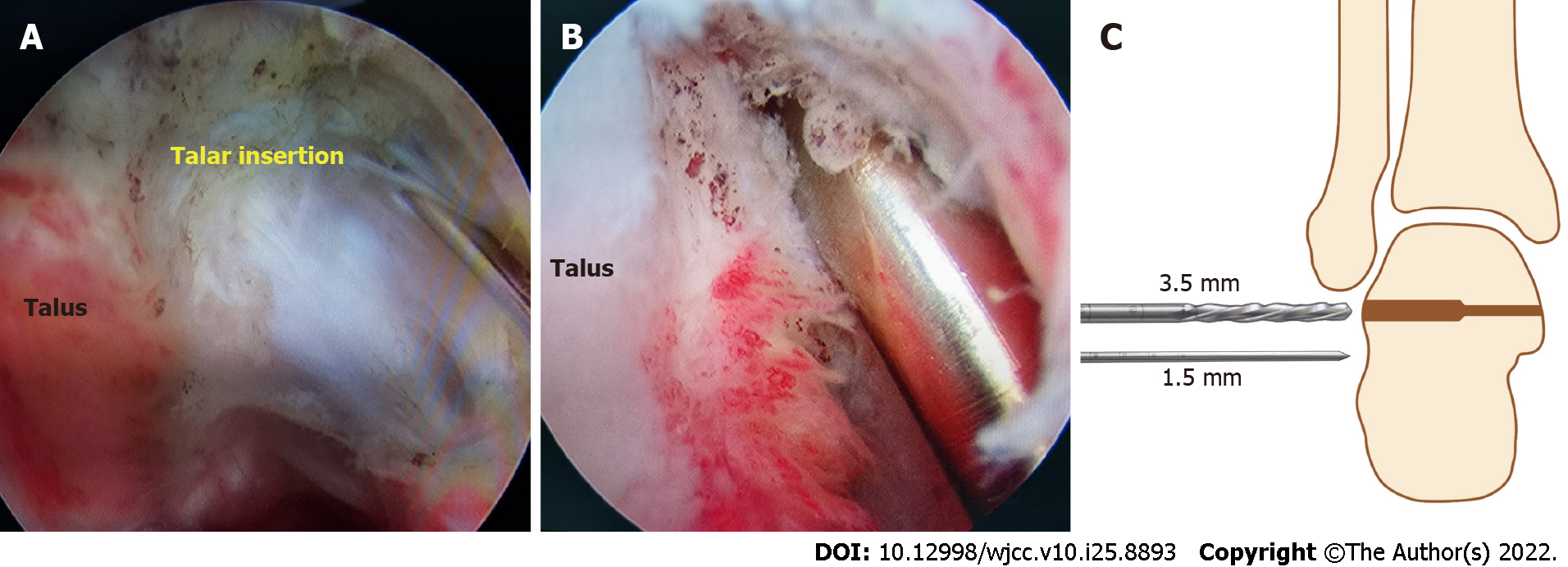
The third step was the preparation of the bone tunnels which were not full length. A third arthroscopic portal was prepared under routine monitoring of the anterolateral portal that was just above the sinus tarsi on the intersection of the fibular tunnel axis and the superior border of the peroneal tendons[19]. Using this third portal as a working portal, the dissection was continued to expose the talar footprint of the ATFL and the calcaneal footprint of the CFL. A guide pin allowed us to drill a 3.0-mm diameter calcaneal tunnel from the calcaneal footprint to the anterior medial edge of the calcaneal tuberosity (Figure 5). An oblique fibular tunnel with a diameter of 3.0 mm was drilled with a guide pin starting at the confluent insertion of the ATFL and CFL (Figure 6)[20]. It was critical to ensure that the tunnel was placed in the center of the fibula in the coronal plane to minimize the risk of tunnel compromise or blowout. Finally, we drilled the talar tunnel under monitoring of the anterolateral portal (Figure 7). The tunnel entrance was located at the talar footprint of the ATFL (Figure 7A), which was below the triangular region of the talus on the midpoint between the superolateral edge of the talar body and the subtalar joint. A 2.0-mm diameter guide pin was then inserted through the sinus tarsi portal, aiming toward the medial malleolus in a superior direction. With this orientation, a completely safe 3 mm × 20 mm tunnel can be drilled using the 3.0-mm hollow drill[21]. The length of the tunnel was strictly controlled within 20 mm (Figure 7C).
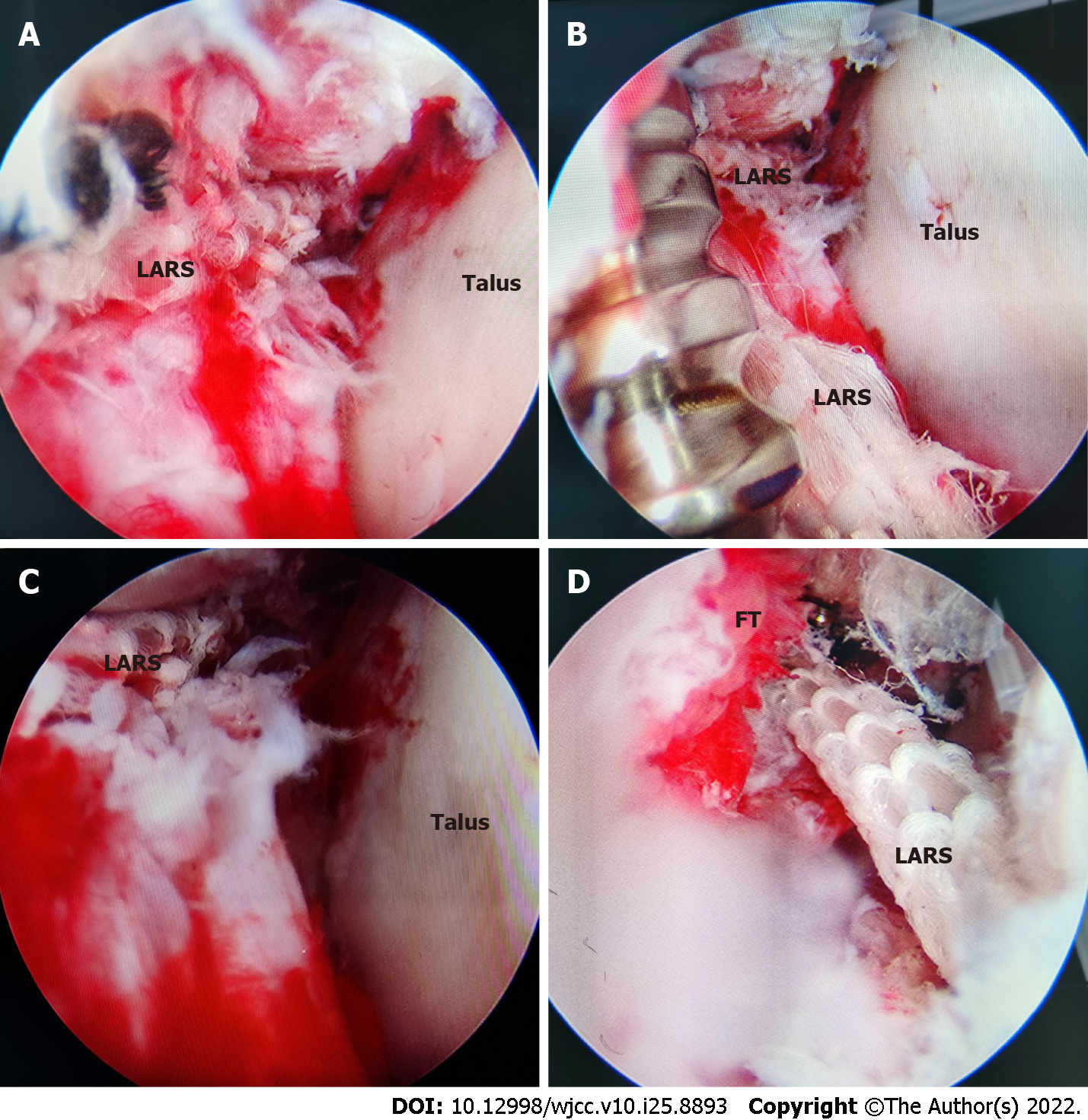
The last step corresponded to the positioning and fixation of the graft (Figure 8). All three stems of the anatomic Y-graft were delivered through the anterolateral portal using an inside-out technique[18]. First, the high-strength sutures passing through the talar stem of the graft were attached to a guidewire which was passed through the talar tunnel. Similarly, the high-strength sutures passing through the fibular and calcaneal stems were attached to a guidewire and passed through their respective tunnels in sequence to pull the grafts through the anterolateral portal and into position. Each graft end was tensioned using the sutures exiting the skin on the opposite side of each bone tunnel. The three anatomic Y-graft stems were inserted into their respective tunnels to a depth of at least 15 mm and each bony attachment of the anatomic Y-graft was fixed with a metal extrusion screw (LARS, F314715, 4.7 mm × 15 mm) while a 30-N tension force was applied[18]. The fibular stem was fixed. The calcaneal stem was fixed while the ankle was in a neutral position with 0° of flexion. The talar stem was fixed in the same manner as the calcaneal attachment and the foot was slightly valgus. After that, full range ankle movements were performed 20 times to confirm the isometricity and adjust the tension of the graft. Once all three stems of the anatomic Y-graft were fixed, the sutures were removed and the incisions were closed using nylon sutures.
After the operation, the ankle was immobilized in a neutral position using a short leg cast. On the 3rd day after surgery, the cast was changed to an ankle orthosis after detumescence in the operative area, the passive and active dorsi and plantar flexion were allowed and X-ray and 3D computed tomography were performed (Figure 9). Inversion and eversion movements were protected during the first 6 wk by an ankle orthosis. At 6 wk postoperatively, the patients started walking without crutches and were allowed to resume full athletic activity at 6 mo after surgery.
The patients were clinically evaluated before the operation and at follow-up using the visual analog scale (VAS), American Orthopaedic Foot and Ankle Society (AOFAS) score and Karlsson score[22].The hindfoot motion was measured using a goniometer with the patient prone and the knee in 90° of flexion and the ankle in 0° of dorsiflexion. The range of motion for dorsiflexion and plantar flexion were also recorded at both ankle joints. A manual anterior drawer test and inversion tests were also performed in all patients.
Paired-sample t tests were used for statistical analysis. The significance level was defined as P < 0.05. Statistical analysis was performed using SPSS version 21.0 (SPSS, Chicago, IL, United States).
All patients reported the disappearance of the instability complaints that they had experienced prior to the operation. No vascular or neural complications occurred during or after the operation in any patients. One patient had poor wound healing which gradually resolved after debridement, suturing and changing the dressing. Another patient presented with numbness of the lateral dorsal part of the foot that resolved after 6 wk.
A total of 22 patients (22 ankles) were followed up for a mean 12 mo (range: 7-16 mo). The mean AOFAS score improved from 42.3 ± 4.9 preoperatively to 90.4 ± 6.7 postoperatively (P = 0.000). The mean Karlsson score improved from 38.5 ± 3.2 preoperatively to 90.1 ± 7.8 postoperatively (P = 0.000). The mean VAS score improved from 1.9 ± 2.5 preoperatively to 0.8 ± 1.7 postoperatively (P < 0.001). The difference between the results of the preoperative and the postoperative were significant (P < 0.05). The average dorsiflexion, as measured with a goniometer, was 14.8 ± 1.8, compared with 15.1 ± 1.7 in the non-operated ankle (P = 0.092), and average plantar flexion was 45.0 ± 4.7, compared with 46.7 ± 2.6° in the non-operated ankle (P = 0.073). The average hindfoot motion was 18.9 ± 2.4, compared with 19.0 ± 2.4 in the non-operated ankle (P = 0.240). The differences between the results of the operated and non-operated ankle were not significant (P > 0.05).
Postoperatively, 21 patients (95%) returned to sports activity. Nineteen patients (88%) returned at the same level and two returned to a lower level. Patients returned to work at a mean of 2 mo (range: 1.5-3 mo). Manual stress testing showed that 21 patients (21 ankles) were stable in both the anterior drawer and inversion tests. One patient (one ankle) showed a mild positive anterior drawer test of the talus. No patient was found to have excessive generalized joint laxity. Patients reported that they were satisfied or very satisfied with the procedure in 21 cases (95%). The results of the patients were excellent (AOFAS score 95, Karlsson score 97 and VAS score 0.9).
In this study, the patients achieved satisfactory clinical results after lateral collateral ligament reconstruction using the all-arthroscopic anatomical reconstruction technique with LARS artificial ligament. Our reconstruction method restored the normal anatomy by positioning the LARS artificial ligament graft at the original ligament point and insertion. One patient reported residual instability on uneven ground but he thought it was better than the preoperative condition. This study supported the effectiveness of this approach in this group of patients with severe instability.
Injury of lateral collateral ligament that results from ankle varus instability is the most common sports-related ankle injury (77%)[23-25]. It mostly affects the lateral ligament complex including the ATFL and/or CFL[14,16]. There are dozens of surgical treatments for the injury of the lateral collateral ligament of the ankle; classical Broström–Gould ligament repair and anatomical reconstruction are presently the most popular in academic circles. Ligament repair refers to open ligament tightening or extensor retinaculum reinforcement for ATFL and CFL.
We think that ligament repair can be chosen for the individuals who are older, the ankle joint is stable, the quality of the remnant ligament is good and the exercise requirements are not high. For the individuals with severe lateral ankle instability, longer injury time, younger age and higher exercise requirements, we think that anatomical reconstruction is an appropriate treatment to promote the rapid recovery of these patients.
The problem to be considered in ligament reconstruction surgery is the choice of graft during the operation. At present, the types of grafts mainly include autografts, allografts and artificial ligament grafts. Autografts are the mainstream graft materials at present including palmaris longus muscle, semitendinosus muscle, peroneus longus muscle and other donor sites. However, the reports show that after tenotomy, a large number of patients may have temporary or permanent pain, numbness, muscle weakness, joint instability, prolonged rehabilitation time and other complications in the donor site[26,27]. At the same time, there is a certain probability of creep after autologous tendon graft which leads to the failure of autograft[28,29]. The downside of allografts with their potential increase of infection rate and the spread of infectious diseases cannot be ignored. Artificial grafts can avoid the series of adverse reactions mentioned above, so they have gradually increased in use in recent years.
The special design of the LARS ligament with open fibers in its intra-articular part is believed to make it more resistant to torsional fatigue and wearing[30]. However, there are few reports about the clinical application of LARS artificial ligament in the reconstruction of lateral collateral ligament of the ankle joint. Japanese investigators have reported the clinical application of Leed–Keio ligament[8], another artificial ligament similar to LARS ,which is widely adopted in Europe and Asia[12]. These two types of artificial ligaments share common features: being capable of inducing the migration of fibroblasts and the regeneration of native tissue, and they are both made of PET, an important tissue engineering material used in artificial ligament fabrication[9]. Di Benedetto et al[10] recently reported a histological and ultrastructural study of an intact Leeds–Keio ligament 20 years after implantation, which showed that when artificial ligament scaffold made of PET polyester was implanted into the knee, the ligament, as a nondegradable scaffold, induced fibroblast migration and regeneration of collagen tissue. The tissue could remodel under physiological load and new ligament with good function was obtained; thus, good long-term clinical results were ensured[10,11]. In the present study, which has followed the same patients over an extended period, there were no cases with a decrease in the range of joint motion, with further development of osteoarthritis, or with a poorer result than those observed in our earlier study.
It should be pointed out that the early functional improvement and rapid postoperative recovery have given LARS artificial ligaments a significant advantage over autografts or allografts. Biomechanical tests have proved that the LARS ligament, weaved by PET, possesses sufficient strength. After enduring a persistent traction of 1700 N and subsequent relaxation in 1 d, the increase in length is < 1.5%[31], while the strength of the autogenous ligament graft is lower. This particular advantage makes LARS a favorable choice for professional athletes and people highly motivated by sports exercise.
The artificial grafts that we selected met the strength requirements and at the same time, the smaller diameter made the diameter of the bone tunnel smaller and the bone mass was maximumly preserved. A number of clinical studies have shown that the diameter of the bone tunnel in the reconstruction of ankle lateral collateral ligament with autogenous or allogeneic tendon is mostly 6 mm, while the operation of fibula graft folding makes the diameter of the bone tunnel larger[19,32]. It increases the risk of iatrogenic fracture when drilling the bone tunnel, which needs more accurate positioning during the operation. Meanwhile, it is necessary to ensure the single success of positioning and reduce the chance of error correction. It has been shown that the thicker bone tunnels mean an increased risk of talar osteonecrosis[33,34]. In our clinical study, the cut LARS tumor strips showed a flaky structure with a width of 6 mm and its cylindrical diameter was only 3 mm after treatment and smaller than that of other grafts. The length of the talar tunnel that we controlled was 15-20 mm which was shorter than that of 30 mm in other operations[32]. Many studies have shown that bone tunnel length ≥ 15 mm is the standard to ensure stability of ligament fixation[35]. Therefore, by making a talar tunnel with smaller diameter and shorter length, the loss of bone mass and the destruction of talar vessels are reduced, thus reducing the risk of iatrogenic fracture and talar osteonecrosis. All our clinical cases were followed up for > 6 mo and no cases of talar osteonecrosis were found but, it has been reported previously in other studies[33,34] which we will follow up on in the future.
In the past, one of the criticisms of artificial ligaments was that it had poor malleability and could not adapt to the flexion and extension of human joints of unequal length which limited joint flexion and extension after the operation. With the continuous development of the concept of anterior cruciate ligament near-isometric reconstruction of the knee in recent years, the application of LARS in anterior cruciate ligament reconstruction has gradually increased. However, different from the two-bundle theory of anterior cruciate ligament, both ATFL and CFL of the ankle joint are tension movements during flexion and extension, so the application of LARS in ankle ligament reconstruction has theo
Another important advantage of this surgery is that the operation is all-arthroscopic. The open technique requires at least a 4-cm-long incision with significant dissection and soft tissue debridement and it sometimes causes superficial nerve injury[41]. Compared with the open technique, all-arthroscopic surgery has a smaller incision (1 cm), lower probability of nerve injury, faster postoperative recovery, is more aesthetic and the postoperative satisfaction of patients is high. However, skilled arthroscopic techniques are needed. When locating the bone tunnel and drilling, we can locate the anatomical insertion under arthroscopy, which is more accurate, but the narrow space makes the operation complicated and sometimes it is necessary to use the probe to enlarge the joint cavity artificially. Combined with the skilled cooperation of assistants, the operation can be conducted smoothly. If the proficiency is poor, the operation time is prolonged which increases the infection rate and the probability of nerve injury. Blurred vision leads to inaccurate positioning or poor surgical process. At present, there are also related reports about the techniques of ankle ligament repair and all-arthroscopic reconstruction[16,42,43], but the all-arthroscopic technique combined with LARS ligament to reconstruct the lateral collateral ligament of the ankle has not been reported.
Our study showed that for young patients with chronic ankle instability who needed high-intensity exercise, the lateral collateral ligament of the ankle was reconstructed by LARS artificial ligament transplantation using an all-arthroscopic procedure with good clinical results within 7-16 mo follow-up. No failures have been found so far. Except for a few cases of superficial peroneal nerve paralysis and poor incision healing (all recovered after follow-up) and the incidence of complications was low. No talar osteonecrosis occurred and 65% of the patients had resumed moderate intensity exercise. Therefore, we consider LARS artificial ligament to be an alternative graft for the reconstruction of the lateral collateral ligament of the ankle, especially for patients with a long disease course and failure after ATFL repair and who are unwilling to undergo autograft or allograft reconstruction.
This study also had some limitations. First, this was a retrospective study; there was no cohort study in the control group and the number of cases was small which was also related to the more stringent inclusion criteria. Second, our mean follow-up time was short, averaging 1 year, and longer-term follow-up should be carried out to determine the long-term clinical results of the reconstruction of the lateral collateral ligament of the ankle with LARS artificial ligament. Third, techniques are being developed and improved to perform anatomical reconstructions with LARS artificial ligament using all-arthroscopic procedures and we are still exploring techniques to make localization easier and tunnel fabrication optimized. We believe that further follow-up studies are required before these techniques can be adopted as routine surgical procedures.
Based on the results of our study, we believe that an all-arthroscopic anatomical reconstruction of the lateral collateral ankle ligament with LARS artificial ligament achieves a satisfactory surgical outcome for chronic ankle instability.
Ligament advanced reinforcement system (LARS), due to its mechanical properties, biocompatibility and unique weaving method showed good clinical performance with low postoperative complication rates and early rehabilitation and has long been held in good grace by orthopedists. At present, it is widely used in the reconstruction of anterior and posterior cruciate ligaments of knee joints. However, there have been a few reports about the use of artificial ligament for lateral collateral ligament reconstruction of the ankle. Based on the results of our study, we believe that an All-arthroscopic anatomical reconstruction of the lateral collateral ankle ligament with LARS artificial ligament achieves a satisfactory surgical outcome for chronic ankle instability.
To determine the safety and efficacy of all-arthroscopic anatomical reconstruction of ankle joint lateral collateral ligament with LARS artificial ligament for chronic ankle instability
To evaluate the clinical results of all-arthroscopic anatomical reconstruction of ankle joint lateral collateral ligaments with the LARS artificial ligament for chronic ankle instability.
We used LARS artificial ligament on lateral collateral ankle ligament reconstruction combined with an all-arthroscopic operation and propose that anatomical reconstruction of the lateral collateral ligaments with LARS artificial ligament can achieve a satisfactory surgical outcome for chronic ankle instability.
No patient was found to have excessive generalized joint laxity. Patients reported that they were satisfied or very satisfied with the procedure in 21 cases (95%). The results of the patients were excellent (AOFAS score 95, Karlsson score 97 and VAS score 0.9).
All-arthroscopic anatomical reconstruction of the lateral collateral ankle ligament with LARS artificial ligament achieves a satisfactory surgical outcome for chronic ankle instability.
Although there are precedents for ankle ligament reconstruction with artificial ligaments, our arthroscopic exercises and biomechanical studies on cadaveric models will also be carried out in an orderly manner.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Castellote-Caballero Y, Spain; Muthu S, India S-Editor: Liu JH L-Editor: Filipodia P-Editor: Liu JH
| 1. | Lassiter TE Jr, Malone TR, Garrett WE Jr. Injury to the lateral ligaments of the ankle. Orthop Clin North Am. 1989;20:629-640. [PubMed] |
| 2. | MacAuley D. Ankle injuries: same joint, different sports. Med Sci Sports Exerc. 1999;31:S409-S411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Karlsson J, Lansinger O. Chronic lateral instability of the ankle in athletes. Sports Med. 1993;16:355-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 66] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Baumhauer JF, O'Brien T. Surgical Considerations in the Treatment of Ankle Instability. J Athl Train. 2002;37:458-462. [PubMed] |
| 5. | Takao M, Oae K, Uchio Y, Ochi M, Yamamoto H. Anatomical reconstruction of the lateral ligaments of the ankle with a gracilis autograft: a new technique using an interference fit anchoring system. Am J Sports Med. 2005;33:814-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 114] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Acevedo JI, Mangone P. Ankle instability and arthroscopic lateral ligament repair. Foot Ankle Clin. 2015;20:59-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Corte-Real NM, Moreira RM. Arthroscopic repair of chronic lateral ankle instability. Foot Ankle Int. 2009;30:213-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 152] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 8. | Usami N, Inokuchi S, Hiraishi E, Miyanaga M, Waseda A. Clinical application of artificial ligament for ankle instability--long-term follow-up. J Long Term Eff Med Implants. 2000;10:239-250. [PubMed] |
| 9. | Li H, Chen S. Biomedical coatings on polyethylene terephthalate artificial ligaments. J Biomed Mater Res A. 2015;103:839-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Di Benedetto P, Giardini P, Beltrame A, Mancuso F, Gisonni R, Causero A. Histological analysis of ACL reconstruction failures due to synthetic-ACL (LARS) ruptures. Acta Biomed. 2020;91:136-145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Jones AP, Sidhom S, Sefton G. Long-term clinical review (10-20 years) after reconstruction of the anterior cruciate ligament using the Leeds-Keio synthetic ligament. J Long Term Eff Med Implants. 2007;17:59-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Chen T, Jiang J, Chen S. Status and headway of the clinical application of artificial ligaments. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;2:15-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Hagemeister N, Duval N, Yahia L', Krudwig W, Witzel U, de Guise JA. Comparison of two methods for reconstruction of the posterior cruciate ligament using a computer based method: quantitative evaluation of laxity, three-dimensional kinematics and ligament deformation measurement in cadaver knees. Knee. 2002;9:291-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Crombé A, Borghol S, Guillo S, Pesquer L, Dallaudiere B. Arthroscopic reconstruction of the lateral ankle ligaments: Radiological evaluation and short-term clinical outcome. Diagn Interv Imaging. 2019;100:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Tourné Y, Besse JL, Mabit C; Sofcot. Chronic ankle instability. Which tests to assess the lesions? Orthop Traumatol Surg Res. 2010;96:433-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 16. | Guillo S, Bauer T, Lee JW, Takao M, Kong SW, Stone JW, Mangone PG, Molloy A, Perera A, Pearce CJ, Michels F, Tourné Y, Ghorbani A, Calder J. Consensus in chronic ankle instability: aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumatol Surg Res. 2013;99:S411-S419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 198] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 17. | Hua Y, Chen S, Li Y, Chen J, Li H. Combination of modified Broström procedure with ankle arthroscopy for chronic ankle instability accompanied by intra-articular symptoms. Arthroscopy. 2010;26:524-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 114] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 18. | Takao M, Glazebrook M, Stone J, Guillo S. Ankle Arthroscopic Reconstruction of Lateral Ligaments (Ankle Anti-ROLL). Arthrosc Tech. 2015;4:e595-e600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Guillo S, Cordier G, Sonnery-Cottet B, Bauer T. Anatomical reconstruction of the anterior talofibular and calcaneofibular ligaments with an all-arthroscopic surgical technique. Orthop Traumatol Surg Res. 2014;100:S413-S417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 20. | Cordier G, Ovigue J, Dalmau-Pastor M, Michels F. Endoscopic anatomic ligament reconstruction is a reliable option to treat chronic lateral ankle instability. Knee Surg Sports Traumatol Arthrosc. 2020;28:86-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 21. | Michels F, Guillo S, Vanrietvelde F, Brugman E; Ankle Instability Group, Stockmans F. How to drill the talar tunnel in ATFL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2016;24:991-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Burn A, Buerer Y, Chopra S, Winkler M, Crevoisier X. Critical evaluation of outcome scales assessment of lateral ankle ligament reconstruction. Foot Ankle Int. 2013;34:995-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Thompson C, Schabrun S, Romero R, Bialocerkowski A, van Dieen J, Marshall P. Factors Contributing to Chronic Ankle Instability: A Systematic Review and Meta-Analysis of Systematic Reviews. Sports Med. 2018;48:189-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 136] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 24. | Balduini FC, Tetzlaff J. Historical perspectives on injuries of the ligaments of the ankle. Clin Sports Med. 1982;1:3-12. [PubMed] |
| 25. | Breitenseher MJ. [Acute ankle injuries]. Radiologe. 1999;39:16-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17:971-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 329] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 27. | Shelton WR, Fagan BC. Autografts commonly used in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2011;19:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 88] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 28. | Boorman RS, Thornton GM, Shrive NG, Frank CB. Ligament grafts become more susceptible to creep within days after surgery: evidence for early enzymatic degradation of a ligament graft in a rabbit model. Acta Orthop Scand. 2002;73:568-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Thornton GM, Boorman RS, Shrive NG, Frank CB. Medial collateral ligament autografts have increased creep response for at least two years and early immobilization makes this worse. J Orthop Res. 2002;20:346-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Kentel M, Barnaś M, Witkowski J, Reichert P. Treatment results and safety assessment of the LARS system for the reconstruction of the anterior cruciate ligament. Adv Clin Exp Med. 2021;30:379-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Gao K, Chen S, Wang L, Zhang W, Kang Y, Dong Q, Zhou H, Li L. Anterior cruciate ligament reconstruction with LARS artificial ligament: a multicenter study with 3- to 5-year follow-up. Arthroscopy. 2010;26:515-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 106] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 32. | Guillo S, Archbold P, Perera A, Bauer T, Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014;3:e593-e598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 33. | Chiodo CP, Herbst SA. Osteonecrosis of the talus. Foot Ankle Clin. 2004;9:745-755, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 34. | Gui J, Jiang Y, Li Y, Tao T, Li W, Zhang K, Yao W, Dong P. All Arthroscopic Remnant-Preserving Technique to Reconstruct the Lateral Ankle Ligament Complex. Arthrosc Tech. 2017;6:e549-e557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 35. | Meacham BP, Granata JD, Berlet GC. Tenodesis reconstruction for chronic ankle instability: graft considerations and structures at risk with tunnel placement. Foot Ankle Spec. 2012;5:378-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 36. | Burks RT, Morgan J. Anatomy of the lateral ankle ligaments. Am J Sports Med. 1994;22:72-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 170] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 37. | Neuschwander TB, Indresano AA, Hughes TH, Smith BW. Footprint of the lateral ligament complex of the ankle. Foot Ankle Int. 2013;34:582-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 38. | Pihlajamäki H, Hietaniemi K, Paavola M, Visuri T, Mattila VM. Surgical versus functional treatment for acute ruptures of the lateral ligament complex of the ankle in young men: a randomized controlled trial. J Bone Joint Surg Am. 2010;92:2367-2374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 39. | Golanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, van Dijk CN. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010;18:557-569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 212] [Cited by in RCA: 229] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 40. | van den Bekerom MP, Oostra RJ, Golanó P, van Dijk CN. The anatomy in relation to injury of the lateral collateral ligaments of the ankle: a current concepts review. Clin Anat. 2008;21:619-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 41. | Karlsson J, Eriksson BI, Bergsten T, Rudholm O, Swärd L. Comparison of two anatomic reconstructions for chronic lateral instability of the ankle joint. Am J Sports Med. 1997;25:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 145] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 42. | Michels F, Cordier G, Guillo S, Stockmans F; ESKKA-AFAS Ankle Instability Group. Endoscopic Ankle Lateral Ligament Graft Anatomic Reconstruction. Foot Ankle Clin. 2016;21:665-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 43. | Song B, Li C, Chen N, Chen Z, Zhang Y, Zhou Y, Li W. All-arthroscopic anatomical reconstruction of anterior talofibular ligament using semitendinosus autografts. Int Orthop. 2017;41:975-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |