Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.8854
Peer-review started: February 16, 2022
First decision: June 7, 2022
Revised: June 16, 2022
Accepted: July 22, 2022
Article in press: July 22, 2022
Published online: September 6, 2022
Processing time: 190 Days and 18.4 Hours
Recurrent anterior shoulder instability is a common traumatic injury, the main clinical manifestation of which is recurrent anteroinferior dislocation of the humeral head. The current follow-up study showed that the effect of arthroscopic Bankart repair is unreliable.
To evaluate the clinical efficacy of arthroscopy with subscapularis upper one-third tenodesis for treatment of anterior shoulder instability, and to develop a method to further improve anterior stability and reduce the recurrence rate.
Between January 2015 and December 2018, male patients with recurrent anterior shoulder instability were selected. One hundred and twenty patients had a glenoid defect < 20% and 80 patients had a glenoid defect > 20%. The average age was 25 years (range, 18–45 years). Patients with a glenoid defect < 20% underwent arthroscopic Bankart repair with a subscapularis upper one-third tenodesis. The patients with a glenoid defect > 20% underwent an arthroscopic iliac crest bone autograft with a subscapularis upper one-third tenodesis. All patients were assessed with Rowe and Constant scores.
The average shoulder forward flexion angle was 163.6° ± 8.3° and 171.8° ± 3.6° preoperatively and at the last follow-up evaluation, respectively. The average external rotation angle when abduction was 90° was 68.4° ± 13.6° and 88.5° ± 6.2° preoperatively and at the last follow-up evaluation, respectively. The mean Rowe scores preoperatively and at the last follow-up evaluation were 32.6 ± 3.2 and 95.2 ± 2.2, respectively (P < 0.05). The mean Constant scores preoperatively and at the last follow-up evaluation were 75.4 ± 3.5 and 95.8 ± 3.3, respectively (P < 0.05). No postoperative dislocations were recorded by the end of the follow-up period.
Arthroscopy with subscapularis upper one-third tenodesis was effective for treatment of recurrent anterior shoulder instability independent of the size of the glenoid bone defect, enhanced anterior stability of the shoulder, and did not affect postoperative range of motion of the affected limb.
Core Tip: Arthroscopy combined with subscapularis upper one-third tenodesis was effective for treatment of recurrent anterior shoulder instability independent of the size of the glenoid bone defect, enhanced anterior stability of the shoulder, and did not affect the postoperative range of motion of the affected limb.
- Citation: An BJ, Wang FL, Wang YT, Zhao Z, Wang MX, Xing GY. Arthroscopy with subscapularis upper one-third tenodesis for treatment of recurrent anterior shoulder instability independent of glenoid bone loss. World J Clin Cases 2022; 10(25): 8854-8862
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/8854.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.8854
Recurrent anterior shoulder instability is a common traumatic injury; the main clinical manifestation of which is recurrent anteroinferior dislocation of the humeral head. In the process of dislocation, the impact between the humeral head and the anteroinferior glenoid can lead to injury of the anterior glenoid labial ligament complex (Bankart lesion), and even an anterior labroligamentous periosteal sleeve avulsion (ALPSA). In some patients, the posterolateral collision between the glenoid and the humeral head in the process of recurrent dislocation may result in a bony glenoid defect (bony Bankart injury) and bone injury of the humeral head (Hill-Sachs injury), which increases the probability of re-dislocation. In recent years, the treatment of recurrent anterior shoulder instability has focused on labrum tear repair and bony structure reconstruction, which enhance the anterior stability of the shoulder. A number of studies have reported that arthroscopic surgery achieves satisfactory results[1,2]. Currently, a labrum repair is generally performed in patients with a glenoid bone defect < 20% and an on-track Hill-Sachs injury. Anterior glenoid bone defects > 20% and off-track Hill-Sachs injuries should be treated with glenoid bone grafting (Latarjet surgery and iliac bone grafting) or the remplissage technique[3,4]. A follow-up study showed that the effect of arthroscopic Bankart repair is unreliable, perhaps because the anterior labrum contracture was incompletely resolved due to repeated dislocation over a long period of time[5]. The blocking force of arthroscopic anterior labrum repair is insufficient, and cannot prevent anterior dislocation of the shoulder. Therefore, the stability and function of the shoulder cannot be improved after a labrum repair. A review of the literature showed that subscapularis upper one-third tenodesis fixed anterior to the scapular glenoid prevents re-dislocation of the shoulder and enhances stability of the shoulder[6]. Therefore, we repaired the torn labrum or reconstructed the bony structure, but also enhanced the anterior shoulder stability with subscapularis tenodesis augmentation in the treatment of recurrent anterior shoulder instability.
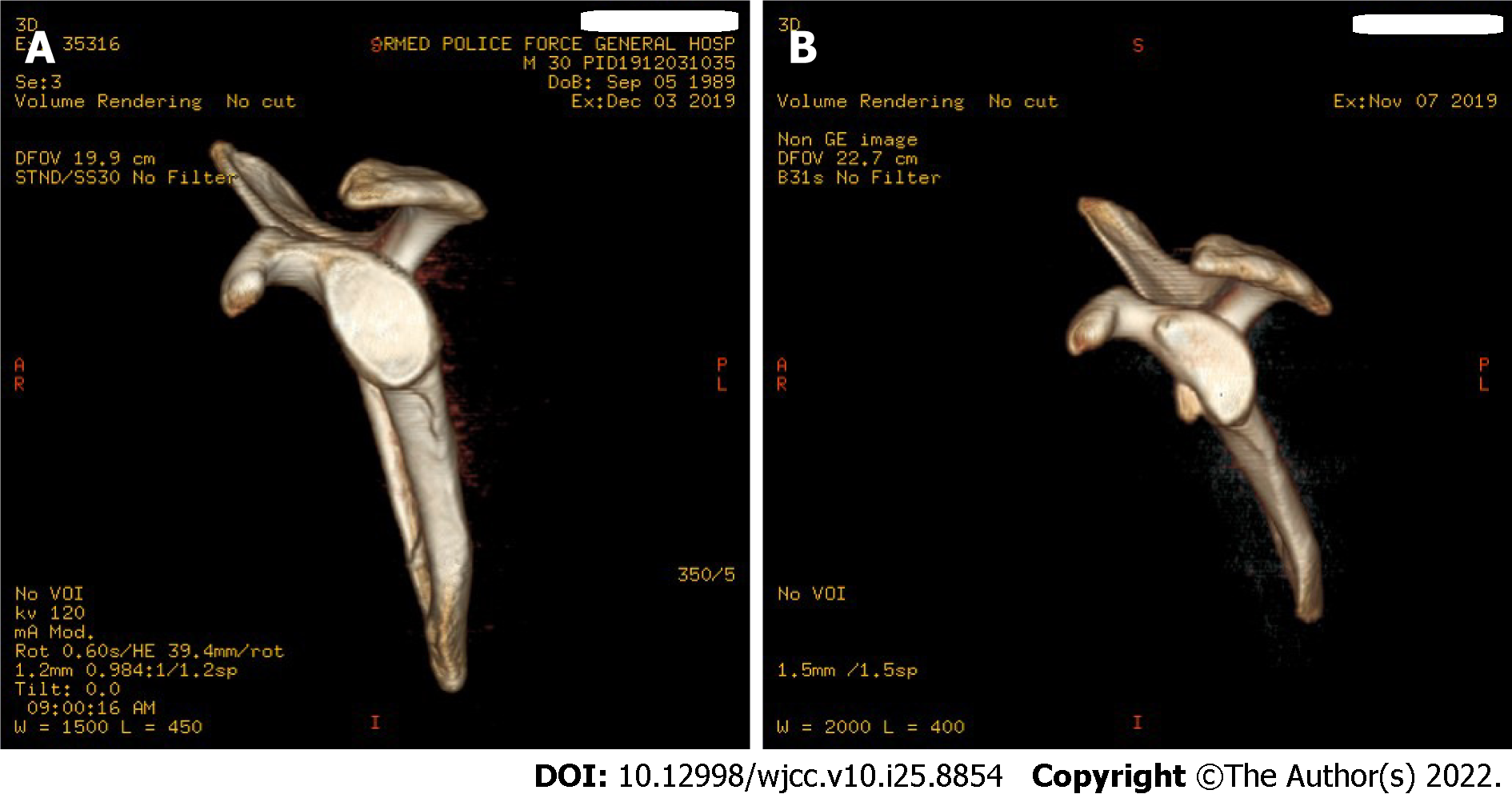
From July 2016 to December 2018, 200 male patients who were diagnosed with recurrent anterior shoulder instability and underwent arthroscopic surgery were enrolled. The average age at the time of surgery was 25 years (range, 18–45 years; Table 1). The inclusion criteria were as follows: (1) Anterior shoulder dislocations > 3; (2) Preoperative imaging examination confirmed anterior and inferior labrum tears or an accompanying bony defect; and (3) No stable operation was performed before participating in this study. The exclusion criteria were as follows: (1) Previous surgery of the affected shoulder; (2) Concomitant rotator cuff tear; (3) Concomitant remplissage or superior labrum anterior to posterior repair; (4) Concomitant epilepsy or psychiatric disease; and (5) Incomplete radiological or clinical follow-up. All patients had anteroposterior and oblique radiographs of the shoulder, a computed tomography (CT) scan, and magnetic resonance imaging (MRI) examination before surgery. MRI angiography was feasible for patients without an obvious labrum tear. Preoperative plain radiographs and CT scans with the population, intervention, control, and outcomes surface area measurement were obtained to accurately determine the glenoid deficit (Figure 1). This study was approved by the Institutional Review Board.
| Parameters | Glenoid defects < 20% | Glenoid defects > 20% | Entire series |
| Number | 120 | 80 | 200 |
| Age (yr) | 23 (18-40) | 26 (18-45) | 25 (18-45) |
| Follow-up (mo) | 36 (24-48) | 36 (26-60) | 36 (24-60) |
| Dominant arm (right/left) | 78/42 | 43/37 | 121/79 |
| Dislocation before surgery | 5 (3-10) | 10 (3-50) | 6 (3-50) |
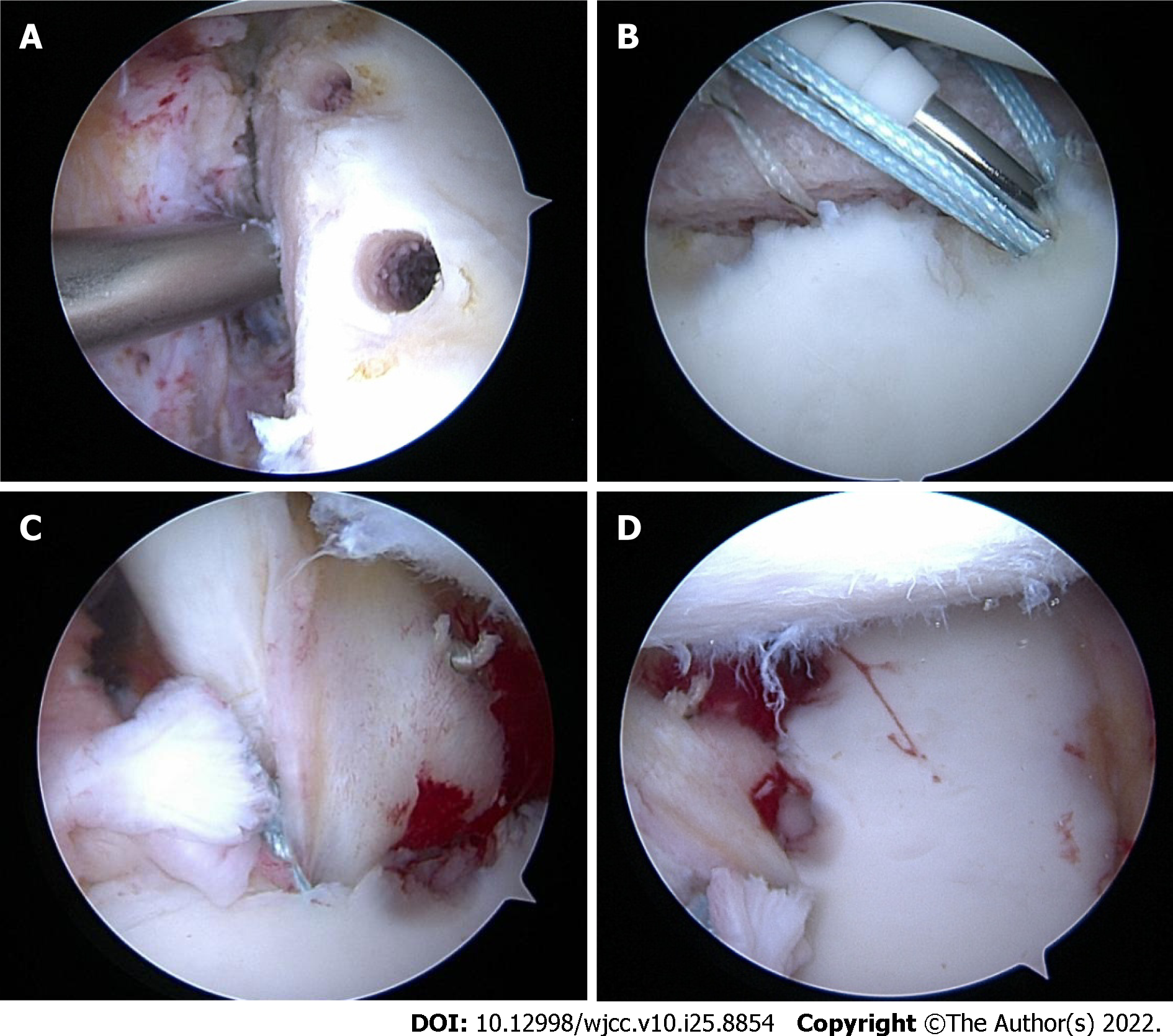
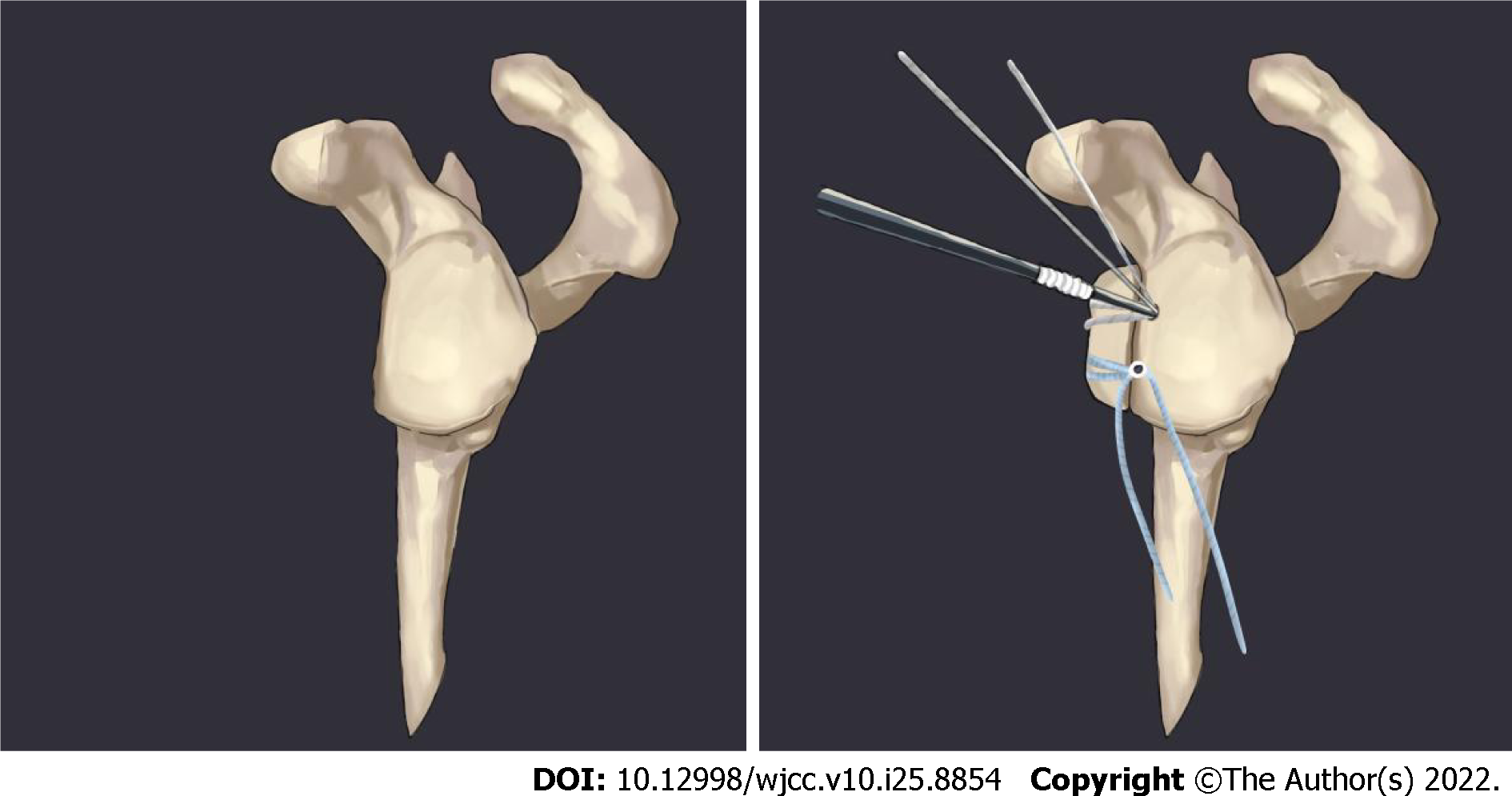
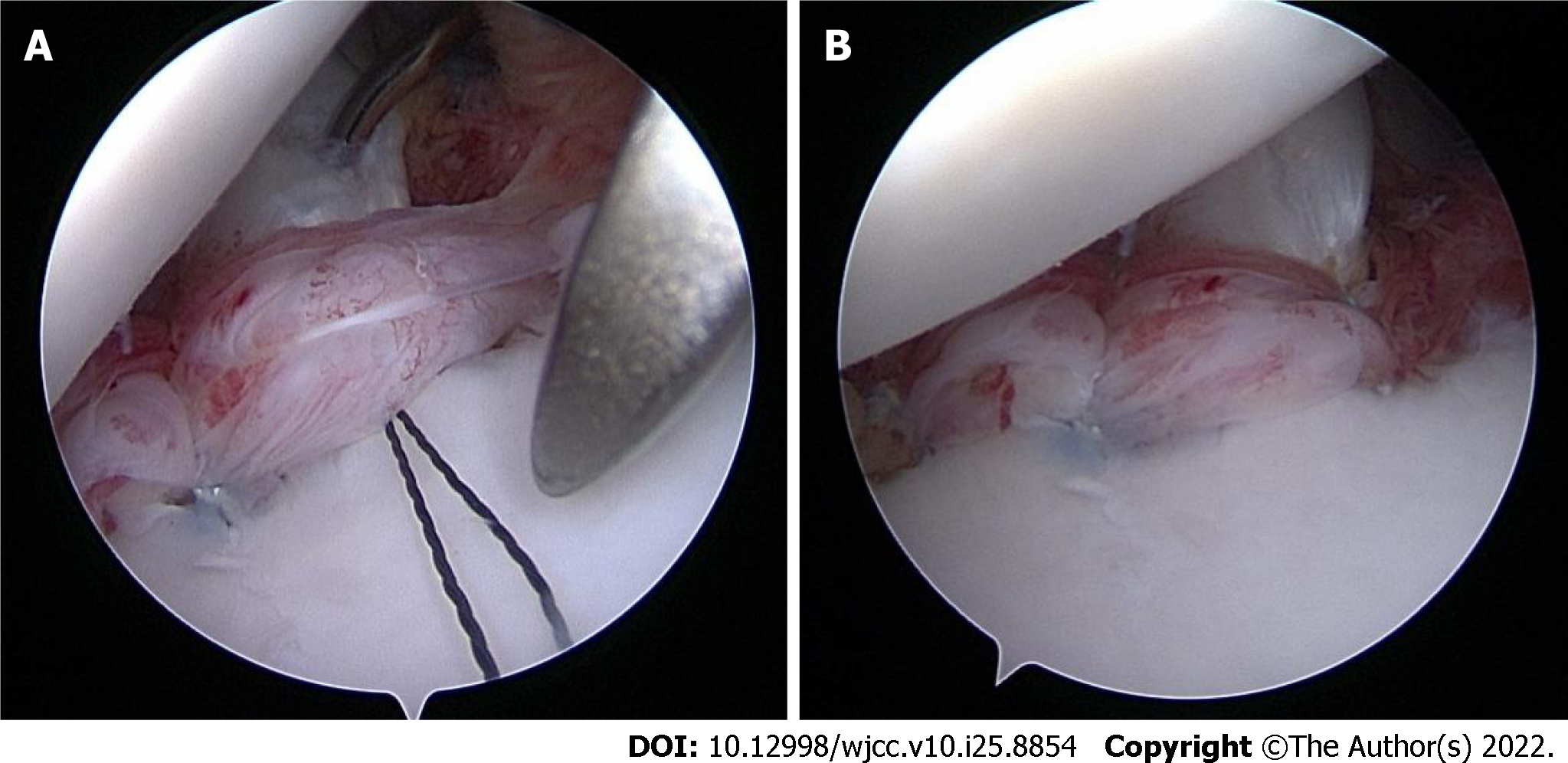
The arthroscopic procedure was performed under locoregional anesthesia with the patient in the lateral decubitus position. Standard posterior, anterior and anterosuperior approaches were used. The posterior approach of the shoulder was established (2 cm down and 1 cm inward at the posterolateral angle of the acromion). Labrum tears were noted in all cases. Some patients also had ALPSA injuries; the anterior labrum had disappeared and presented as clip-like changes. The area of the glenoid defect and whether the trajectory of the humeral head was on- or off-track were evaluated intraoperatively. Anterior and anterosuperior approaches were established. Pre-positioned Pushlock anchors were arranged approximately 45° oblique to the coronal plane and perpendicular to the longitudinal axis of the labrum for patients with a glenoid defect < 20%. The labrum and the capsule were sutured with a threading device, and the suture line was pressed by Pushlock anchors to adjust the tension. An iliac crest bone autograft, 2.0 cm × 1 cm × 1 cm in size, from the ipsilateral anterior superior iliac spine was used for patients with a glenoid defect > 20%. Two 2.9-mm Pushlock anchor holes were drilled at the 3 and 5 o’clock positions in the left shoulder. A 3.0-mm suture anchor was drilled at the 4 o’clock position in the left shoulder, 1 cm from the upper edge of the glenoid surface. The bone graft was implanted through the anterosuperior approach. The cancellous bone surface of the bone block was attached to the defect surface of the glenoid, and the double anchor tail lines were fixed by two Pushlock anchors (Figures 2 and 3). The upper one-third of the subscapularis tendon was sutured and fixed at the 2 o'clock position in the left shoulder with both methods (Figure 4).
After surgical repair, the shoulder was strictly immobilized in a sling for 2 wk in patients without bone grafts and for 4 wk in patients with bone grafts. The patients began passive range-of-motion (ROM) exercises to increase joint mobility in the 3rd week postoperatively in patients without bone grafts and the 5th week postoperatively in patients with bone grafts. At 6-8 wk postoperatively, physiotherapy focused on recovery of full ROM in the shoulder. Strengthening exercises began 10-12 wk postoperatively. Full ROM of the shoulder was permitted 12 wk postoperatively. All sports activities were allowed 6 mo postoperatively.
Statistical analysis was performed using SPSS 23.0 software. Measurement data are shown as the mean ± SD. The Rowe and Constant scores of patients were normally distributed before and at the last follow-up evaluation. Paired t-tests were used for quantitative data. Two-sided P values were calculated and the level of significance was defined as P < 0.05.
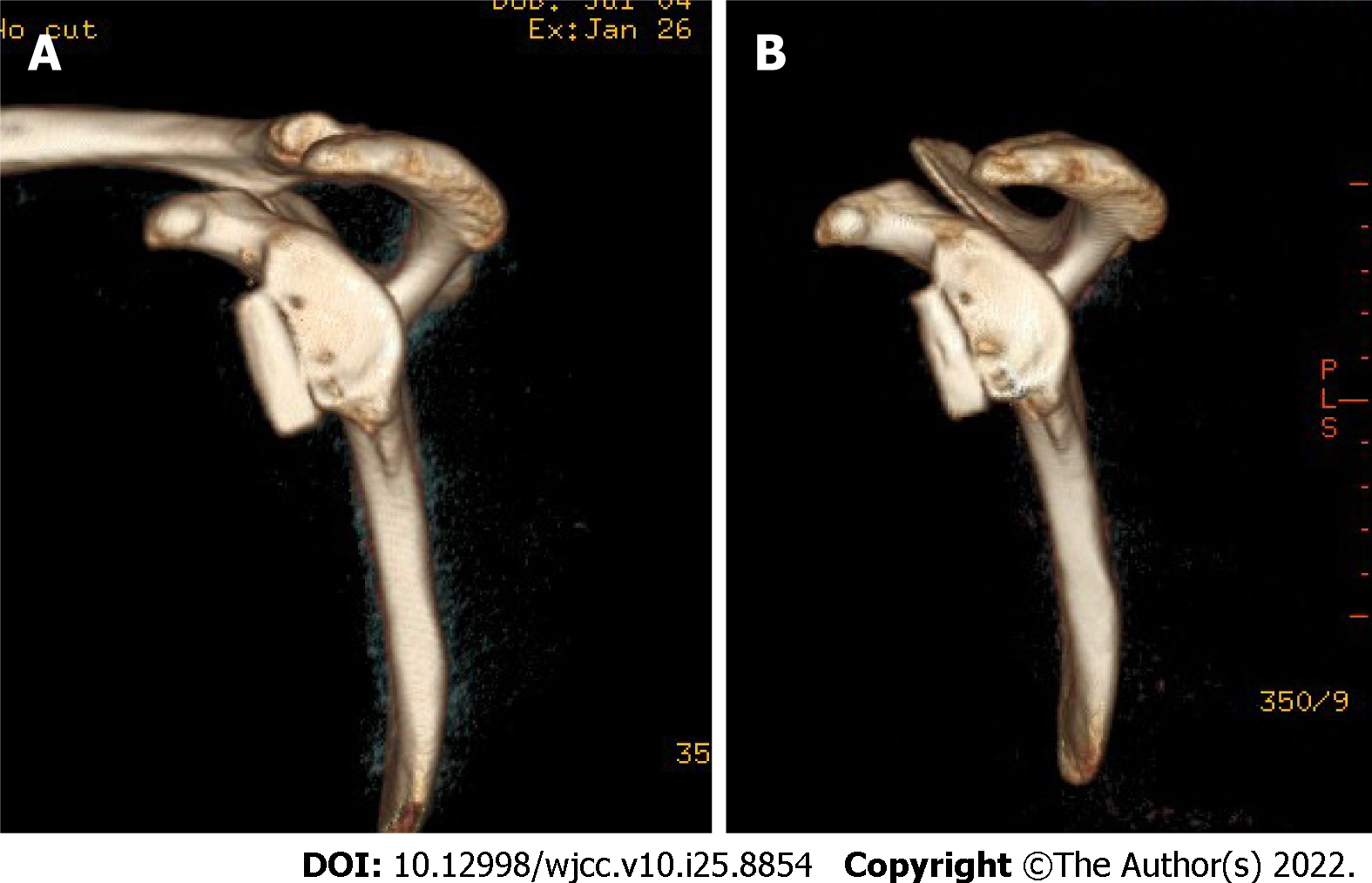
Patients were followed for an average of 3 years (2-5 years). Clinical efficacy was analyzed based on the patient’s chief complaint, ROM of the shoulder, X-ray findings, and CT three-dimensional reconstruction (Figure 5). Pre- and postoperative shoulder function was evaluated by ROM, and Constant and Rowe scores. The average angle of shoulder forward flexion before surgery and at the last follow-up evaluation was 163.6° ± 8.3° and 171.8° ± 3.6°, respectively. The average angle of external rotation with the arm in abduction before surgery and at the last follow-up evaluation was 68.4° ± 13.6° and 88.5° ± 6.2°, respectively. The mean Constant scores before and at the last follow-up evaluation were 75.4 ± 3.5 and 95.8 ± 3.3, respectively, which were significantly different from the before-treatment score (P < 0.05). The mean Rowe scores before and at the last follow-up evaluation were 32.6 ± 3.2 and 95.2 ± 2.2, respectively, which were significantly higher than the before-treatment score (P < 0.05; Table 2). No recurrent dislocations occurred through the final follow-up evaluation.
| Preoperative | Follow-up | P value | |
| Forward flexion | 163.6 ± 8.3 | 171.8 ± 3.6 | < 0.005 |
| ER | 68.4 ± 13.6 | 88.5 ± 6.2 | < 0.005 |
| Constant score | 75.4 ± 3.5 | 95.8 ± 3.3 | < 0.005 |
| Rowe score | 32.6 ± 3.2 | 95.2 ± 2.2 | < 0.005 |
Arthroscopic single labrum repair for recurrent anterior shoulder instability achieves good results; however, follow-up evaluations have shown that there is a high probability of recurrent shoulder re-dislocation[7]. The risk factors for re-dislocation of the shoulder after arthroscopic labrum repair include ALPSA injuries, Hill-Sachs injuries, and anterior glenoid bone defects[8]. In 2015 Klungsøyr et al[9] reported that arthroscopy with upper one-third subscapularis augmentation had satisfactory efficacy in the treatment of recurrent anterior shoulder instability. The recurrence rate was < 2.5%, and the external rotation function of the shoulder was not affected at the time of short-term follow-up evaluation because upper one-third subscapularis augmentation fixation increased the contact surface between the capsule and bone. Maiotti and Massoni[6] conducted biomechanical studies in cadavers and showed that subscapularis augmentation acts as a barrier to the eccentric movement of the humeral head. In a multicenter study, Taverna et al[10] confirmed that Bankart injury repair with the subscapularis technique had good results, a low failure rate, and no impact on external rotation of the shoulder. Therefore, for patients who do not require bone grafting, the binding force of arthroscopic Bankart repair is insufficient for the humeral head. Inferior labrum and capsule augmentation cannot effectively prevent recurrent dislocation of the shoulder, thus the recurrence rate is high[11]. Several studies have shown that patients with recurrent anterior shoulder instability have severe anterior labrum tears; some patients even have an absent anterior labrum and the anterior capsule is clearly loosened[12]. Therefore, it is difficult to obtain sufficient stability with the Bankart repair alone, which leads to failure and recurrence. The subscapularis has an important role in maintaining forward stability of the shoulder. Suturing part of the subscapularis tendon and joint capsule to the anterior labrum effectively enhances the anterior blocking effect of the shoulder and does not have a significant impact on rotation of the shoulder[13,14]. We observed a reduction in movement of the humeral head during arthroscopic subscapular augmentation. Therefore, it is clear that contraction of some subscapular muscles has a role in blocking forward movement of the humeral head. Postoperative functional exercise will not affect rotation of shoulder, and no dislocations occurred in our study.
According to Ito et al[15], treatment of recurrent anterior shoulder instability should be based on the type of glenoid defect, the surface area as measured by CT scans, and repair of on-track Hill-Sachs injuries with soft tissue. Remplissage or Latarjet technology is required for off-track Hill-Sachs injuries. Burkhart and De Beer[16] summarized the strategies for treatment of recurrent anterior shoulder instability as follows: (1) Glenoid defects < 20% in on-track Hill-Sachs injuries are repaired by Bankart arthroscopy; (2) Articular glenoid defects < 20% accompanied by off-track Hill-Sachs injuries are repaired by arthroscopy Bankart plus remplissage; and (3) Latarjet surgery is performed for glenoid defects > 20%. Latarjet surgery, iliac crest bone autografts, and distal tibial allografts are the most widely used methods for glenoid defects. Compared with other surgical methods, an iliac crest bone autograft is an anatomic repair that is more consistent with the normal structural relationship of the shoulder. Autogenous iliac bone does not elicit a rejection reaction, reduces damage to the subscapular muscle, and facilitates satisfactory bone healing; however, Latarjet surgery is a nonanatomical reconstruction, the combined tendon has a traction effect on the bone graft postoperatively, healing of the bone graft is affected, the normal anatomical structure of the shoulder is distorted, and whether there is a long-term impact on the normal movement of the shoulder is currently unknown. The main complications of Latarjet surgery are failure of fixation, poor position, displacement, absorption, and secondary osteoarthritis and axillary nerve injury[17-21]. A recent randomized controlled trial by Moroder et al[22] reported that iliac crest bone graft transfer results in similar clinical results as the Latarjet procedure, but glenoid bone grafting may have several potential advantages over the Latarjet procedure, including an ability to accommodate a greater degree of glenoid bone loss and reduced risk of convulsion-related graft failure in patients. Moreover, there is no internal fixation material in the glenoid bone grafting and bone absorption is less. Glenoid bone grafting is more anatomical without damaging the sternoclavicular arch structure. Finally, the operating time for glenoid bone grafting is short when compared with that of Latarjet surgery[23], and upper one-third subscapular augmentation further compresses the contact between the bone graft and the glenoid, which is conducive to bone healing without affecting rotation of the shoulder.
Hill-Sachs injuries have recently received increased attention. The mechanism underlying Hill-Sachs injuries is a collision between the anterior-inferior aspect of the scapular glenoid and the posterior-superior aspect of the humeral head during anterior dislocation of the shoulder, resulting in a bony defect of the posterior-superior aspect of the humeral head and the anterior-inferior aspect of the scapular glenoid. Injury to the labrum or even a bony defect frequently coexist with Hill-Sachs injuries[24]. The most commonly used method for this type of injury is the remplissage procedure. It is believed that the remplissage procedure can effectively limit engagement of the glenoid and humeral head during external rotation and abduction of the shoulder, thereby reducing the occurrence of anterior instability of the humeral head. It has been reported that the remplissage procedure will cause limited external rotation of the shoulder[25]. Whether or not the bone graft was implanted, we used arthroscopic composite partial upper one-third subscapular augmentation instead of the remplissage procedure, which also achieved satisfactory results without affecting recovery of shoulder function. Historical surgery, such as the Putty–Platt and Magnuson–Stack procedures, involves entire tendon shortening, thus interfering with external rotation. In contrast, our method only involved the stretched portion of the subscapularis tendon upper border, thus leaving the middle and inferior subscapularis in the normal, anatomic position[26,27].
Therefore, the effect of arthroscopy with upper one-third subscapularis augmentation in the treatment of recurrent anterior shoulder instability is satisfactory, and compared with simple labrum repair, this method is more reliable, the recurrence rate is lower, and rotation of the shoulder is not affected. In addition, the postoperative rehabilitation process is equally important. It is necessary to resume physical activity when the shoulder joint is fully restored to the normal ROM; the entire rehabilitation cycle lasts approximately 6 mo.
Arthroscopy combined with subscapularis upper one-third tenodesis was shown to be effective for treatment of recurrent anterior shoulder instability independent of the size of the glenoid bone defect, enhanced the anterior stability of the shoulder, and did not affect the postoperative range of motion of the affected limb. This method is simple, and the selection of patients, proficiency of the surgical procedure, and postoperative functional exercises are the key to the success of the operation.
Recurrent anterior shoulder instability is a common traumatic injury, the main clinical manifestation of which is recurrent anteroinferior dislocation of the humeral head. The current follow-up study showed that the effect of arthroscopic Bankart repair is unreliable.
To evaluate the clinical efficacy of arthroscopy with subscapularis upper one-third tenodesis in the treatment of anterior shoulder instability.
To seek a method to enhance anterior stability and reduce the recurrence rate.
Patients with a glenoid defect < 20% underwent an arthroscopic Bankart repair combined with a subscapularis upper one-third tenodesis. Arthroscopic iliac crest bone autograft for the patients with a glenoid defect > 20% underwent an arthroscopic iliac crest bone autograft combined with a subscapularis upper one-third tenodesis. All patients were assessed with Rowe and Constant scores.
The average shoulder forward flexion angle was 163.6° ± 8.3° and 171.8° ± 3.6° preoperatively and at the last follow-up evaluation, respectively. When abduction was 90°, the average external rotation angle was 68.4° ± 13.6° and 88.5° ± 6.2°, respectively. The mean Rowe scores preoperatively and at the last follow-up evaluation were 32.6 ± 3.2 and 95.2 ± 2.2, respectively (P < 0.05). The mean Constant scores were 75.4 ± 3.5 and 95.8 ± 3.3, respectively (P < 0.05). No postoperative dislocations were recorded by the end of the follow-up period.
Arthroscopy combined with subscapularis upper one-third tenodesis was shown to be effective for treatment of recurrent anterior shoulder instability independent of the size of the glenoid bone defect, enhanced the anterior stability of the shoulder, and did not affect the postoperative range of motion of the affected limb. This method is simple, and the selection of patients, proficiency of the surgical procedure, and postoperative functional exercises are the key to the success of the operation.
We decided not only to repair the torn labrum or reconstruct the bony structure, but also to enhance the anterior shoulder stability with subscapularis tenodesis augmentation in the treatment of recurrent anterior shoulder instability.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mastrantonakis K, Greece; Oommen AT, India S-Editor: Gao CC L-Editor: Kerr C P-Editor: Zhang YL
| 1. | Shields E, Mirabelli M, Amsdell S, Thorsness R, Goldblatt J, Maloney M, Voloshin I. Functional and imaging outcomes of arthroscopic simultaneous rotator cuff repair and bankart repair after shoulder dislocations. Am J Sports Med. 2014;42:2614-2620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Willemot LB, Elhassan BT, Verborgt O. Bony Reconstruction of the Anterior Glenoid Rim. J Am Acad Orthop Surg. 2018;26:e207-e218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | Fedorka CJ, Mulcahey MK. Recurrent anterior shoulder instability: a review of the Latarjet procedure and its postoperative rehabilitation. Phys Sportsmed. 2015;43:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Flinkkilä T, Sirniö K. Open Latarjet procedure for failed arthroscopic Bankart repair. Orthop Traumatol Surg Res. 2015;101:35-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Argintar E, Heckmann N, Wang L, Tibone JE, Lee TQ. The biomechanical effect of shoulder remplissage combined with Bankart repair for the treatment of engaging Hill-Sachs lesions. Knee Surg Sports Traumatol Arthrosc. 2016;24:585-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Maiotti M, Massoni C. Arthroscopic augmentation with subscapularis tendon in anterior shoulder instability with capsulolabral deficiency. Arthrosc Tech. 2013;2:e303-e310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Shibata H, Gotoh M, Mitsui Y, Kai Y, Nakamura H, Kanazawa T, Okawa T, Higuchi F, Shirahama M, Shiba N. Risk factors for shoulder re-dislocation after arthroscopic Bankart repair. J Orthop Surg Res. 2014;9:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Neoral P, Holibka R, Kalina R, Mlčůchová D, Gallo J. [Arthroscopic stabilisation of the shoulder. Risk factors for its failure]. Acta Chir Orthop Traumatol Cech. 2014;81:51-56. [PubMed] |
| 9. | Klungsøyr PJ, Guldal F, Vagstad T, Klungsøyr JA. A new subscapular sling operation to stabilize the shoulder. A cadaver study. J Exp Orthop. 2015;2:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Taverna E, D'Ambrosi R, Perfetti C, Garavaglia G. Arthroscopic bone graft procedure for anterior inferior glenohumeral instability. Arthrosc Tech. 2014;3:e653-e660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Gamulin A, Dayer R, Lübbeke A, Miozzari H, Hoffmeyer P. Primary open anterior shoulder stabilization: a long-term, retrospective cohort study on the impact of subscapularis muscle alterations on recurrence. BMC Musculoskelet Disord. 2014;15:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Maiotti M, Russo R, Zanini A, Schröter S, Massoni C, Bianchedi D. Arthroscopic Bankart repair and subscapularis augmentation: an alternative technique treating anterior shoulder instability with bone loss. J Shoulder Elbow Surg. 2016;25:898-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Russo R, Maiotti M, Taverna E. Arthroscopic bone graft procedure combined with arthroscopic subscapularis augmentation (ASA) for recurrent anterior instability with glenoid bone defect: a cadaver study. J Exp Orthop. 2018;5:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Maiotti M, Massoni C, Russo R, Schroter S, Zanini A, Bianchedi D. Arthroscopic Subscapularis Augmentation of Bankart Repair in Chronic Anterior Shoulder Instability With Bone Loss Less Than 25% and Capsular Deficiency: Clinical Multicenter Study. Arthroscopy. 2017;33:902-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Itoi E, Yamamoto N, Kurokawa D, Sano H. Bone loss in anterior instability. Curr Rev Musculoskelet Med. 2013;6:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1392] [Cited by in RCA: 1288] [Article Influence: 51.5] [Reference Citation Analysis (0)] |
| 17. | Malahias MA, Chytas D, Raoulis V, Chronopoulos E, Brilakis E, Antonogiannakis E. Iliac Crest Bone Grafting for the Management of Anterior Shoulder Instability in Patients with Glenoid Bone Loss: a Systematic Review of Contemporary Literature. Sports Med Open. 2020;6:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 18. | Jeong JY, Yoo YS, Kim T. Arthroscopic Iliac Bone Block Augmentation for Glenoid Reconstruction: Transglenoid Fixation Technique Using an All-Suture Anchor. Arthrosc Tech. 2020;9:e351-e356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Nzeako O, Bakti N, Bawale R, Singh B. Bone block procedures for glenohumeral joint instability. J Clin Orthop Trauma. 2019;10:231-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Ranalletta M, Tanoira I, Bertona A, Maignon G, Bongiovanni S, Rossi LA. Autologous Tricortical Iliac Bone Graft for Failed Latarjet Procedures. Arthrosc Tech. 2019;8:e283-e289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Hurley ET, Jamal MS, Ali ZS, Montgomery C, Pauzenberger L, Mullett H. Long-term outcomes of the Latarjet procedure for anterior shoulder instability: a systematic review of studies at 10-year follow-up. J Shoulder Elbow Surg. 2019;28:e33-e39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 152] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 22. | Moroder P, Schulz E, Wierer G, Auffarth A, Habermeyer P, Resch H, Tauber M. Neer Award 2019: Latarjet procedure vs. iliac crest bone graft transfer for treatment of anterior shoulder instability with glenoid bone loss: a prospective randomized trial. J Shoulder Elbow Surg. 2019;28:1298-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 112] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 23. | Hurley ET, Matache BA, Wong I, Itoi E, Strauss EJ, Delaney RA, Neyton L, Athwal GS, Pauzenberger L, Mullett H, Jazrawi LM; Anterior Shoulder Instability International Consensus Group. Anterior Shoulder Instability Part II-Latarjet, Remplissage, and Glenoid Bone-Grafting-An International Consensus Statement. Arthroscopy. 2022;38:224-233.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 73] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 24. | Provencher MT, Frank RM, Leclere LE, Metzger PD, Ryu JJ, Bernhardson A, Romeo AA. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg. 2012;20:242-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 202] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 25. | Brilakis E, Mataragas E, Deligeorgis A, Maniatis V, Antonogiannakis E. Midterm outcomes of arthroscopic remplissage for the management of recurrent anterior shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2016;24:593-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Maiotti M, Russo R, Zanini A, Castricini R, Castellarin G, Schröter S, Massoni C, Savoie FH 3rd. Bankart Repair With Subscapularis Augmentation in Athletes With Shoulder Hyperlaxity. Arthroscopy. 2021;37:2055-2062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 27. | Russo R, Maiotti M, Cozzolino A, Della Rotonda G, Guastafierro A, Massoni C, Viglione S. Arthroscopic Iliac Crest Bone Allograft Combined With Subscapularis Upper-Third Tenodesis Shows a Low Recurrence Rate in the Treatment of Recurrent Anterior Shoulder Instability Associated With Critical Bone Loss. Arthroscopy. 2021;37:824-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |