Published online Aug 16, 2022. doi: 10.12998/wjcc.v10.i23.8392
Peer-review started: March 30, 2022
First decision: May 30, 2022
Revised: June 13, 2022
Accepted: July 5, 2022
Article in press: July 5, 2022
Published online: August 16, 2022
Processing time: 124 Days and 6.1 Hours
Skin bronchogenic cysts are extremely rare congenital bronchocystic changes caused by the abnormal development of the trachea, bronchial trees or lung buds during the embryonic period. The first case of skin bronchogenic cysts was reported in 1945. Since then, this disease has attracted increasing attention, but due to the low incidence, its pathogenesis is still not clear.
Here, we report another case of skin bronchogenic cysts with infection in a 64-year-old female patient. The patient had no symptoms for more than 60 years until her chest wall was recently found to be swollen, and she felt pain and discomfort. At the same time, secretions were found on the surface of the swelling. Color Doppler ultrasound examination showed abnormal echoes in the soft tissue under the frontal chest wall, suggesting the presence of cysts. Cytological puncture resulted in about 2 mL of pus and showed the presence of more acute inflammatory cells. The final clinical diagnosis was skin cyst with infection, and surgery was carried out. The pathological results obtained after surgery showed that the cystic wall was covered with column-like cilia epithelial cells, and the interstitial structure was partially inundated with inflammatory cells. After a variety of examinations and clinical diagnoses, we finally confirmed that the patient was suffering from bronchogenic cyst.
This article not only describes the case of an elderly patient with rare skin bronchogenic cysts with infection but also provides a detailed and correct diagnosis and a successful treatment process, which is of great value for the diagnosis and treatment of the disease.
Core Tip: Skin bronchogenic cysts are a rare disease with low incidence, which is easy to be misdiagnosed. We have reported a case of bronchogenic cysts with infection in the frontal chest wall of a 64-year-old patient. Pain-accompanied secretions appeared in the patient’s frontal thoracic wall. Combined with color Doppler ultrasound examinations and cytological puncture examinations, we suggest that skin cysts with infections had been present before surgery. The diagnosis of skin bronchogenic cysts was confirmed by the final pathological results obtained after resection. We emphasize that the diagnosis of skin bron
- Citation: Ma B, Fu KW, Xie XD, Cheng Y, Wang SQ. Bronchogenic cysts with infection in the chest wall skin of a 64-year-old asymptomatic patient: A case report. World J Clin Cases 2022; 10(23): 8392-8399
- URL: https://www.wjgnet.com/2307-8960/full/v10/i23/8392.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i23.8392
Bronchogenic cysts are an extremely rare congenital disease that is caused by the abnormal development of the trachea, bronchial trees or lung buds during the embryonic period. The first case of skin bronchogenic cysts was reported by Seybold and Clagett[1] in 1945. Bronchogenic cysts may occur in various areas, such as the mediastinum[2], lungs[3], heart[4], stomach[5], peritoneum[6] and in other areas. The disease is more commonly diagnosed in childhood than in adulthood[7]. Furthermore, the incidence of this disease is approximately four times higher in males than in females[8]. In older female patients, fewer cases of skin bronchogenic cysts with infections are reported. Unfortunately, obvious clinical symptoms are absent, imaging examination does not provide any specific findings, the diagnosis of bronchogenic cysts before surgery is very difficult, and the rate of misdiagnosis is high[9]. To lay a foundation for future clinical work, we report the detailed diagnostic process and successful treatment of a 64-year-old female patient with skin bronchogenic cysts with infection. The timeline is shown in Table 1.
| Time | Information about the patient |
| September 24, 2020 | Admitted to our hospital |
| July 20, 2021 | Admitted to our hospital |
| July 20, 2021 | Received laboratory and imaging examinations |
| July 20, 2021 | Received ultrasonography |
| July 20, 2021 | Received cytological puncture |
| July 20, 2021 | The sac wall and necrosis tissue were completely removed |
| July 23, 2021 | Pathological results confirmed skin bronchogenic cysts |
| July 28, 2021 | Debridement and suture surgery |
| August 20, 2021 | Follow-up |
Chest wall swelling occurred for more than 60 years. Intermittent pain was accompanied by secretions for nearly half a year.
On September 24, 2020, a 64-year-old Chinese female patient visited our hospital presenting with intermittent pain. After careful outpatient examination, we thought that the patient may have a skin cyst and recommended surgery. At that time, the patient rejected surgery as a treatment option and received only oral antibiotics for treatment. For nearly half a year, the patient felt intermittent pain in the chest wall swellings and had secretions on the surface of the swellings. Therefore, the patient came to our hospital again for medical treatment on July 20, 2021.
The patient had no history of other diseases, such as diabetes, high blood pressure and heart disease. Moreover, she had no history of drug allergies.
The patient has gone through the menopause. She has one son and one daughter.
The patient’s vital signs were stable. We found a swelling of about 3 cm × 3 cm in the front chest wall near the thoracic bone handle protruding from the surface of the skin. The texture of the swelling was soft and caused slight pain upon pressure. Except for secretion in the skin around the swelling, no other obvious abnormalities were found, and the boundaries of the swelling were clear.
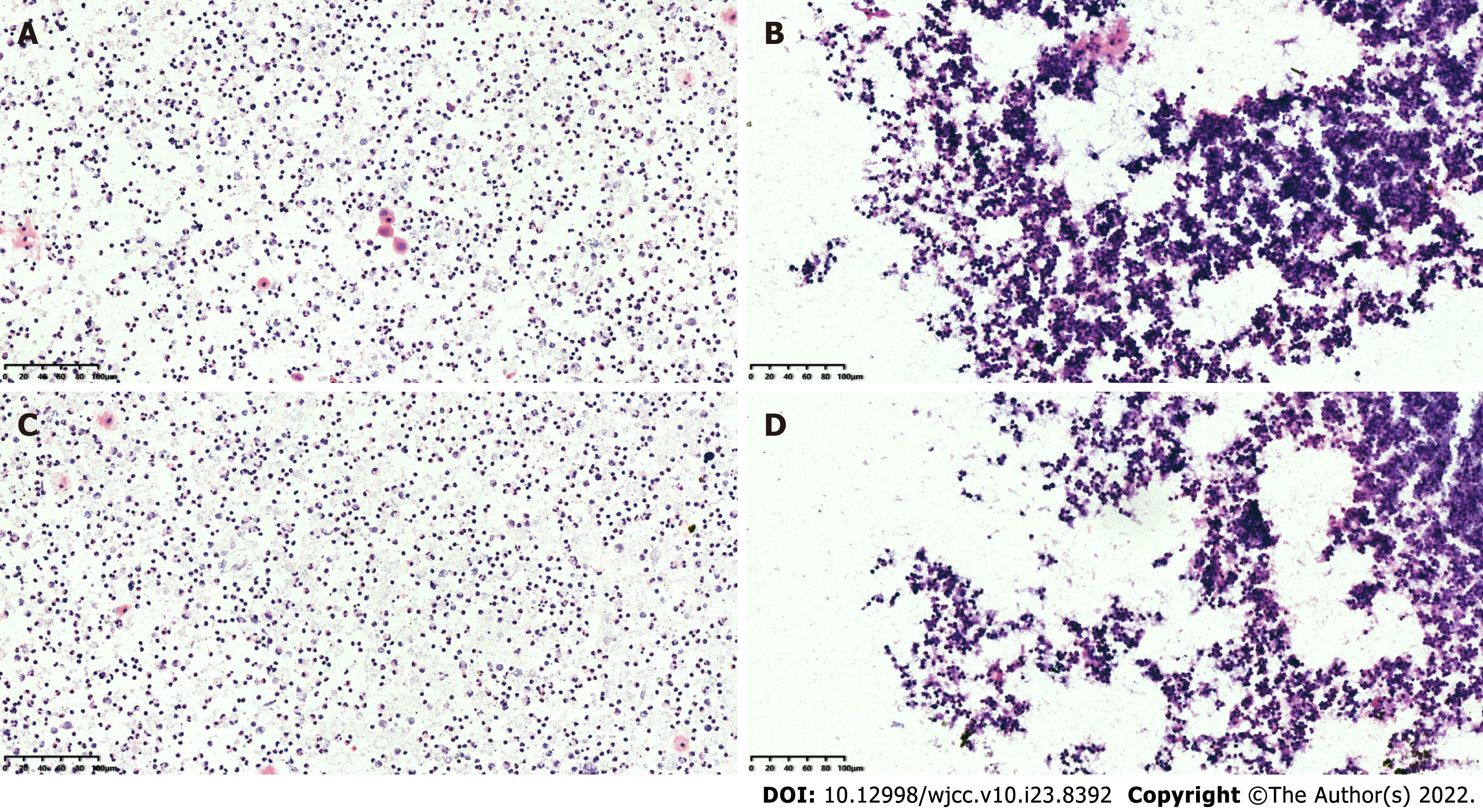
We further performed a fine-needle cytological puncture, which resulted in about 2 mL of pus. The results showed many acute inflammatory cells (Figure 1). Furthermore, other preoperative indicators, including blood biochemistry, complete blood count, HIV test and an electrocardiogram, were within the normal range. Based on the above results and findings, we speculate that the patient was most likely to have a skin cyst with infection.
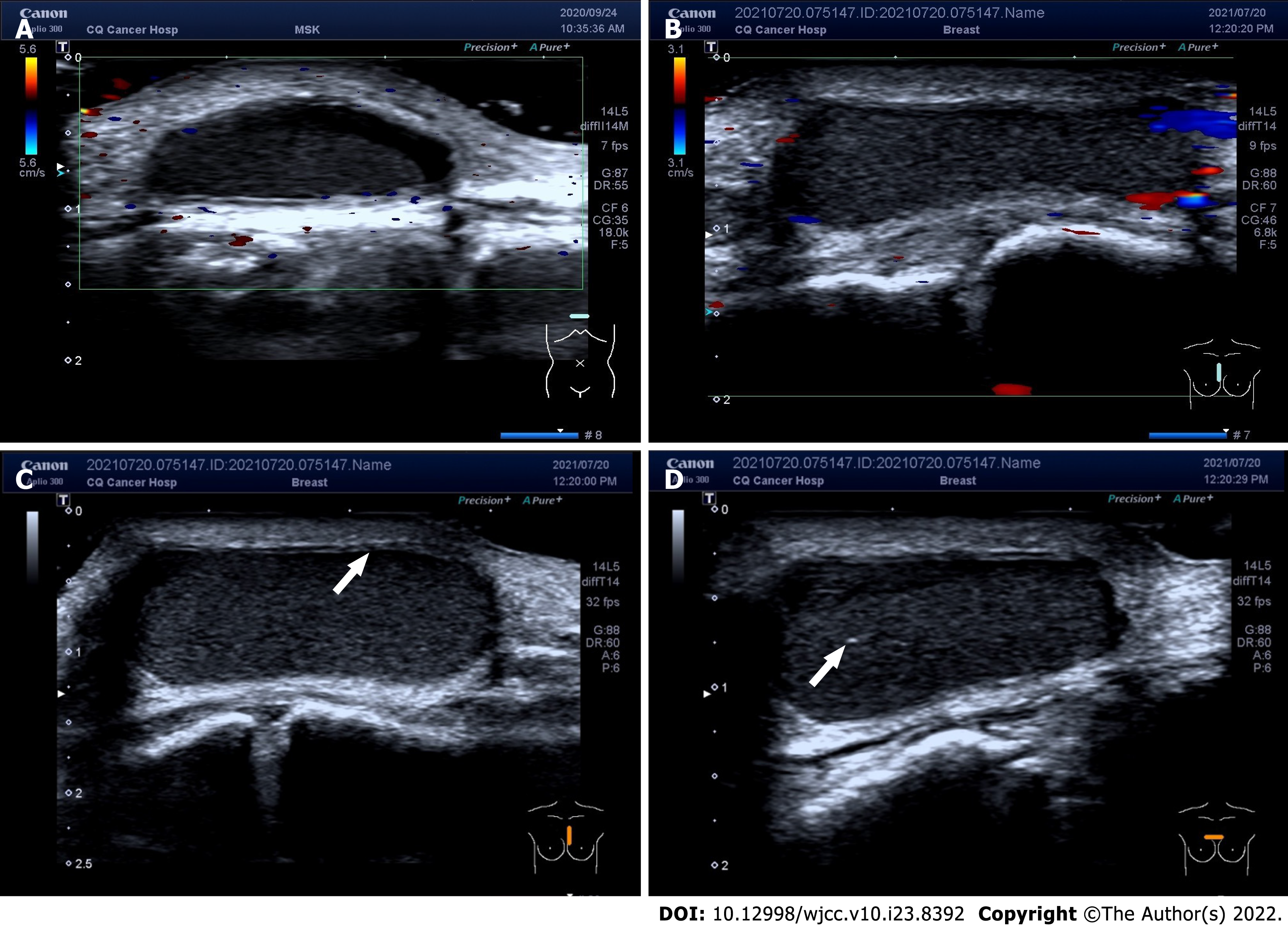
Color Doppler ultrasound examination revealed abnormal echoes in the soft tissue under the frontal chest wall, suggesting the presence of cysts in the corresponding area (Figure 2).
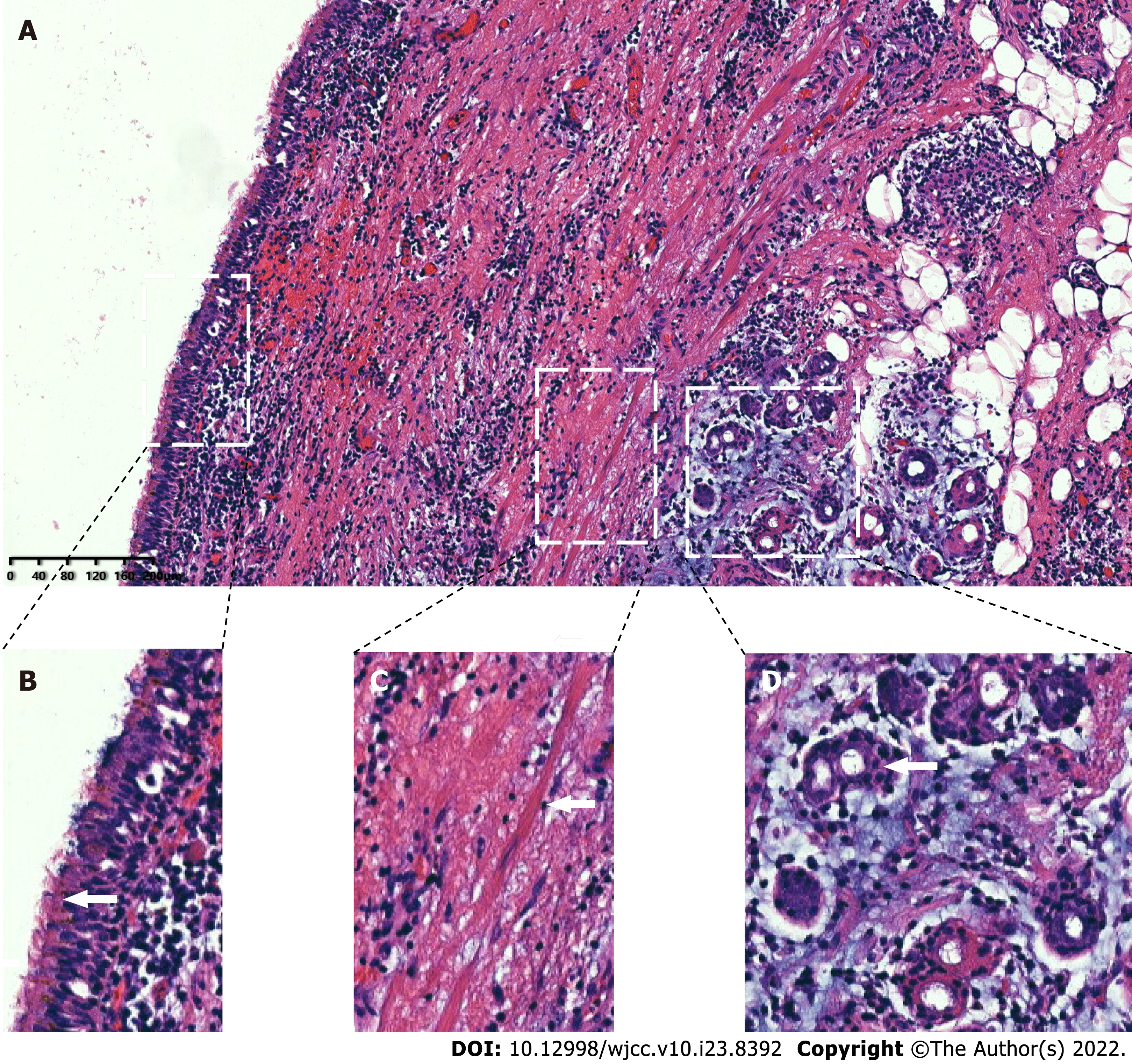
A large amount of yellow viscous liquid was found in the sample obtained from the patient. The pathological diagnosis was made based on the obtained tissue specimen (Figure 3). We found cyst lesions in the sample. The cystic wall was covered with column-like cilia epithelial cells. These cells had the same structure as the bronchus. At the same time, we found that the interstitial structure was partially infested with inflammatory cells, which were not reported in the usual histopathological findings of bronchogenic cysts. Combined with these results, the pathologists ultimately verified that the cyst of this patient was a bronchogenic cyst.
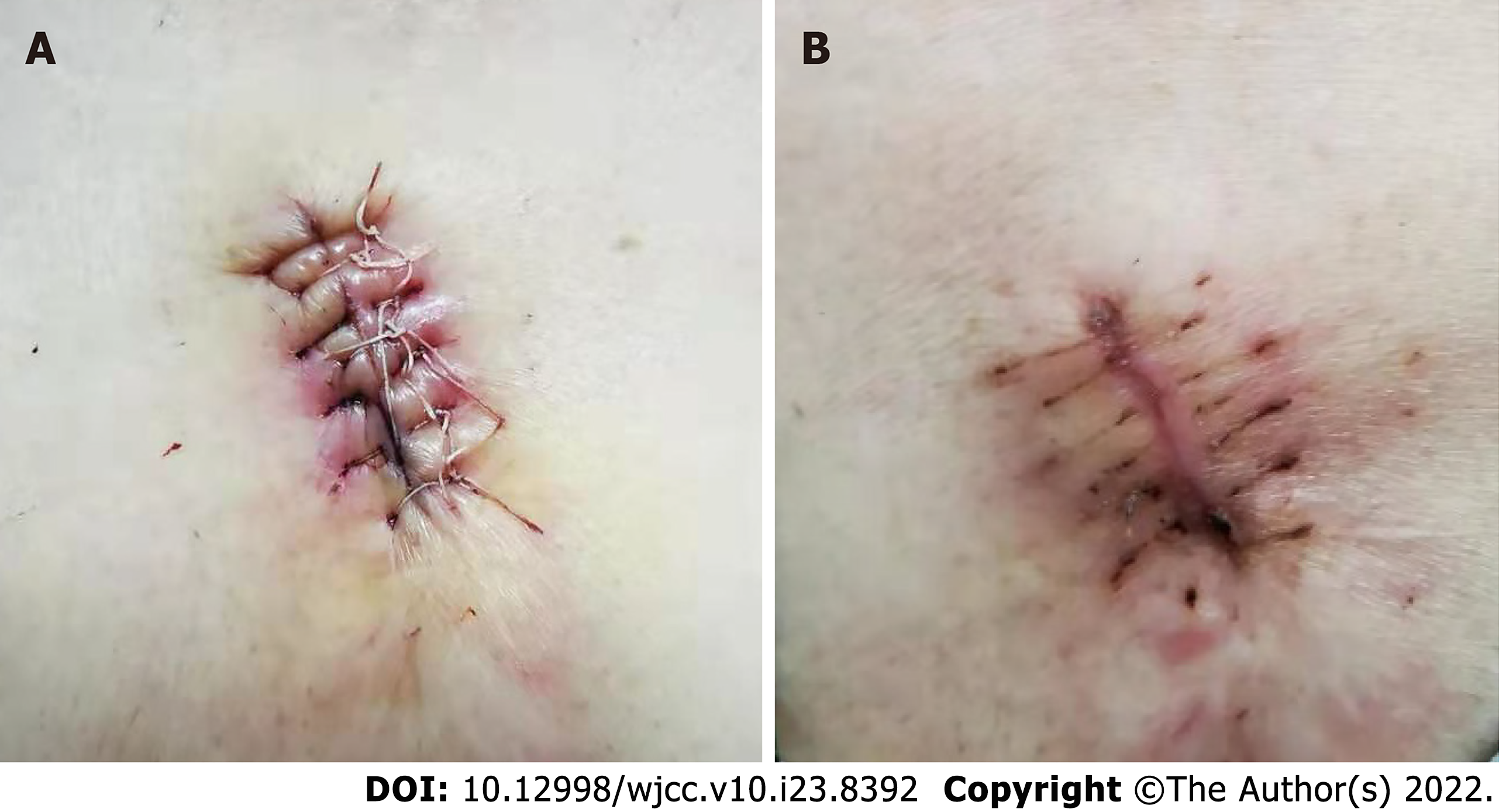
As the patient chose the complete removal of the cysts, we developed a personalized treatment plan in conjunction with our imaging examination. First, we cut open the skin at the location of the cysts and observed secretion of pus. Then, the sac wall and necrosis tissue were completely removed. We repeatedly rinsed the wound with hydrogen peroxide solution until no more obvious cyst wall, necrotic tissue and secretions were found. Then, the wound was rinsed again using normal saline. After that, the wound surface was filled with medical gauze, and we carefully observed the wound healing every day. After 8 d, the leakage of fluid from the trauma location was significantly reduced, and we observed bright red granulation tissue at the trauma location. Finally, we performed debridement and suture surgery again under local anesthesia. During the surgery, the secretions on the wound surface were thoroughly removed, and the cut edge and some inactivated tissues were trimmed to fit the skin well. As a result, the patient recovered well, and her symptoms disappeared completely (Figure 4).
The patient recovered well, and her symptoms disappeared completely within the following 30 d.
As bronchogenic cysts are a rare congenital disease, the pathogenesis of this disease is not yet known. Lots of medical doctors and researchers consider bronchogenic cysts to be congenital broncho saccharin changes caused by the abnormal development of trachea, bronchial trees or lung buds during the embryonic period[6,10]. Shah et al[7] reported a total of 86 cases of bronchogenic cysts, and about 74% of these patients were male. In these cases, the most common locations of subcutaneous bronchogenic cysts were thoracic bone incision (26), followed by neck (18), shoulder blade (15) and thoracic bone handle (13). Only 2 cases (2.3%, 2/86) were found in the front of the chest wall. In the present case, the cyst was in the frontal chest wall of the patient.
As previously reported, imaging generally shows no obvious clinical symptoms or specific signs. The clinical manifestations of the patient may be papules, cystic nodules, sinus tracts or secretions associated with the sinus tract[11]. Some patients even had no symptoms. It is worth noting that the patient reported in this case did not show any symptoms for up to 64 years. The cause of this phenomenon may have a lot to do with the location of the cyst and the limited size of the cyst (8-9 mm thick). For example, it has been reported that bronchial cysts located in the stomach can cause symptoms such as abdominal pain, nausea and vomiting in patients[5,12]. The clinical symptoms of benign masses in the skin layer are mostly the continuous growth of the mass, which affects the skin morphology. Due to these characteristics of bronchogenic cysts, the misdiagnosis rate of this disease is so high that it can delay the patients’ treatment processes.
In the case of the patient reported herein, the swelling was present for more than 60 years. Over time, the swelling grew at a very slow rate. Furthermore, no obvious clinical symptoms occurred in any stage of the disease. Therefore, this disease has not attracted the attention of the patient, and she did not seek urgent treatment. However, skin bronchogenic cysts can result in repeated breakages, infections and even malfunctions of the skin[13]. The current patient sought further treatment in our hospital as she had developed redness, intermittent pain and discomfort in recent months.
Pathological diagnosis is the gold standard for the diagnosis of bronchogenic cysts. Cysts are mainly located in the dermis and subcutaneous tissue. The cystic wall is composed of pseudo-complex respiratory cilia column epithelial cells and cup-shaped cells but sometimes contains smooth muscles and cartilage[14,15]. When the pathology cannot be clearly diagnosed, it has been suggested that the growth site of the lesion can be used as a criterion for the diagnosis of the disease. We performed a postoperative pathological diagnosis of the patient reported in this case. Combined with the patient’s symptoms, color Doppler ultrasound results, cytological puncture results and histopathological diagnosis, we confirmed that the disease was a bronchogenic cyst with infection.
This is an interesting case, as the patient did not show any symptoms for up to 64 years. Most regrettable in this case is that the preoperative diagnosis was not clear before the pathological diagnosis. Because of the rarity of bronchogenic cysts, the misdiagnosis rate of this disease is so high that it can delay the patients’ treatment processes. We emphasize that the possibility of bronchogenic cysts should be considered by doctors in the diagnosis and treatment of patients when imaging examination suggests fluid-containing cysts. Since the cystic wall is composed of pseudo-complex respiratory cilia column epithelial cells, cup-shaped cells, smooth muscles and cartilage[14,15], we recommend that medical researchers should be able to identify some markers specific to bronchial cysts by comparing genetic or metabolite differences between different cyst types. At the same time, considering the cost of treating patients, it is necessary to establish some simple and low-cost methods to accurately identify the corresponding special markers. This strategy can improve the doctor’s confidence in diagnosis and enable the patients to understand the disease in detail.
The suitable treatment of bronchogenic cysts is surgical excision in the early stage of the disease, and the cyst wall should be completely removed during surgery to prevent the recurrence of the disease[8]. We have selected 16 cases of chest wall cutaneous bronchial cysts, all of which were also treated by surgical excision (Supplementary Table 1). Among them, the first 2 cases were accompanied by infection. The patient in this case had repeatedly broken chest wall skin and secretions. The treatment process of this disease is different from that of other related diseases, such as sebum adeno cysts, epidermal cysts and cilia skin cysts[16]. On the other hand, the presence of infection further increases the difficulty of treating the disease. As shown in Supplementary Table 1, the first patient was treated with incision and drainage of the wound and oral antibiotics[17]. Then, the wound was allowed to heal spontaneously. As a result, a fistula formed in the wound. The second patient was treated with complete excision of the cyst[18]. However, complete excision of diseased tissue during inflammation often results in an excessively large excision, causing unnecessary damage to the patient. At the same time, in the presence of inflammation, the wound of the patient may become infected after the complete removal of the cyst. Therefore, we designed a personalized treatment plan for the patient based on our successful treatment strategy. As a result, the patient recovered well, and her symptoms disappeared completely.
This case report is of great value for the diagnosis and treatment of bronchogenic cysts as a rare disease. This successful experience allows improving the preoperative diagnosis and develops a personalized treatment plan for the patient. Furthermore, it is helpful to improve our understanding of the disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abdul Aziz JM, Iraq; Esch M, Germany S-Editor: Xing YX L-Editor: Filipodia P-Editor: Xing YX
| 1. | Seybold WD, Clagett OT. Presternal Cyst: Report of a Case. J Thorac Surg. 1945;14:217-220. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 14] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Tan GJS, Ooi WM, Law RHF, Nardini M. Robotic pericardial patch repair of the bronchus intermedius after bronchogenic cyst removal. Interact Cardiovasc Thorac Surg. 2018;26:711-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Kosar A, Tezel C, Orki A, Kiral H, Arman B. Bronchogenic cysts of the lung: report of 29 cases. Heart Lung Circ. 2009;18:214-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Park J, Cho GY, Park KH, Oh IY. Intracardiac bronchogenic cyst: report of a growing lesion. Circulation. 2014;130:1107-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | He WT, Deng JY, Liang H, Xiao JY, Cao FL. Bronchogenic cyst of the stomach: A case report. World J Clin Cases. 2020;8:1525-1531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Chen HY, Fu LY, Wang ZJ. Ileal bronchogenic cyst: A case report and review of literature. World J Clin Cases. 2018;6:807-810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Shah SK, Stayer SE, Hicks MJ, Brandt ML. Suprasternal bronchogenic cyst. J Pediatr Surg. 2008;43:2115-2117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Pul N, Pul M. Bronchogenic cyst of the scapular area in an infant: case report and review of the literature. J Am Acad Dermatol. 1994;31:120-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Tan KK, Nandini CL, Ho CK. A case of gastric bronchogenic cyst in Singapore with multiple intrigues. ANZ J Surg. 2010;80:286-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Tu C, Zhu J, Shao C, Mao W, Zhou X, Lin Q, Li Z, Zhang J, Zhou Q, Chen W. Gastric bronchogenic cysts: A case report and literature review. Exp Ther Med. 2016;11:1265-1270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 11. | Sun J, Yuan T, Deng H. Cutaneous bronchogenic cyst in the left scapular region of a boy. World J Pediatr. 2014;10:365-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Sun B, Wang AK, Chen H, Qian BL, Yi XK, Jiang Y, Li Q, Fu WG, Li J. Bronchogenic cyst of the stomach: A case report and literature review. Exp Ther Med. 2020;20:166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Tanita M, Kikuchi-Numagami K, Ogoshi K, Suzuki T, Tabata N, Kudoh K, Suetake T, Takahashi T, Tagami H. Malignant melanoma arising from cutaneous bronchogenic cyst of the scapular area. J Am Acad Dermatol. 2002;46:S19-S21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Kim DH, Kim HK, Lee JW, Lee HI, Park KY, Li K, Seo SJ, Hong CK, Song KY. A case of cutaneous bronchogenic cyst presenting with lymphoid follicles. Ann Dermatol. 2011;23:392-395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Perrot P, Lescour V, Jossic F, Barbarot S, Duteille F. [A rare congenital lesion: bronchogenic cyst. Case report and review of the literature]. Ann Chir Plast Esthet. 2013;58:263-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Avalos P, García-Hernández MJ, Ríos JJ, Moreno D, Camacho F. [Cutaneous bronchogenic cyst]. Actas Dermosifiliogr. 2005;96:186-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Carden C, Dykes E, Pollock AM. An unusual midline swelling--case report of a cutaneous bronchogenic cyst. Eur J Pediatr Surg. 2008;18:345-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Shilova M, Wong MCL, Davies J, Kimble R. A bronchogenic cyst presenting as a presternal abscess. J Pediat Surg Case R. 2020;63:101653. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |