Published online Aug 16, 2022. doi: 10.12998/wjcc.v10.i23.8323
Peer-review started: February 27, 2022
First decision: April 8, 2022
Revised: May 25, 2022
Accepted: July 11, 2022
Article in press: July 11, 2022
Published online: August 16, 2022
Processing time: 155 Days and 4 Hours
Femoral and tibial stress injuries are commonly found in long distance running athletes. Stress fractures have rarely been reported in athletes performing high intensity interval training (HIIT) exercise. The objective of this study was to report a case of a patient who presented with medial tibial stress syndrome and femoral neck stress fracture after performing HIIT exercises.
A 26 year old female presented with bilateral medial tibial pain. She had been performing HIIT exercise for 45 min, five times weekly, for a seven month period. Her tibial pain was gradual in onset, and was now severe and worse on exercise, despite six weeks of rest. Magnetic resonance imaging (MRI) revealed bilateral medial tibial stress syndrome. As she was taking norethisterone for birth control, a dual energy X-ray absorbitometry scan was performed which demonstrated normal bone mineral density of her lumbar spine and femoral neck. She was managed conservatively with analgesia and physiotherapy, but continued to exercise against medical advice. She presented again six months later with severe right hip pain. MRI of her right hip demonstrated an incomplete stress fracture of her subtrochanteric region. Her symptoms resolved with strict rest and physiotherapy.
HIIT may cause stress injury of the tibia and femur in young individuals.
Core Tip: Stress injuries of the femur and tibia commonly occur in long distance runners, but have rarely been reported in individuals performing high intensity interval training (HIIT). An index of suspicion for stress injury, and proper investigation is required for patients presenting with hip or tibial pain following HIIT.
- Citation: Tan DS, Cheung FM, Ng D, Cheung TLA. Femoral neck stress fracture and medial tibial stress syndrome following high intensity interval training: A case report and review of literature. World J Clin Cases 2022; 10(23): 8323-8329
- URL: https://www.wjgnet.com/2307-8960/full/v10/i23/8323.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i23.8323
High Intensity Interval Training (HIIT) has become increasingly popular as a method of exercise. HIIT involves alternating periods of relatively intense work and recovery. HIIT exercises may be subdivided into aerobic exercises e.g., running and cycling, and body weight/resistance exercises. HIIT programs can vary greatly and combine both types of exercise[1]. The incidence and type adverse events related to HIIT exercise are not well known, with isolated case reports described in the literature. However, injury rates may be under-reported and higher than previously realised[2].
Medial tibial stress syndrome (MTSS), also known to the layman as ‘shin-splints’, is exercise-induced pain over the anterior tibia which may lead to stress fracture. MTSS is common in long distance runners and military personnel[3]. Femoral neck stress fractures (FNSF) are an uncommon but potentially disabling cause of athletes presenting with exercise-related hip and groin pain. The commonest causative sports are marathon and long-distance running. Outcomes are considerably worse for fractures with a delay in diagnosis, and displacement[4].
This study reports a case of bilateral medial tibial stress syndrome, and subsequent femoral neck stress fracture, following prolonged high intensity interval training in a young female adult. Such a case has not previously been reported.
A 26 year old female presented in the outpatient clinic with bilateral tibial pain following HIIT. Continuation of exercise resulted in severe right groin pain six months later.
A 26 year old female presented with bilateral medial tibial pain. She had been performing HIIT exercise for 45 min, five times weekly, for a seven month period. Her tibial pain was gradual in onset, and was now severe and worse on exercise, despite six weeks of rest. The patient was unwilling to cease HIIT and continued to exercise against medical advice. She presented with severe right groin pain six months later.
There was no specific underlying disease.
The patient was taking norethisterone for birth control. She had previously had an open reduction and internal fixation of a right ankle fracture seven years previously and had made a full recovery.
On initial presentation the patient complained of pain in the anteromedial aspect of the middle third of both tibiae. There was tenderness bilaterally in these regions. Gait was normal and the patient was able to squat and tiptoe easily. Spine and bilateral hip, knee and ankle examination was within normal limits. There were no clinical features of rhabodomyolysis such as myalgia, muscle weakness or dark urine. She presented six months later with right groin pain. Range of motion in both hips was 135/135, adduction 35/35, abduction 45/45, internal rotation 10/15 (painful and reduced motion on the right).
Blood tests did not show any abnormality. Vitamin D level was within normal limits.
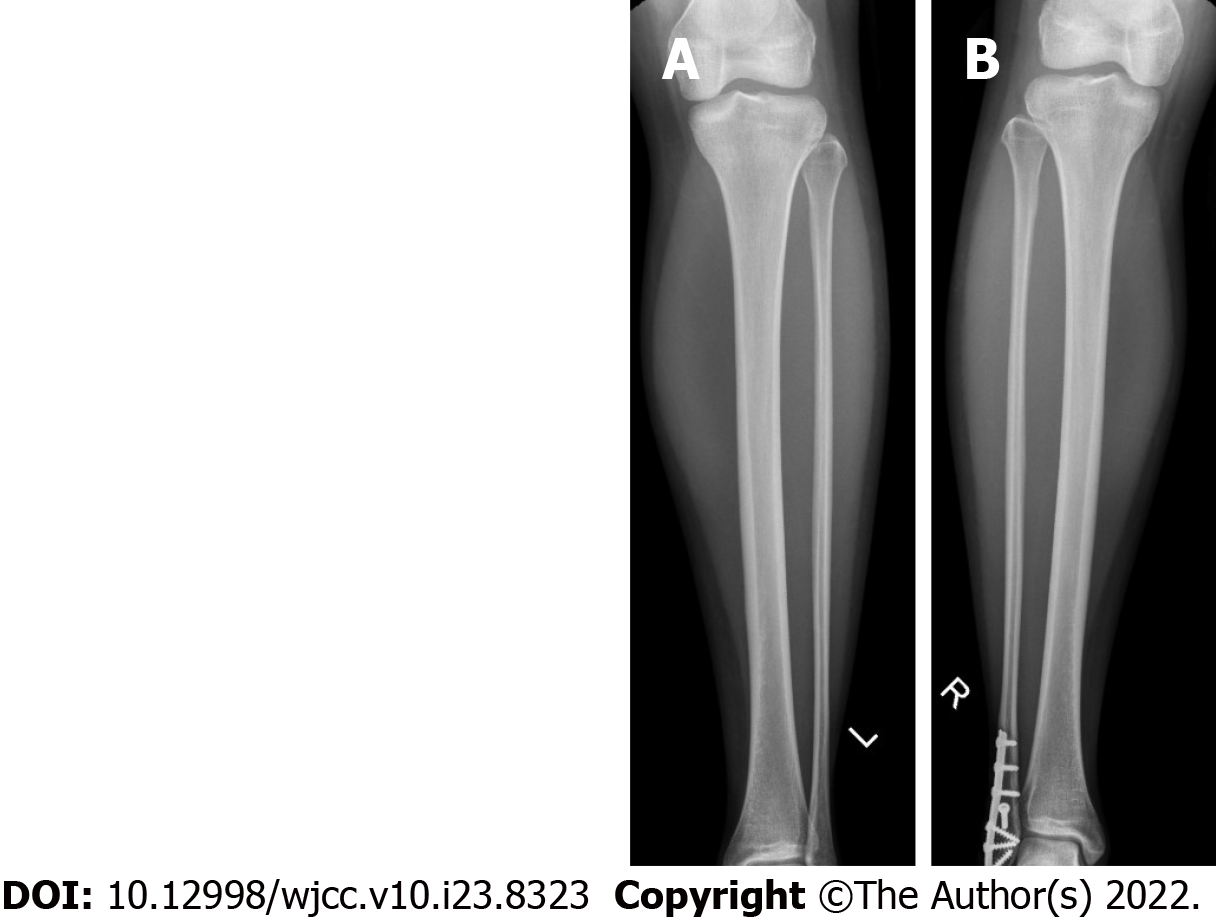
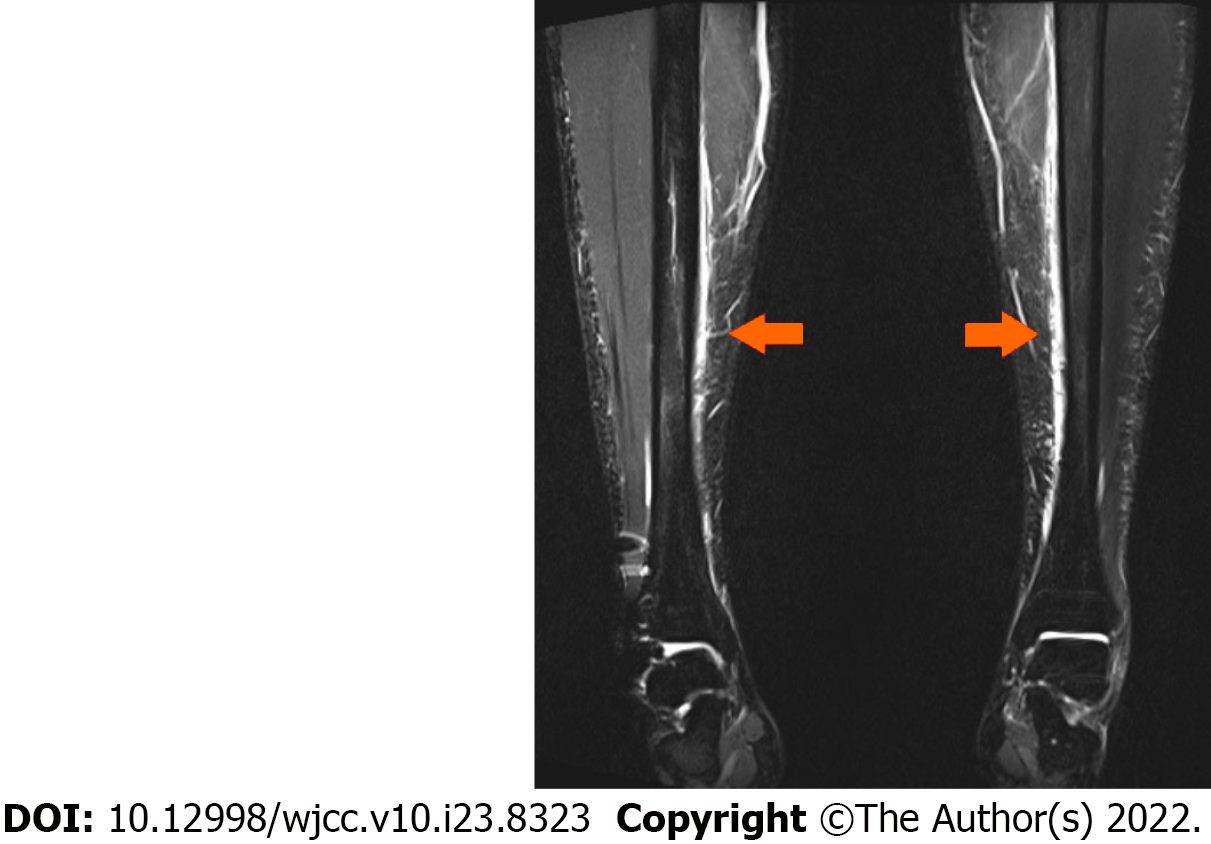
Radiographs did not show any tibial fracture. An old healed right ankle fracture fixation was seen (Figure 1). MRI scans of both tibiae demonstrated periosteal oedema and fluid overlying the antero-medial cortices of the tibial diaphyses, but no fracture, consistent with bilateral medial tibial stress syndrome (Figure 2).
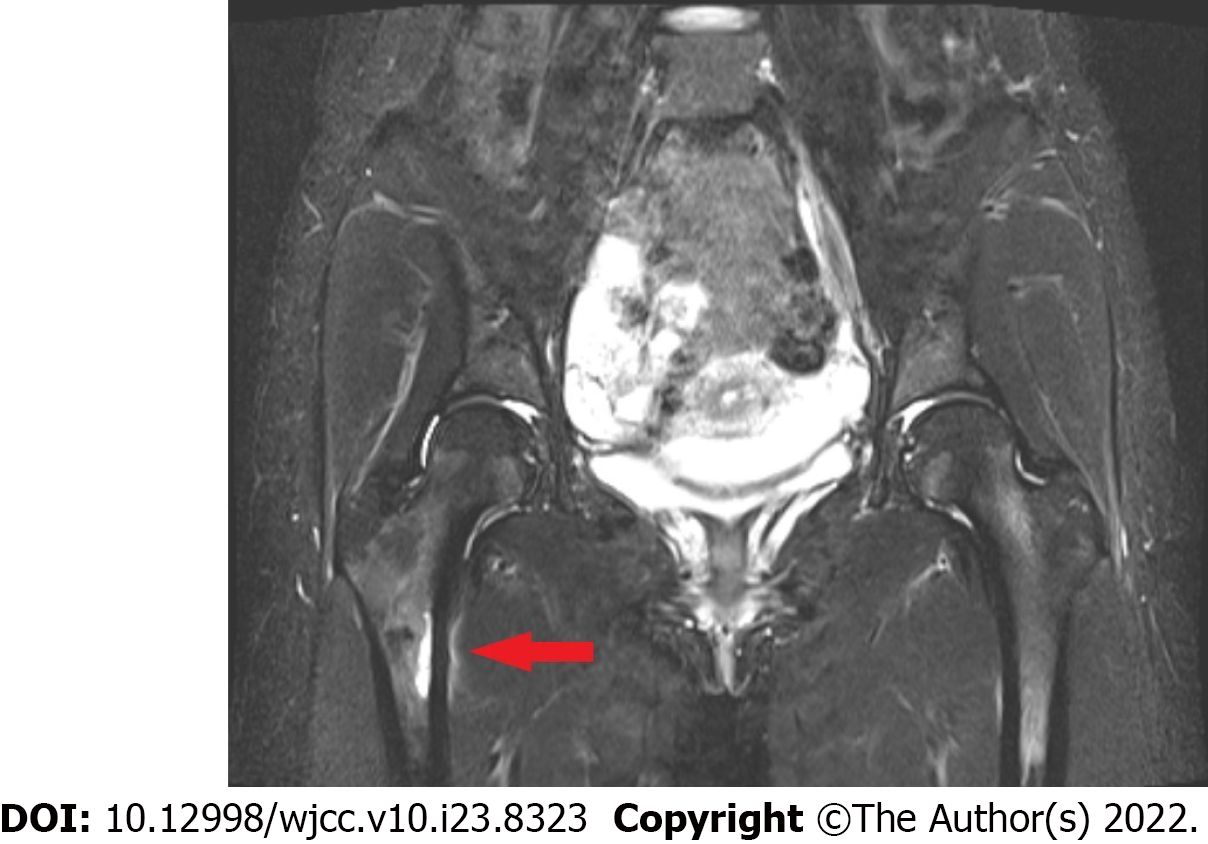
MRI scan of the right hip demonstrated an incomplete, undisplaced stress fracture at the medial subtrochanteric level of the right femur (Figure 3). A dual energy X-ray absorbitometry scan dem
Dr. Mishra N, Chief of Endocrinology, Singapore Medical Group.
Bilateral medial tibial stress syndrome; femoral neck stress fracture.
The patient was managed conservatively with analgesia and physiotherapy, but continued to exercise against medical advice. She presented again six months later with severe right hip pain.
The patient was warned of the risk of hip fracture requiring surgery. Her symptoms resolved with strict rest and physiotherapy.
The main objective of this study was to highlight the risk of stress injury to the tibia and femur in a young population performing HIIT. A sequential combination of these injuries is unusual and has not been reported before following HIIT.
HIIT has become increasingly popular as a method of exercise. HIIT involves alternating periods of relatively intense work and recovery. HIIT exercises may be subdivided into aerobic exercises e.g., running and cycling, and body weight/resistance exercises[1]. Disciplines such as Crossfit, Tabata training, F45, and ‘Bootcamps’ are examples of HIIT[5-8]. HIIT programs can vary greatly, and may combine aerobic and weight/resistance exercises.
The principle of HIIT is that a greater volume of higher intensity exercise is accumulated during a single HIIT exercise session, compared to traditional moderate-intensity continuous exercise (MICE) training[9,10]. It has been postulated that HIIT improves cardiovascular health, metabolic capacity, and aerobic performance, at a similar or superior rate to MICE[11]. HIIT may be beneficial in individuals with chronic disease[12-18], and in adolescents and the elderly[19-22]. The incidence and type adverse events related to HIIT exercise are not well known, with isolated case reports described in the literature[23-25]. However, injury rates may be under-reported and higher than previously realised[2,26].
MTSS, known to the layperson as ‘shin-splints’, is exercise-induced pain over the anterior tibia, and may lead to tibial stress fractures[1]. MTSS has an incidence of approximately 13 to 20% in runners, and up to 35% in military recruits[27]. Predisposing factors include increasing load and volume of high impact exercise, female gender, previous history of MTSS, high BMI[28-32], as well as Vitamin D deficiency[33,34].
MTSS results from accumulated cortical microdamage which exceeds the ability of the bone to repair itself[35]. Periostitis usually occurs at the site of bony injury, which is at the site of attachment of the tendinous attachments of the soleus, flexor digitorum longus, and posterior tibialis muscles.
MTSS is primarily a clinical diagnosis[36]. Imaging may be performed to exclude a more significant tibial injury such as a stress fracture. Whereas radiographs alone may detect a stress fracture, MRI is the gold standard investigation for identifying MTSS and stress fractures. MRI findings include periosteal oedema and bone marrow oedema. Isotope bone scans are less specific and sensitive than MRI. High-resolution computed tomography is an option but has lower sensitivity than MRI or isotope bone scan. Excluding Vitamin D deficiency is also helpful[30,37].
MTSS is typically managed conservatively, with rest and lifestyle/activity modification to reduce load and stress. An ideal duration of rest and activity has not been defined. There is low-quality evidence to suggest that adjunct therapies such as ice massage, ultrasound therapy, and extracorporeal shockwave therapy, and orthotics may be of benefit. Not every patient that experiences MTSS develops a tibial stress fracture. Severe tibial stress fractures may require surgical intervention[38-40].
FNSF are an uncommon but potentially disabling cause of athletes presenting with exercise-related hip and groin pain. FNSFs account for 5% of all stress fractures and 3% of all sports-related stress fractures. The commonest causative sports are marathon and long-distance running. Outcomes are considerably worse for fractures with a delay in diagnosis and displacement. Risk factors for FNSFs include female gender, poor baseline physical fitness, eating disorders, amenorrhea, and decreased bone mineral density. A combination of repetitive mechanical load to the femoral neck, and bone absorption exceeding metabolic repair during remodelling, may result in FNSF. Radiographs are initially used for diagnosis but have low sensitivity. MRI scan has 100% sensitivity and is the gold standard investigation to detect FNSF. An early diagnosis is important to prevent fracture displacement and reduce risk of avascular necrosis. Management consists of surgical and non-surgical treatments, depending upon symptoms, and fracture characteristics such as location and displacement[4,41-45].
In this case report, the patient was a female who had subjected herself to a large volume of high intensity training. MRI scanning, which is the gold standard to detect bony stress injury, was utilised to confirm the diagnosis[46,47]. Vitamin D deficiency and osteoporosis were excluded. Stress injury was detected, and treated with rest and physical therapy. Surgery was not required. A sequential combination of tibial and femoral stress injury following HIIT exercise has not been reported before. More research needs to be performed to determine a safe duration, type and intensity of exercise performed during HIIT to reduce risk of stress injury.
HIIT can lead to stress injury of the tibia and femur in a young population.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Vyshka G, Albania; Xu G, China S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Billat LV. Interval training for performance: a scientific and empirical practice. Special recommendations for middle- and long-distance running. Part I: aerobic interval training. Sports Med. 2001;31:13-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 310] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 2. | Rynecki ND, Siracuse BL, Ippolito JA, Beebe KS. Injuries sustained during high intensity interval training: are modern fitness trends contributing to increased injury rates? J Sports Med Phys Fitness. 2019;59:1206-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 3. | Kiel J, Kaiser K. Stress Reaction and Fractures. 2021 Aug 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2022. [PubMed] |
| 4. | Robertson GA, Wood AM. Femoral Neck Stress Fractures in Sport: A Current Concepts Review. Sports Med Int Open. 2017;1:E58-E68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Claudino JG, Gabbett TJ, Bourgeois F, Souza HS, Miranda RC, Mezêncio B, Soncin R, Cardoso Filho CA, Bottaro M, Hernandez AJ, Amadio AC, Serrão JC. CrossFit Overview: Systematic Review and Meta-analysis. Sports Med Open. 2018;4:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 154] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 6. | Tabata I. Tabata training: one of the most energetically effective high-intensity intermittent training methods. J Physiol Sci. 2019;69:559-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 51] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 7. | Smith AAH, Wananu M, Carlson MD. Spontaneous Coronary Artery Dissection in a Healthy Woman after Initiating a High-Intensity Interval Training Workout Program. Am J Cardiol. 2018;122:1588-1589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Hoffman JR, Kahana A, Chapnik L, Shamiss A, Davidson B. The relationship of physical fitness on pilot candidate selection in the Israel Air Force. Aviat Space Environ Med. 1999;70:131-134. [PubMed] |
| 9. | Gibala MJ, Little JP, Macdonald MJ, Hawley JA. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol. 2012;590:1077-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 900] [Cited by in RCA: 1013] [Article Influence: 77.9] [Reference Citation Analysis (0)] |
| 10. | CHRISTENSEN EH, HEDMAN R, SALTIN B. Intermittent and continuous running. (A further contribution to the physiology of intermittent work.). Acta Physiol Scand. 1960;50:269-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 92] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Helgerud J, Høydal K, Wang E, Karlsen T, Berg P, Bjerkaas M, Simonsen T, Helgesen C, Hjorth N, Bach R, Hoff J. Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc. 2007;39:665-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 701] [Cited by in RCA: 778] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 12. | Beauchamp MK, Nonoyama M, Goldstein RS, Hill K, Dolmage TE, Mathur S, Brooks D. Interval vs continuous training in individuals with chronic obstructive pulmonary disease--a systematic review. Thorax. 2010;65:157-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 107] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Guiraud T, Nigam A, Gremeaux V, Meyer P, Juneau M, Bosquet L. High-intensity interval training in cardiac rehabilitation. Sports Med. 2012;42:587-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 190] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 14. | Kessler HS, Sisson SB, Short KR. The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Med. 2012;42:489-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 264] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 15. | Ross LM, Porter RR, Durstine JL. High-intensity interval training (HIIT) for patients with chronic diseases. J Sport Health Sci. 2016;5:139-144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 16. | Rognmo Ø, Hetland E, Helgerud J, Hoff J, Slørdahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2004;11:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 429] [Cited by in RCA: 467] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 17. | Freyssin C, Verkindt C, Prieur F, Benaich P, Maunier S, Blanc P. Cardiac rehabilitation in chronic heart failure: effect of an 8-week, high-intensity interval training vs continuous training. Arch Phys Med Rehabil. 2012;93:1359-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 111] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 18. | Karstoft K, Winding K, Knudsen SH, Nielsen JS, Thomsen C, Pedersen BK, Solomon TP. The effects of free-living interval-walking training on glycemic control, body composition, and physical fitness in type 2 diabetic patients: a randomized, controlled trial. Diabetes Care. 2013;36:228-236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 217] [Cited by in RCA: 239] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 19. | Terada T, Wilson BJ, Myette-Côté E, Kuzik N, Bell GJ, McCargar LJ, Boulé NG. Targeting specific interstitial glycemic parameters with high-intensity interval exercise and fasted-state exercise in type 2 diabetes. Metabolism. 2016;65:599-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 20. | Cao M, Quan M, Zhuang J. Effect of High-Intensity Interval Training vs Moderate-Intensity Continuous Training on Cardiorespiratory Fitness in Children and Adolescents: A Meta-Analysis. Int J Environ Res Public Health. 2019;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 85] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 21. | Martin-Smith R, Cox A, Buchan DS, Baker JS, Grace F, Sculthorpe N. High Intensity Interval Training (HIIT) Improves Cardiorespiratory Fitness (CRF) in Healthy, Overweight and Obese Adolescents: A Systematic Review and Meta-Analysis of Controlled Studies. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 22. | Marriott CFS, Petrella AFM, Marriott ECS, Boa Sorte Silva NC, Petrella RJ. High-Intensity Interval Training in Older Adults: a Scoping Review. Sports Med Open. 2021;7:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 23. | Jiménez-García JD, Martínez-Amat A, De la Torre-Cruz MJ, Fábrega-Cuadros R, Cruz-Díaz D, Aibar-Almazán A, Achalandabaso-Ochoa A, Hita-Contreras F. Suspension Training HIIT Improves Gait Speed, Strength and Quality of Life in Older Adults. Int J Sports Med. 2019;40:116-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 24. | Vukanic D, Murphy D, Juhdi A, Leonard M. A Big HIIT: A Fracture Dislocation of the Hip in a Young Man Participating in Extreme Conditioning Exercise: A Case Report. JBJS Case Connect. 2020;10:e1900516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Sephien A, Orr J, Remaley DT. Pectoralis major tear in a 23-year-old woman while performing high-intensity interval training: a rare presentation. BMJ Case Rep. 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Jackson, J, Hart S, Fries CA, Robinson J, Murray J, Wood AM. CrossFitter’s knee: patellofemoral chondral injury following high-intensity functional training. J R Nav Med Serv. 103:35-38. [PubMed] |
| 27. | Minghelli B, Vicente P. Musculoskeletal injuries in Portuguese CrossFit practitioners. J Sports Med Phys Fitness. 2019;59:1213-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | Yates B, White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am J Sports Med. 2004;32:772-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 219] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 29. | Reinking MF, Austin TM, Richter RR, Krieger MM. Medial Tibial Stress Syndrome in Active Individuals: A Systematic Review and Meta-analysis of Risk Factors. Sports Health. 2017;9:252-261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 30. | Franklyn M, Oakes B. Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World J Orthop. 2015;6:577-589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (2)] |
| 31. | Moen MH, Tol JL, Weir A, Steunebrink M, De Winter TC. Medial tibial stress syndrome: a critical review. Sports Med. 2009;39:523-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 114] [Article Influence: 7.1] [Reference Citation Analysis (1)] |
| 32. | Hamstra-Wright KL, Bliven KC, Bay C. Risk factors for medial tibial stress syndrome in physically active individuals such as runners and military personnel: a systematic review and meta-analysis. Br J Sports Med. 2015;49:362-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 33. | Barton CJ, Bonanno DR, Carr J, Neal BS, Malliaras P, Franklyn-Miller A, Menz HB. Running retraining to treat lower limb injuries: a mixed-methods study of current evidence synthesised with expert opinion. Br J Sports Med. 2016;50:513-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 117] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 34. | Tenforde AS, Sayres LC, Sainani KL, Fredericson M. Evaluating the relationship of calcium and vitamin D in the prevention of stress fracture injuries in the young athlete: a review of the literature. PM R. 2010;2:945-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Ruohola JP, Laaksi I, Ylikomi T, Haataja R, Mattila VM, Sahi T, Tuohimaa P, Pihlajamäki H. Association between serum 25(OH)D concentrations and bone stress fractures in Finnish young men. J Bone Miner Res. 2006;21:1483-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 152] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 36. | Winters M, Burr DB, van der Hoeven H, Condon KW, Bellemans J, Moen MH. Microcrack-associated bone remodeling is rarely observed in biopsies from athletes with medial tibial stress syndrome. J Bone Miner Metab. 2019;37:496-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Winters M, Bakker EWP, Moen MH, Barten CC, Teeuwen R, Weir A. Medial tibial stress syndrome can be diagnosed reliably using history and physical examination. Br J Sports Med. 2018;52:1267-1272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 38. | Moen MH, Schmikli SL, Weir A, Steeneken V, Stapper G, de Slegte R, Tol JL, Backx FJ. A prospective study on MRI findings and prognostic factors in athletes with MTSS. Scand J Med Sci Sports. 2014;24:204-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 39. | Winters M, Eskes M, Weir A, Moen MH, Backx FJ, Bakker EW. Treatment of medial tibial stress syndrome: a systematic review. Sports Med. 2013;43:1315-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 40. | Lohrer H, Malliaropoulos N, Korakakis V, Padhiar N. Exercise-induced leg pain in athletes: diagnostic, assessment, and management strategies. Phys Sportsmed. 2019;47:47-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 41. | Bonanno DR, Murley GS, Munteanu SE, Landorf KB, Menz HB. Effectiveness of foot orthoses for the prevention of lower limb overuse injuries in naval recruits: a randomised controlled trial. Br J Sports Med. 2018;52:298-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 42. | Matcuk GR Jr, Mahanty SR, Skalski MR, Patel DB, White EA, Gottsegen CJ. Stress fractures: pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol. 2016;23:365-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 129] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 43. | Voss L, DaSilva M, Trafton PG. Bilateral femoral neck stress fractures in an amenorrheic athlete. Am J Orthop (Belle Mead NJ). 1997;26:789-792. [PubMed] |
| 44. | Bennell K, Matheson G, Meeuwisse W, Brukner P. Risk factors for stress fractures. Sports Med. 1999;28:91-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 175] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 45. | Maffulli, N. , Longo, U. and Denaro, V., 2009. Femoral Neck Stress Fractures. Operative Techniques in Sports Medicine. 2009;17:90-93. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 46. | Sofka CM. Imaging of stress fractures. Clin Sports Med. 2006;25:53-62, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 47. | Biz C, Berizzi A, Crimì A, Marcato C, Trovarelli G, Ruggieri P. Management and treatment of femoral neck stress fractures in recreational runners: a report of four cases and review of the literature. Acta Biomed. 2017;88:96-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |