Published online Aug 16, 2022. doi: 10.12998/wjcc.v10.i23.8249
Peer-review started: December 1, 2021
First decision: March 15, 2022
Revised: June 3, 2022
Accepted: June 21, 2022
Article in press: June 21, 2022
Published online: August 16, 2022
Processing time: 242 Days and 19.6 Hours
Epiglottic cysts is a rare but potentially lethal supraglottic airway pathology in infants due to the high risk of cannot intubation or cannot ventilation. Awake fiberoptic intubation appeared to be the safest technique, but it is very challenging in infants with large epiglottic cysts. Even it has the risk of airway loss. We report that cyst aspiration is an effective treatment as the first-choice procedure for airway management in an infant with large epiglottic cysts.
A 46-day-old male infant weighing 2.3 kg presented to the emergency room with difficulty feeding, worsening stridor, and progressive respiratory distress. Epiglottic cysts was diagnosed, but fibro bronchoscopy examination failed, as the fiberoptic bronchoscope was unable to cross the epiglottic cysts to the trachea. The infant was transferred to the operating room for emergency cystectomy under general anesthesia. Spontaneous respiration was maintained during anesthesia induction, and cyst aspiration was performed as the first procedure for airway management under video laryngoscopy considering that the preoperative fibro bronchoscopy examination failed. Then, the endotracheal tube was intubated successfully. Cystectomy was performed uneventfully, and the infant was safely transferred to the intensive care unit after surgery. The infant was extubated smoothly on the third postoperative day and discharged on the eighth day after surgery. On follow-up 1 year after the surgery, a normal airway was found by fibro bronchoscopy examination.
Epiglottic cyst aspiration can be considered the first procedure for airway management in infants with large epiglottic cysts.
Core Tip: Epiglottic cysts is a rare but potentially lethal supraglottic airway pathology in infants. Surgical cystectomy is the mainstay and established treatment method, which poses a significant anesthetic challenge for airway management due to the increased risk of difficult tracheal intubation and airway occlusion resulting in hypoventilation, hypoxemia, and even death. In this report, cysts aspiration was selected as the first treatment for airway management in an infant with large epiglottic cysts, and an endotracheal tube was successfully intubated after cysts aspiration. This anesthesia technique is considered as the first choice for airway management in infants with large epiglottic cysts.
- Citation: Zheng JQ, Du L, Zhang WY. Aspiration as the first-choice procedure for airway management in an infant with large epiglottic cysts: A case report. World J Clin Cases 2022; 10(23): 8249-8254
- URL: https://www.wjgnet.com/2307-8960/full/v10/i23/8249.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i23.8249
Epiglottic cysts is a rare but potentially lethal supraglottic airway pathology in infants and are caused by ductal obstruction of either mucous glands or minor salivary glands in the vallecula and base of the tongue[1]. Epiglottic cysts can cause stridor, wheezing, respiratory distress, swallowing difficulty, failure to thrive, and even life-threatening conditions according to the extent of airway obstruction by its location and size[2]. Acute life-threatening airway compromise always requires emergency airway management[3]. However, patients with catastrophic cases are still reported during airway mana
Surgery is the mainstay and established treatment method for epiglottic cysts[6]. Surgical cystectomy for epiglottic cysts poses a significant anesthetic challenge for airway management, as these patients are at increased risk of difficult tracheal intubation and airway occlusion resulting in hypoventilation, hypoxemia, and even death[4,5,7]. Particularly in infants with large epiglottic cysts, the success rate of tracheal intubation by different equipment remains low[8,9]. Tracheal intubation may not be able to be completed by straight blade laryngoscopy, video laryngoscopy, and even fiberoptic intubation, as the passage for endotracheal intubation could be blocked by the cysts[8-11]. Therefore, a meticulous airway assessment and an anesthetic plan are mandatory before surgery and anesthesia induction.
Considering the risk of pulmonary aspiration, epiglottic cysts aspiration is only used in an emergency, such as cannot intubation or cannot ventilation[8,9]. Whether epiglottic cysts aspiration could be used as the first-choice procedure for airway management in infants with large epiglottic cysts remains unclear as the speculated risk of pulmonary inspiration[4,8,9]. In our case report, cysts aspiration was selected as the first treatment for airway management in an infant with large epiglottic cysts, and an endotracheal tube was successfully intubated after cysts aspiration. Herein, we recommend cysts aspiration as the first choice for airway management in infants with large epiglottic cysts.
A 46-d-old male infant weighing 2.3 kg presented to the emergency room with difficulty feeding, worsening stridor, and progressive respiratory distress.
The infant developed difficulty feeding, worsening stridor, and progressive respiratory distress for 1 wk.
The infant had no past history.
The infant had no personal or family history.
The physical examination of the infant showed stridor and progressive respiratory distress.
Preoperative blood biochemistry was normal. Saturation of pulse oximetry ranged from 85% to 90% on 60% oxygen by nasal catheters.
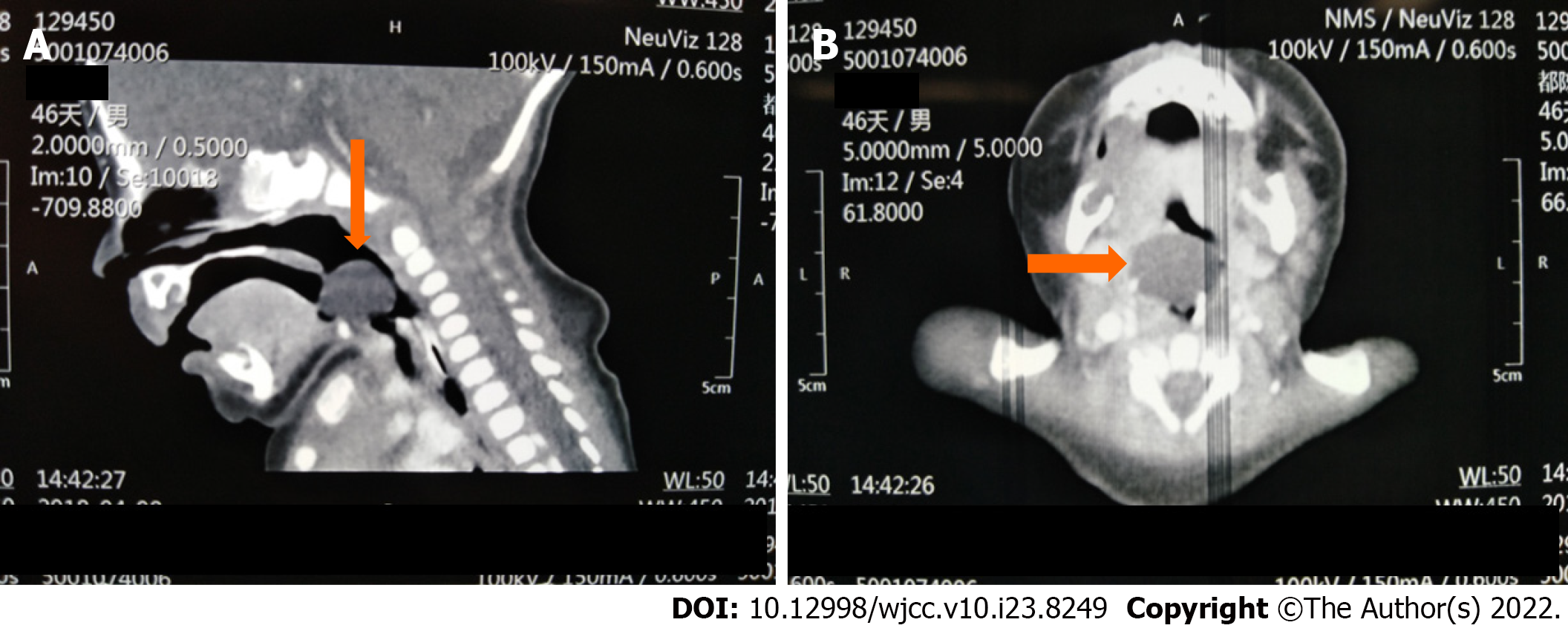
Preoperative electrocardiogram, transthoracic echocardiography, and chest X-ray were normal. Computed tomography (CT) showed a giant round mass on the lingual surface of the epiglottis (Figure 1). Fibro bronchoscopy examination failed, but video laryngoscopy confirmed the giant cyst to be implanted on the tip of the epiglottis (Figure 2).
The infant was diagnosed with epiglottic cysts.
The infant was transferred to the operating room for emergency cystectomy under general anesthesia. The anesthesia induction plan was inhalational induction maintaining spontaneous breathing and keeping an otolaryngologist on standby for emergency tracheostomy if necessary. The infant was placed in the sniffing position on the operation table preoxygenated with 100% oxygen and premedicated with intravenous atropine 0.02 mg/kg. Inhalational induction was performed by upward titration of sevoflurane from 1% to 6% with 100% oxygen. Spontaneous breathing was maintained, and the effectiveness of mask ventilation was confirmed during the induction process. When the skeletal muscle relaxation was adequate, a video laryngoscope blade was inserted from the right side of the mouth. Large epiglottic cysts was visualized in the midline of the laryngeal inlet, and the epiglottis was not revealed (Figure 2). Considering that fiberoptic bronchoscopy failed to cross the epiglottic cysts during fibro bronchoscopy examination, fiberoptic intubation was not attempted. Any repeated attempts to reveal the epiglottis by pushing cysts to the left could rupture the cysts by accident, which could increase the risk of pulmonary aspiration. Therefore, cysts aspiration was performed as the first procedure for airway management after careful consideration. Aspiration was used by an 18-gauge needle with an attached 20 mL syringe (Figure 2). Six milliliters of transparent fluid were aspirated from the cysts, and then the epiglottis and arytenoid cartilage appeared. A 3.0 mm inner diameter cuffed endotracheal tube was intubated successfully under the infant's spontaneous breathing (Figure 3). Thereafter, fentanyl and atracurium were administered intravenously and general anesthesia was maintained with sevoflurane. Carbon dioxide laser cystectomy was performed under the suspended laryngoscope. The infant was safely transferred to the intensive care unit for gradual weaning considering the development of edema at the surgical site after surgery.
Tracheomalacia was suspected on the postoperative first day as the positive cuff leak test. So, the infant was extubated smoothly until the postoperative third day after repeated postoperative fiberoptic bronchoscopy to ruled out tracheomalacia. Diagnostic fibro bronchoscopy examination revealed a normal airway on the fifth day and the infant was discharged on the eighth day after surgery. On follow-up 1 year after the surgery, a normal airway was found by fibro bronchoscopy examination.
Epiglottic cysts pose a great challenge to airway management, especially in neonates and young infants with a relatively small airway. Detailed preoperative assessment, including obstructive symptoms assessment, CT scan, and fiberoptic bronchoscope examination, must be determined to make a meticulous airway assessment and anesthetic plan[12].
Due to the high risk of difficult endotracheal intubation and difficult mask ventilation, spontaneous breathing should be maintained to avoid the disastrous consequences caused by cannot intubation or cannot ventilation[8,9]. Otolaryngologists must standby for emergency tracheostomy if required during anesthesia induction. Muscle relaxants (preferred succinylcholine) can be used to improve intubation conditions only when the effectiveness of face-mask ventilation is confirmed. Successful tracheal intubation by direct laryngoscopy, video laryngoscope, awake fiberoptic bronchoscope or tongue tip traction suture technique or “three-person technique” of fiberoptic intubation in patients with large epiglottic cysts was reported[7-11,13-17]. However, the success rate is low, and several attempts are often needed, which could increase the risk of airway trauma[8,9].
Awake fiberoptic intubation appeared to be the safest technique, particularly in adult patients with upper airway obstruction. However, in infants, several hurdles could be encountered during awake fiberoptic intubation. First, there was a lack of cooperation in this age group. Second, the hypopharynx is occupied by the large cyst, and the space available for manipulation of the scope in the hypopharynx is limited even in expert hands. Third, anatomical structures such as the larynx and arytenoid cartilage were severely distorted, and the glottis was pushed to an unusually acute angle to the arytenoid cartilage, which created an awkward passage for advancement of the endotracheal tube under the guidance of the bronchoscope. In addition, the resistance of upper airway soft tissue can make it difficult to intubate using fiberoptic intubation. In this situation, the tracheal tube could rupture the cysts by accident during intubation. Last, adequate topicalization could be difficult to acquire due to the limitations in the volume of local anesthetic. As a result, awake fiberoptic intubation still has the potential for loss of airway patency. In infants with large epiglottic cysts, it can be very distressing and may even fail in well-trained anesthesiologists[9,11,13,18,19].
Cyst aspiration by a large-bore needle to improve the intubation conditions can be beneficial. It is only used in an emergency as the previous clinical case reported, considering the risk of pulmonary aspiration[8,9]. Even in a clinical case, emergency tracheostomy was performed as the first treatment for cannot intubation and cannot ventilation, rather than epiglottic cysts aspiration[4]. Obviously, the complications of tracheostomy are significantly higher than epiglottic cyst aspiration[20]. In addition, aspiration is a safe surgical approach for the epiglottic cyst[6]. Reviewing the literature on anesthesia management of epiglottic cysts, we found that epiglottic cysts aspiration is a safe and effective procedure for airway management. However, it was only used as the rescue technique, when the routine intubation techniques failed. It can reduce the cyst size and can avoid a tracheostomy[21-25]. Based on the safety and feasibility of this procedure, if this method is preferred as the first procedure for airway management, it will be more beneficial to these patients.
Pulmonary aspiration is the most concerning complication for the clinical application of epiglottic cyst aspiration. Adequate aspiration and quick endotracheal intubation are the key factors of this technique, as to avoid pulmonary aspiration. However, aspiration treatment is a safe and established surgical approach for epiglottic cyst in the clinic. In our case, adequate aspiration by a large-bore needle (18-gauge needle) with an attached syringe (20 mL) can safely expose arytenoids and epiglottis, facilitating endotracheal intubation. In addition, it is a safe and effective procedure for airway management based on a literature review. Simultaneously, adequate aspiration could prevent pulmonary aspiration caused by accidental cysts rupture during repeated attempts of endotracheal intubation. It should be noted that when the patient's coagulation function was abnormal, epiglottic cysts aspiration was considered contraindicated. Hence, we propose that cysts aspiration could be considered as the first choice for airway management in infants with large epiglottic cysts.
Epiglottic cysts aspiration by a large-bore needle can facilitate endotracheal intubation in infants with giant epiglottic cysts. It could be considered the first procedure for airway management in infants with large epiglottic cysts. It is also an effective and safe procedure to protect the airway away from pulmonary aspiration caused by accidental cysts rupture.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Amornyotin S, Thailand; Arslan M, Turkey; Arumugam EAP, India; Moschovi MA, Greece S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Mulcahy CF, Reddy SK, Wikner EE, Mudd PA. Neonatal airway anomaly: vallecular cyst. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Oelsen JM, Hewett KM, Discolo CM, Jackson BF. Congenital Vallecular Cyst as a Cause of Neonatal Stridor and Apnea. Pediatr Emerg Care. 2018;34:e152-e154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Sugiyama T, Kamijo A, Aoyama K, Kuroda Y, Masuyama K, Sugita K. Rapid development of severe respiratory distress due to a vallecular cyst in a 3-day-old infant. Pediatr Int. 2012;54:297-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Batra UB, Kale S, Malik A. Anaesthetic management of an infant with vallecular cyst: A challenging situation. Indian J Anaesth. 2012;56:423-425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Breysem L, Goosens V, Vander Poorten V, Vanhole C, Proesmans M, Smet M. Vallecular cyst as a cause of congenital stridor: report of five patients. Pediatr Radiol. 2009;39:828-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Li Y, Irace AL, Dombrowski ND, Perez-Atayde AR, Robson CD, Rahbar R. Vallecular cyst in the pediatric population: Evaluation and management. Int J Pediatr Otorhinolaryngol. 2018;113:198-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Leibowitz JM, Smith LP, Cohen MA, Dunham BP, Guttenberg M, Elden LM. Diagnosis and treatment of pediatric vallecular cysts and pseudocysts. Int J Pediatr Otorhinolaryngol 2011; 75:899-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Vorobeichik L, Hare GM, Zirkle M, Garavaglia MM. Airway Management of Incidental Vallecular Cysts in Adults. A A Case Rep. 2015;5:223-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Cheng KS, Ng JM, Li HY, Hartigan PM. Vallecular cyst and laryngomalacia in infants: report of six cases and airway management. Anesth Analg. 2002;95:1248-1250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Sugita T, Arisaka H. AirWay Scope™ for Difficult Ventilation in a Patient With Epiglottic Cyst. Anesth Prog. 2018;65:204-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Gupta A, Gupta N. Failed videolaryngoscopy in an infant with giant vallecular cyst managed successfully with a 'three-person technique' of fibre-optic intubation. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Suzuki J, Hashimoto S, Watanabe K, Takahashi K. Congenital vallecular cyst in an infant: case report and review of 52 recent cases. J Laryngol Otol. 2011;125:1199-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Wong CM, Ghazal EA, Dyleski RA, Applegate RL 2nd. Management of Near-Complete Airway Obstruction Caused by a Vallecular Cyst in an Infant Using a Tongue Tip Traction Suture. A A Case Rep. 2016;6:31-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Lin N, Li M, Shi S, Li TZ, Zhang BX. Shikani™ Seeing Optical Stylet-aided tracheal intubation in patients with a large epiglottic cyst. Chin Med J (Engl). 2011;124:2795-2798. [PubMed] |
| 15. | Choi GS, Park SI, Lee EH, Yoon SH. Awake Glidescope® intubation in a patient with a huge and fixed supraglottic mass -A case report-. Korean J Anesthesiol. 2010;59 Suppl:S26-S29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Kothandan H, Ho VK, Chan YM, Wong T. Difficult intubation in a patient with vallecular cyst. Singapore Med J. 2013;54:e62-e65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Ajimi J, Nishikawa K, Niwa Y, Suzuki T. Successful tracheal intubation in a patient with a large epiglottic cyst using the MedAn video laryngoscope with Nishikawa blade. J Clin Anesth. 2021;71:110232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 18. | Kalra S, Saraswat N, Kaur R, Agarwal R. Vallecular cyst in a newborn: a challenging airway. Anaesth Intensive Care. 2011;39:509-510. [PubMed] |
| 19. | Ku AS. Vallecular cyst: report of four cases--one with co-existing laryngomalacia. J Laryngol Otol. 2000;114:224-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Pereira KD, MacGregor AR, Mitchell RB. Complications of neonatal tracheostomy: a 5-year review. Otolaryngol Head Neck Surg. 2004;131:810-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Choi YW, Chon JY, Moon HS, Kim JY, Lee JY. Anesthetic management of a neonate with congenital laryngeal cyst. Korean J Anesthesiol. 2012;63:282-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Reiersen DA, Gungor AA. Airway management in an infant with a giant vallecular cyst. Am J Otolaryngol. 2014;35:261-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 23. | Ouchi K, Onizawa Y, Kido T, Iwabuchi A, Sumazaki R. Congenital epiglottic cyst: Neck position-dependent respiratory distress in newborns. Pediatr Int. 2017;59:939-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | AlAbdulla AF. Congenital Vallecular Cyst Causing Airway Compromise in a 2-Month-Old Girl. Case Rep Med. 2015;2015:975859. [PubMed] |
| 25. | Kislal FM, Acar B, Inan Y, Degerli S, Günbey E. Giant congenital epiglottic cyst presenting with airway obstruction at birth. J Craniofac Surg. 2012;23:602-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |