Published online Jul 26, 2022. doi: 10.12998/wjcc.v10.i21.7539
Peer-review started: February 4, 2022
First decision: March 23, 2022
Revised: April 5, 2022
Accepted: May 28, 2022
Article in press: May 28, 2022
Published online: July 26, 2022
Processing time: 157 Days and 1.3 Hours
One of the causes of foot drop is compression of the common peroneal nerve caused by space-occupying lesions such as a synovial cyst or a ganglion cyst. Most previous reports have involved compressive common peroneal neuropathy by intraneural ganglion cysts and synovial cysts. Compression of the peroneal nerve by extraneural ganglion cysts is rare. We report a rare case of compressive common peroneal neuropathy by an extraneural ganglion cyst.
A 46-year-old man was hospitalized after he reported a right foot drop for 1 mo. Manual muscle testing revealed scores of 1/5 on dorsiflexion of the right ankle. Hypoesthesia and paresthesia on the right lateral leg and foot dorsum were noted. He was diagnosed with a popliteal cyst by using electrophysiologic study and popliteal ultrasound (US). To facilitate common peroneal nerve (CPN) decom
Precise diagnosis and immediate treatment are important in cases of compressive common peroneal neuropathy caused by an extraneural cyst.
Core Tip: Nerve compression by a ganglion cyst is less common compared to other complications. Compression of the tibial nerve by a Baker’s cyst has been frequently reported. Cases of compression of the common peroneal nerve alone by an intraneural ganglion cyst have been reported sometimes. In our case, the peroneal nerve was compressed by an extraneural ganglion cyst, making it a very rare occurrence.
- Citation: Won KH, Kang EY. Differential diagnosis and treatment of foot drop caused by an extraneural ganglion cyst above the knee: A case report. World J Clin Cases 2022; 10(21): 7539-7544
- URL: https://www.wjgnet.com/2307-8960/full/v10/i21/7539.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i21.7539
Foot drop is a clinical condition wherein the foot drags on the ground during the swing phase due to weakness of dorsiflexors of the ankle and foot. Common peroneal neuropathy is the most common cause of foot drop. It is caused by space-occupying lesions such as a synovial cyst or a ganglion cyst around the fibular neck.
There are many case about compressive common peroneal neuropathy by an intraneural ganglion cyst or a synovial cyst. Other causes include anterior horn cell disease, lumbar plexopathies, L5 radiculopathy, and partial sciatic neuropathy. Therefore, those lesions should be differentiated by careful history taking, physical examination, electrodiagnosis, and imaging studies.
We report a rare case of an extraneural ganglion cyst compressing the common peroneal nerve (CPN).
A 46-year-old Asian man (162 cm and 50 kg) complained of a right foot drop.
The patient was hospitalized after he reported a right foot drop for 1 mo. He visited another hospital before visiting our practice and was recommended to undergo rehabilitation treatment for foot drop due to suspected nerve damage; however, no radiological examination was performed.
Medical history taking revealed that the patient had been diagnosed with fibromyalgia and Addison's disease and had been consuming prednisolone, acetaminophen, and tramadol for over 8 years.
There was no specific personal and family history.
Manual muscle testing revealed scores of 1/5 on dorsiflexion of the right ankle and toes, 4/5 on plantar flexion of the right ankle, and 5/5 on others. Hypoesthesia and paresthesia on the right lateral leg and foot dorsum were noted.
There were no abnormal findings in laboratory examinations.
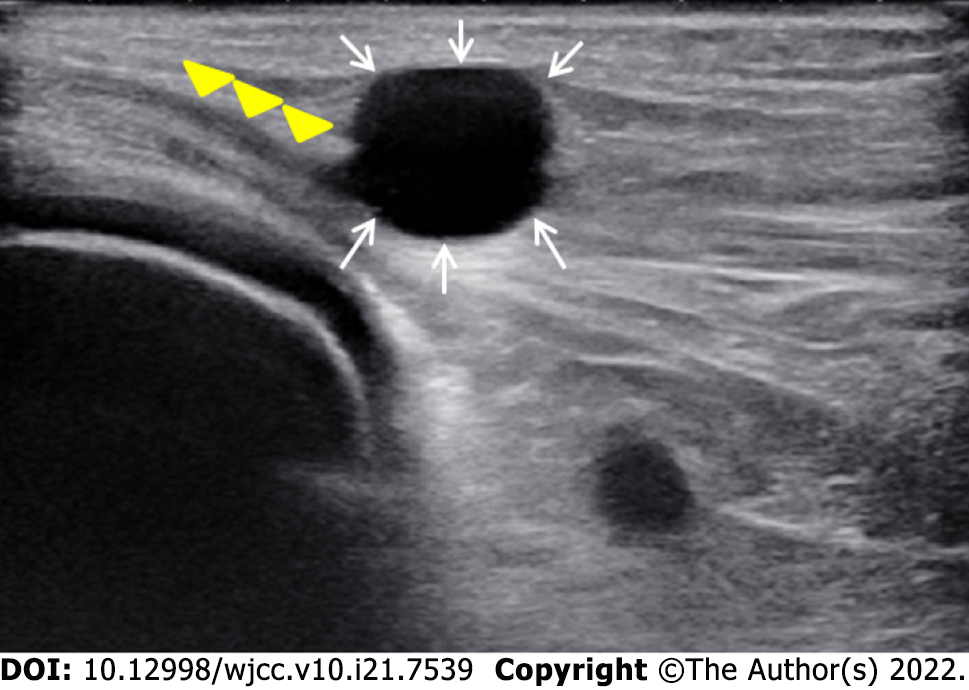
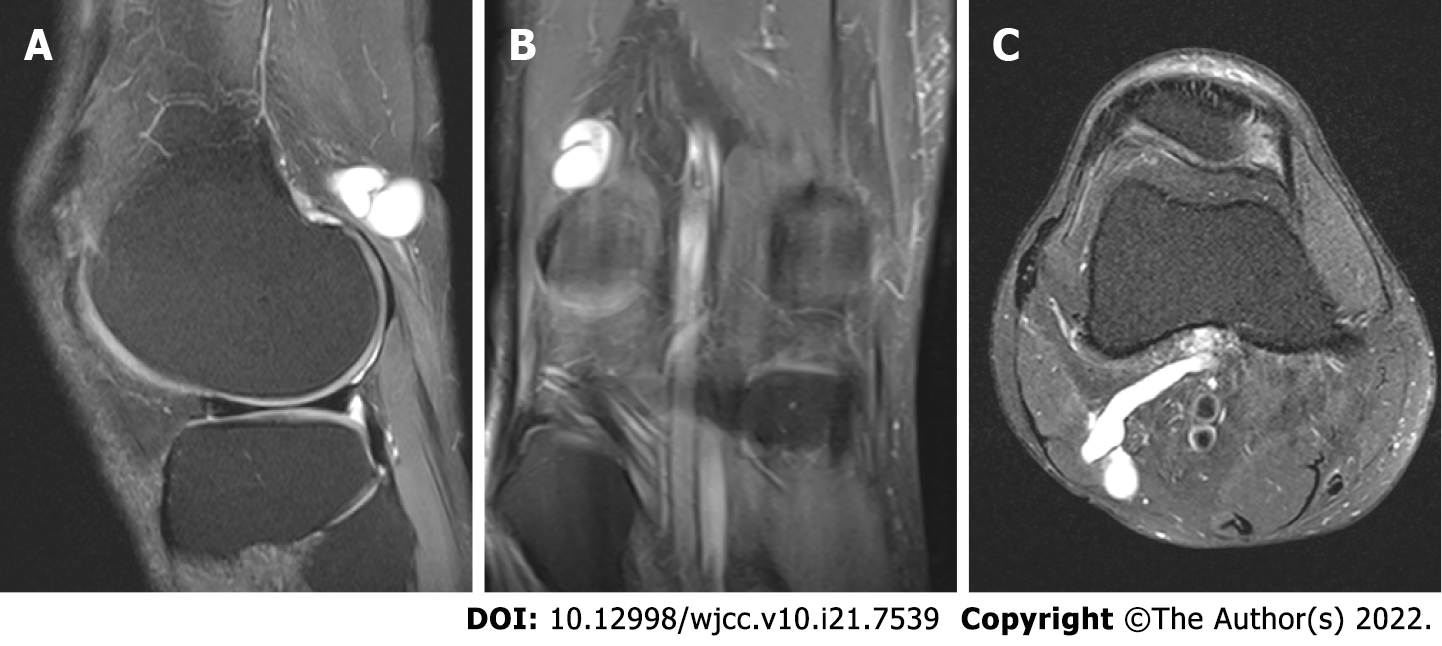
Knee ultrasonography and magnetic resonance imaging (MRI) were performed (Figures 1 and 2).
Common peroneal neuropahty caused by an extranueral ganglion cyst.
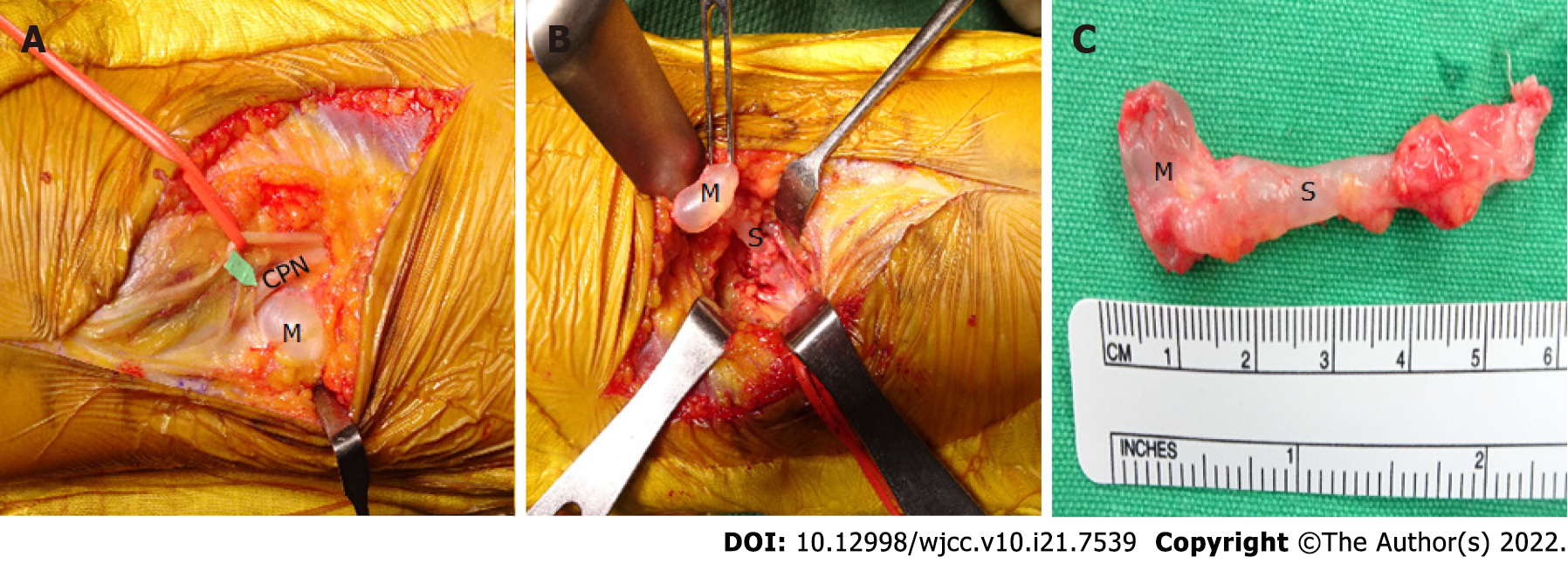
Cyst aspiration under ultrasound (US) guidance and resection of the cyst were performed (Figures 3 and 4).
Four weeks after the operation, the strength of the muscles innervated by the CPN improved to grade 4/5, and the patient could walk safely without posterior leaf spring ankle-foot orthosis (PLS AFO) with only mild residual numbness. In the follow-up physical examination after 1 year, his muscle power was preserved, and he showed a normal gait pattern. Follow-up electrodiagnosis (EDX) 1 year after surgery revealed that the compound muscle action potential of the right deep peroneal nerve amplitude was within the normal limit. Positive sharp waves and fibrillations were observed only in the right tibialis anterior.
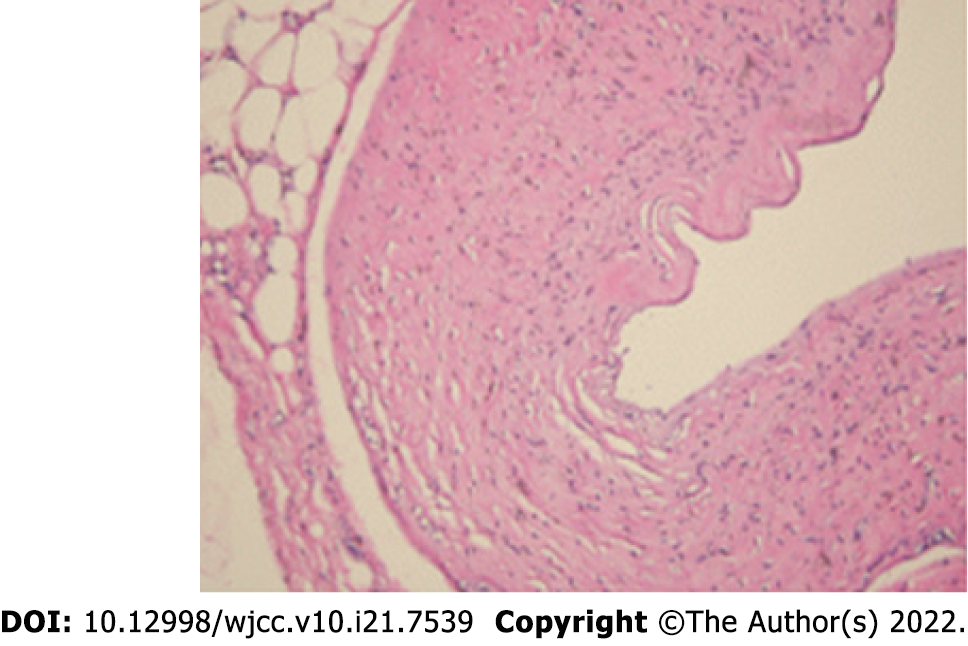
The CPN is the most commonly injured nerve in the lower part of the body[1]; it is susceptible to compression or injury due to its superficial location in the subcutaneous space, directly over the unyielding fibula, tethered by tight fascial bands. It also has a relatively high nerve fascicle to connective tissue ratio, making it vulnerable to injury[2-4]. The CPN can be injured at any location along the thigh to the fibular head region by various types of trauma, including bullet wounds, lacerations, and femur fractures, or by compression secondary to habitual leg crossing, precipitous weight loss, or maintaining the squatting position for extended periods of time. Secondary causes also include space-occupying lesions such as ganglia, cysts, and vascular abnormalities. Malghem et al[5] classified cysts around the knee as ganglion, synovial, and meniscal cysts. Meniscal cysts are formed by accumulation of the synovial fluid in the meniscocapsular junction leaking through the tear or degeneration of the meniscus. Synovial cysts are defined as common cystic masses and are sometimes referred to as a Baker's cyst or popliteal cyst. These cysts are caused by the bulging of the gastrocnemiosemimembranosus bursa towards the posteromedial joint capsule. These cysts can be observed as regions of high signal on T2-weighted images and low signal on T1-weighted MRI images. Diagnosis is confirmed by observation of synovial lining on pathological examination. Zeng et al[6] reported cases of patients with weakness of the peroneal nerve innervation muscles; using MRI, they confirmed that Baker’s cysts compressed the peroneal nerve on the knee and performed surgical resection for cyst removal. Ganglionic cysts are soft-tissue masses caused by the myxoid degeneration of the connective tissue at the joint capsules and tendon sheaths[7]. These show up as hyperintense regions on T2-weighted MRI images. In pathologic findings, the walls are composed of bland fibrous tissue without a specialized lining. It is often difficult to distinguish between ganglion and synovial cysts due to similarities in the site of origin. The principal difference between synovial and ganglion cysts comes from their different content and histologic features. A synovial cyst has, by definition, a synovial cell lining, while a ganglion cyst is delineated by dense fibrous connective tissue[8]. Because of the low prevalence of peroneal nerve palsy caused by ganglion cysts, this condition is generally not easily diagnosed. Ganglion cysts causing compression of the CPN can be classified as either intraneural or extraneural lesions. Most previous reports have involved compressive common peroneal neuropathy by intraneural ganglion cysts related to trauma. Intraneural ganglion cysts are fluid-filled formations within the epineural sheath of peripheral nerves that can cause nerve compression[5,7,9]. According to the articular theory[10], the intranerual ganglion is formed by one-way communication between the proximal tibioficular joint and the articular branch of the CPN. Nerve compression by extraneural ganglion cysts is rare. In this case, a patient with no history of trauma complained of foot drop for 1 mo. During admission to a previous hospital, the medical impression was foot drop due to right sciatic or peroneal nerve lesion, and he was recommended to undergo conservative treatment including rehabilitation to improve foot drop and sensory symptoms without radiologic examination to determine the cause. Upon presentation to our hospital, we conducted an EDX and diagnosed the patient with right incomplete common peroneal neuropathy. US was performed to examine the status of the CPN and surrounding structure, which demonstrated hypoechoic and edematous CPN, compressed by a cystic lesion. The patient’s motor and sensory symptoms were improved after aspiration and rehabilitation. We later performed MRI after the cyst had regrown. MRI demonstrated compression of the CPN by a cystic mass with a narrow and long stalk, which stretched out posterolaterally from the middle popliteal fossa. US and MRI are useful diagnostic methods to evaluate the characteristics of space-occupying lesions such as cysts or tumors. MRI appears to be a superior choice for diagnosing a ganglion cyst. MRI was reported to be a non-invasive approach that shows the precise location of the lesion, the muscle innervated by the peroneal nerve, multiplanar images, and soft-tissue contrast[9]. It was also reportedly helpful in planning surgical resection by allowing the comparison of T1-weighted images and high signals on T2-weighte images[9]. Treatment of ganglion cysts involves cyst aspiration under US guidance and surgical removal[11]. In this case, rehabilitation treatment was performed following decompression of the CPN by aspiration of the cyst. The patient was prescribed ankle dorsiflexor strengthening exercises using elastic band, electrical stimulation for foot drop, and PLS AFO to assist weak dorsiflexors while walking. After rehabilitation for 2 mo, the ankle dorsiflexor recovered to grade 4 in the manual muscle test performed during a follow-up visit. In spite of improvement of symptoms, the cyst was surgically removed after it showed signs of recurrence at follow-up. The ankle dorsiflexor was sustained well at grade 4 in the manual muscle test of the patient who was followed after 1 year. Aspiration of the cyst was effective to allow immediate decompression of the CPN, but the effect was temporary and did not prevent reoccurrence of the cyst. Therefore, surgical excision of the cyst following exact diagnosis is recommended.
Compressive common peroneal neuropathy by an extraneural cyst is rare and is therefore commonly not diagnosed or misdiagnosed. A ganglion cyst should be considered as a differential diagnosis of CPN lesions, and electrophysiologic examination, US, and MRI are useful diagnostic method to evaluate the various possible causes. Early decompression by aspiration and revision surgery has been reported to allow a better prognosis for patients with foot drop due to compression of the CPN caused by a space-occupying lesion such as a mass, ganglion cyst, or synovial cyst. Therefore, precise diagnosis and immediate treatment are important in cases of compressive common peroneal neuropathy caused by an extraneural cyst.
Provenance and peer review: Invited Conference articles; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Rehabilitation
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lu H, China; Nath R, United States; Wei C, China A-Editor: Lin FY, China S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Kara A, Yalçın S, Çelik H, Kuyucu E, Şeker A. Compression neuropathy of the common peroneal nerve caused by an intraosseous ganglion cyst of fibula. Int J Surg Case Rep. 2017;40:10-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Sanchez JE, Conkling N, Labropoulos N. Compression syndromes of the popliteal neurovascular bundle due to Baker cyst. J Vasc Surg. 2011;54:1821-1829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Jung DH, Shin YB, Lee BJ. Early diagnosis with electrodiagnostic study and successful treatment of foot drop caused by intraneural ganglion cyst. J Electrodiagn Neuromuscul Dis. 2020;22:23-26. [DOI] [Full Text] |
| 4. | Souter J, Swong K, McCoyd M, Balasubramanian N, Nielsen M, Prabhu VC. Surgical Results of Common Peroneal Nerve Neuroplasty at Lateral Fibular Neck. World Neurosurg. 2018;112:e465-e472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Malghem J, Vande berg BC, Lebon C, Lecouvet FE, Maldague BE. Ganglion cysts of the knee: articular communication revealed by delayed radiography and CT after arthrography. AJR Am J Roentgenol. 1998;170:1579-1583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 74] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Zeng X, Xie L, Qiu Z, Sun K. Compression neuropathy of common peroneal nerve caused by a popliteal cyst: A case report. Medicine (Baltimore). 2018;97:e9922. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Han HH, Kim JM, Moon SH. A Cystic Mass in the Popliteal Fossa and Its Differential Diagnosis. Arch Plast Surg. 2015;42:484-486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Giard MC, Pineda C. Ganglion cyst versus synovial cyst? Rheumatol Int. 2015;35:597-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Greer-Bayramoglu RJ, Nimigan AS, Gan BS. Compression neuropathy of the peroneal nerve secondary to a ganglion cyst. Can J Plast Surg. 2008;16:181-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Spinner RJ, Atkinson JL, Tiel RL. Peroneal intraneural ganglia: the importance of the articular branch. A unifying theory. J Neurosurg. 2003;99:330-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 193] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 11. | Ji JH, Shafi M, Kim WY, Park SH, Cheon JO. Compressive neuropathy of the tibial nerve and peroneal nerve by a Baker's cyst: case report. Knee. 2007;14:249-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |