Published online Jul 26, 2022. doi: 10.12998/wjcc.v10.i21.7531
Peer-review started: January 10, 2022
First decision: April 8, 2022
Revised: May 17, 2022
Accepted: June 17, 2022
Article in press: June 17, 2022
Published online: July 26, 2022
Processing time: 182 Days and 2.5 Hours
A patient with type III Kummell's disease had a ruptured posterior cortex of the fractured vertebral body, which caused spinal cord compression. An open surgery was considered the best choice of operation. However, the patient and her family refused open surgery and instead demanded a minimally invasive surgical treatment such as percutaneous vertebroplasty (PVP). After preoperative discussion, we finally adopted the novel therapy of traditional Chinese medicine manipulative reduction (TCMMR) combined with PVP.
A patient with type III Kummell's disease exhibiting bone block-induced spinal cord compression was admitted to our hospital. She suffered from a variety of medical disorders but refused open surgery, and instead asked for PVP surgery. TCMMR, in parallel with PVP, was used to restore the height of the compressed vertebral body and reduce the symptoms of spinal cord compression by the bone block in order to strengthen the vertebral body and prevent further collapse. The surgery was very successful. The height of the compressed vertebra was restored, and the symptom of spinal cord compression by bone block was reduced successfully via TCMMR. The fractured vertebra was solidified by the PVP. The pain visual analog score declined from preoperative 7 scores to postoperative 2 scores, and the Frankel spinal cord scale increased from preoperative D degree to postoperative E degree.
The new method has advantages in treating patients with type III Kummell's disease who cannot be treated with open surgery.
Core Tip: We introduced a novel method to treat type III Kummell's disease with spinal cord compression by bone block using traditional Chinese medicine manipulative reduction (TCMMR) combined with percutaneous vertebroplasty (PVP). The combination method could integrate the advantages of the two methods while avoiding open surgery. TCMMR combined with PVP for the treatment of type III Kummell's disease with spinal cord compression by bone block has the advantages of being a simple operation with high safety, and good curative effect.
- Citation: Hao SS, Zhang RJ, Dong SL, Li HK, Liu S, Li RF, Ren HH, Zhang LY. Traditional Chinese medicine manipulative reduction combined with percutaneous vertebroplasty for treating type III Kummell's disease: A case report. World J Clin Cases 2022; 10(21): 7531-7538
- URL: https://www.wjgnet.com/2307-8960/full/v10/i21/7531.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i21.7531
Osteoporotic vertebral compression fractures (OVCF) are one of the most common fragility fractures. Although most patients gradually relieve their symptoms after several weeks of conservative treatment, about 1/3 of patients still have persistent pain and discomfort. OVCF in about 10% of patients may develop into delayed vertebral collapse after trauma[1]. Named after the German surgeon who described the disease for the first time in 1985[2], Kummell’s disease is an occult fracture that originates due to untimely detection and treatment when the vertebral bone trabecular is damaged. Early and repeated exercises after the fracture hinders the healing process and eventually leads to nonunion of the fractured vertebra[3]. Therefore, Kummell's disease may be associated with osteoporosis, avascular necrosis of the vertebral body, biomechanical changes after fracture, and various factors[4]. Li et al[5] classified Kummell’s disease into three types: Type Ⅰ, with less than 20% compressed height of the vertebral body and no adjacent disc degeneration; type Ⅱ, with more than 20% compressed height of the vertebral body and usual adjacent disc degeneration; and type III, with spinal cord compression caused by the ruptured posterior cortex of the fractured vertebral body with or without neurological symptoms.
Due to the characteristics of type III Kummell’s disease, open surgery is usually considered as the standard approach[6]. These surgeries include, but are not limited to, solidified bone cement combined with short-segment pedicle screw fixation, titanium mesh graft combined with pedicle screw fixation, spinal resection combined with short-segment fixation, or posterior osteotomy combined with long-segment fixation[7]. However, if a patient with type III Kummell’s disease was accompanied by various medical conditions and refused to receive an open surgery, the treatment options are limited. In addition to pain management, the purpose of percutaneous vertebroplasty (PVP) surgery is to strengthen the fractured vertebral body and prevent further collapse. Thus, the difficulty in the application of PVP in this disease lies in how to relieve the compression of the spinal cord resulting from the fractured vertebral bone block. In this case report, we admitted a patient with type III Kummell’s disease and spinal cord compression by bone block who refused to undergo open surgery. A novel method, namely the use of traditional Chinese medicine manipulative reduction (TCMMR) combined with PVP, was introduced. TCMMR was used to restore the height of the compressed vertebral body and reduce the symptoms of spinal cord compression by bone block. PVP was then used to relieve pain, solidify and strengthen the fractured vertebral body, and prevent further collapse. The combined application of the two treatment methods resulted in satisfactory treatment outcomes of the patient. We reported this case for two purposes: Introducing our novel approach and providing a reference method for doctors.
A 67-year-old female patient was admitted to our hospital with a complaint of "low back pain for 10 years, aggravated with right lower limb pain for 10 d".
The patient had recurrent low back pain for 10 years and had not received surgery. The pain had worsened in the past 10 d, accompanied by the symptoms of right lower limb pain due to spinal cord compression.
The patient had a series of conditions, including old spinal fractures (unknown reason), kyphosis, lumbar disc herniation, lumbar fusion, hypertension, cerebral infarction, chronic gastritis, dynamic sclerosis, lung disease, etc.
The patient was a 67-year-old Chinese woman, a non-smoker with a blood type of B rhesus positive, and her body mass index was 25.0 kg/m2 (height 155 cm and weight 60 kg).
The patient presented with the following conditions: Spinal kyphosis with apex at L1; lumbar spine movement restriction; local tenderness, percussion pain, centered on the lumbar vertebral body; grade 5 left lower limb and grade 4 right lower limb muscle strength; normal sensation on the left leg, but decreased sensation on the right leg; negative straight leg raise test for the left lower limb, and positive straight leg raise test for the right lower limb; negative Babinski sign bilaterally; no edema in both lower limbs; and normal peripheral blood supply. The patient rated 7 scores on the preoperative pain visual analog scale and a D degree for the Frankel spinal cord score.
Laboratory exam results were all within normal range.
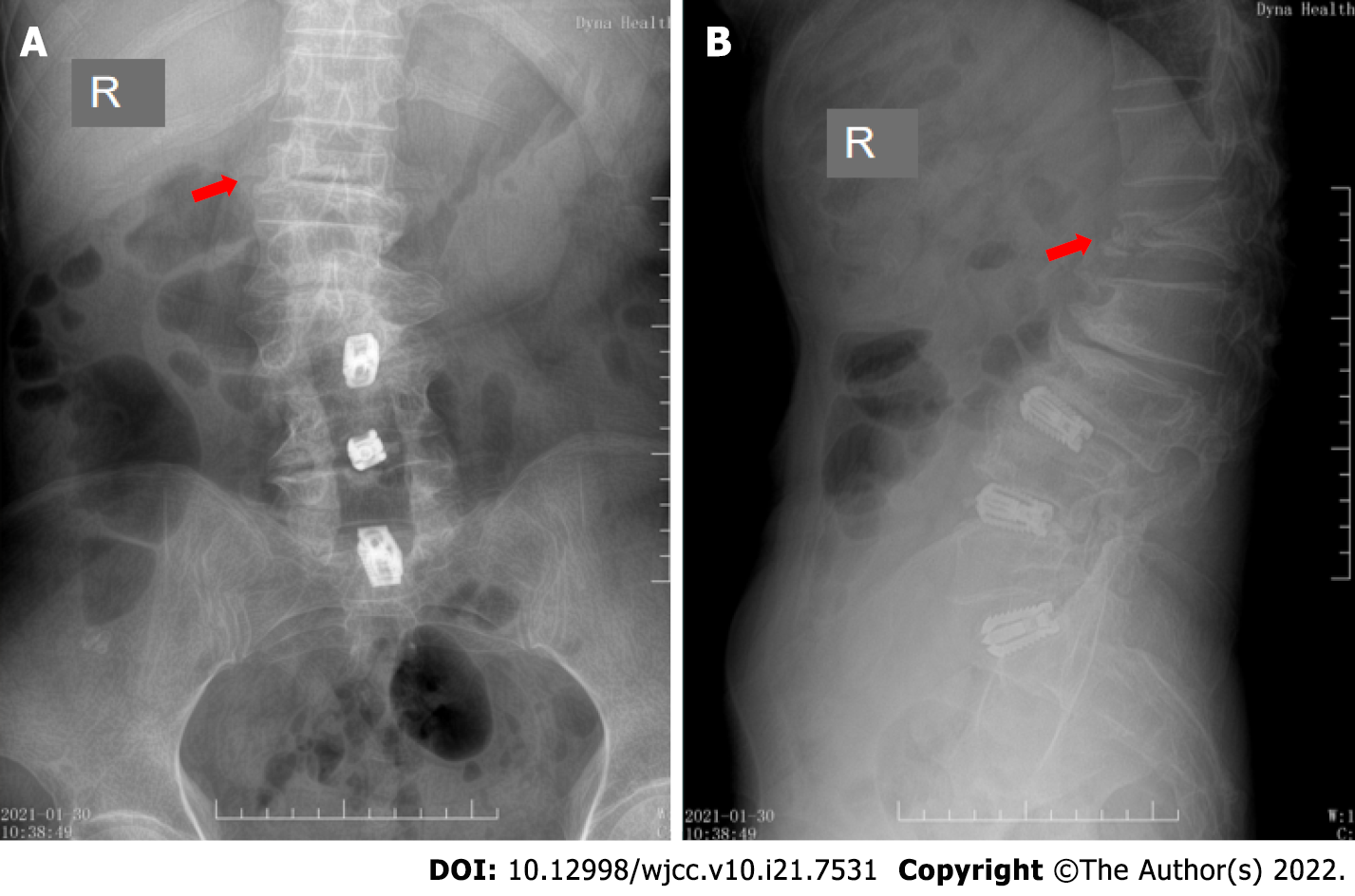
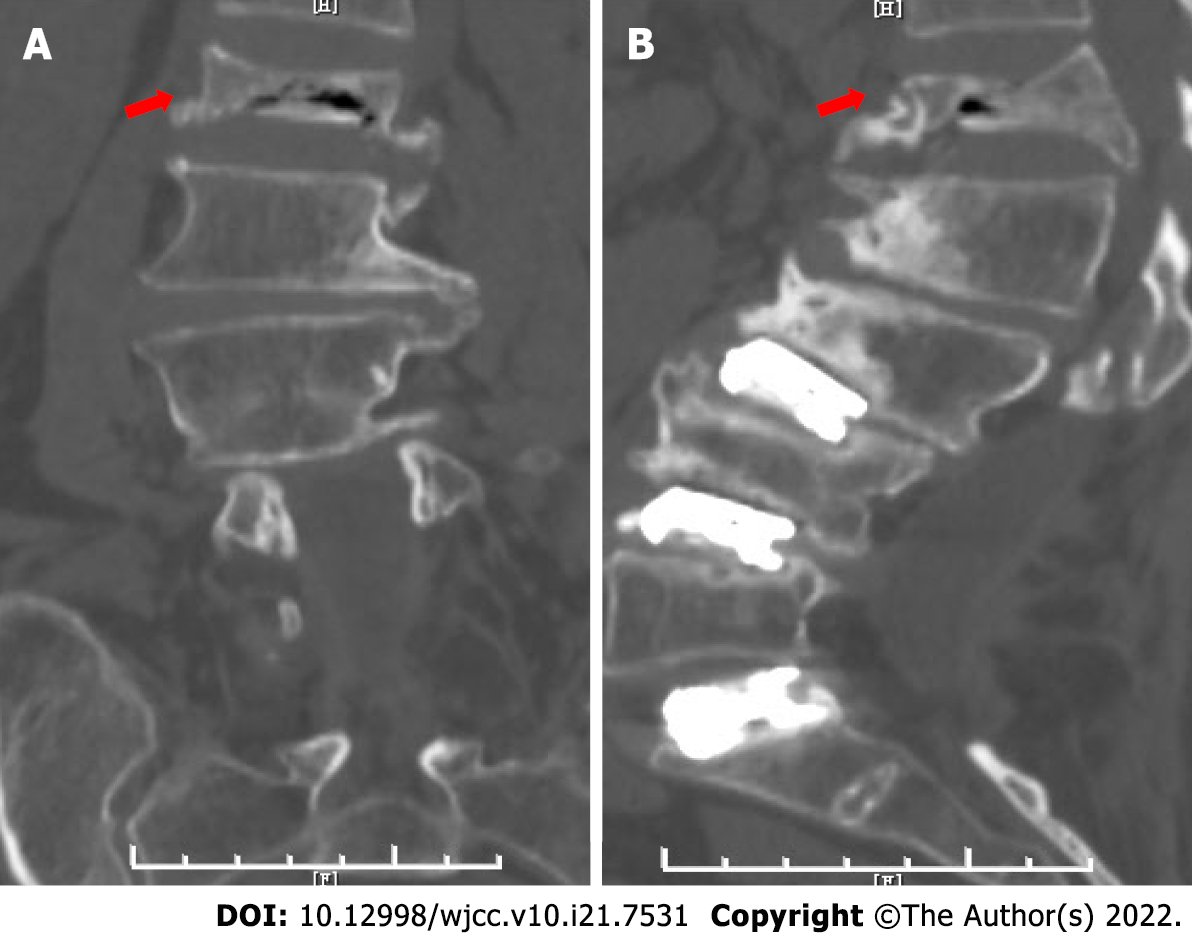
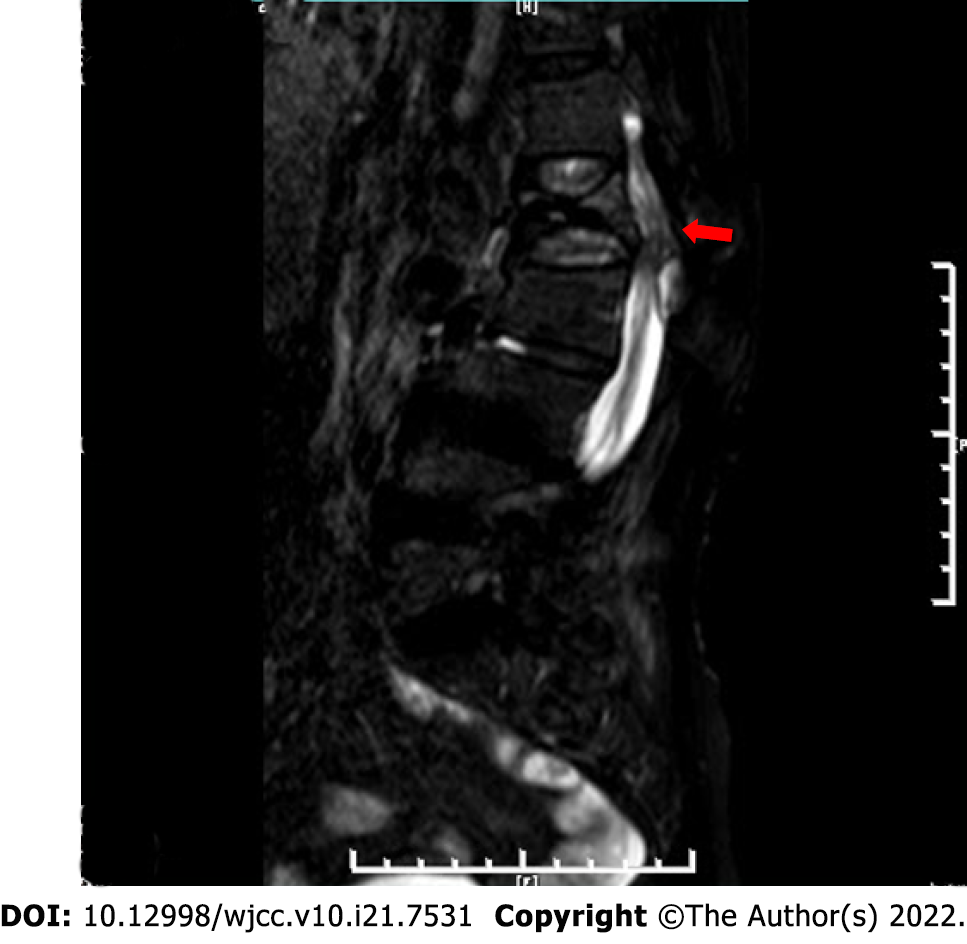
Preoperative X-ray showed an OVCF of the first lumbar vertebra, with compression on the anterior edge of the vertebral body (Figure 1). Preoperative computed tomography indicated that the first lumbar vertebra body had collapsed and that there was a bone block behind the vertebral body, which compressed the spinal cord (Figure 2). Preoperative magnetic resonance imaging revealed that the first lumbar vertebral body was collapsed, and that the spinal cord was compressed by a bone block of the fractured vertebral body (Figure 3). These results demonstrated that the patient had first lumbar OVCF, corresponding horizontal dural sac compression, and spinal stenosis. The imaging examination was conducted with the patient lying supine because of her inability to assume standing position during the examination.
Type III Kummell’s disease with spinal cord compression by bone block was diagnosed based on the medical history, physical examination, and imaging assessments.
The specific operation process of TCMMR was as follows. The patient was transferred into a prone position on the operating table after applying painkillers. One assistant held the patient firmly from the armpit, while the other assistant held the patient’s ankles to provide fixation. At the same time, the surgeon put his hands on the spinous process of the fractured vertebrae on the patient’s back and used it as a fulcrum to apply a posterior-anterior reduction force (Figure 4). As a result, the height of the compressed vertebra body was reset so that the kyphotic deformity gradually became smaller and the symptoms of right lower limb pain became less severe at the end of the treatment. The patient’s posture also remained unchanged during the following PVP process. The specific operation process of PVP was as follows. The puncture entry point of PVP was located in the outer upper part of the pedicle under C-arm X-ray fluoroscopy. The tissue between the skin and the fractured vertebral periosteum was anesthetized layer by layer. Then, the 20-30 degree outward direction was chosen to insert the puncture needle until the needle tip reached about the anterior and middle 1/3 regions of the vertebrae. Due to this, the tip was close to or slightly over the midline of the vertebral body. Then, high-viscosity bone cement was reconciled to toothpaste-like matter and slowly injected into the fractured vertebral body until the body was filled and diffused satisfactorily while maintaining the reset vertebral height by filling a sufficient amount of bone cement. Subsequently, the original position was held for about 5 min till the bone cement had completely hardened before the puncture needle was removed. The operation took 27 min, and went very smoothly.
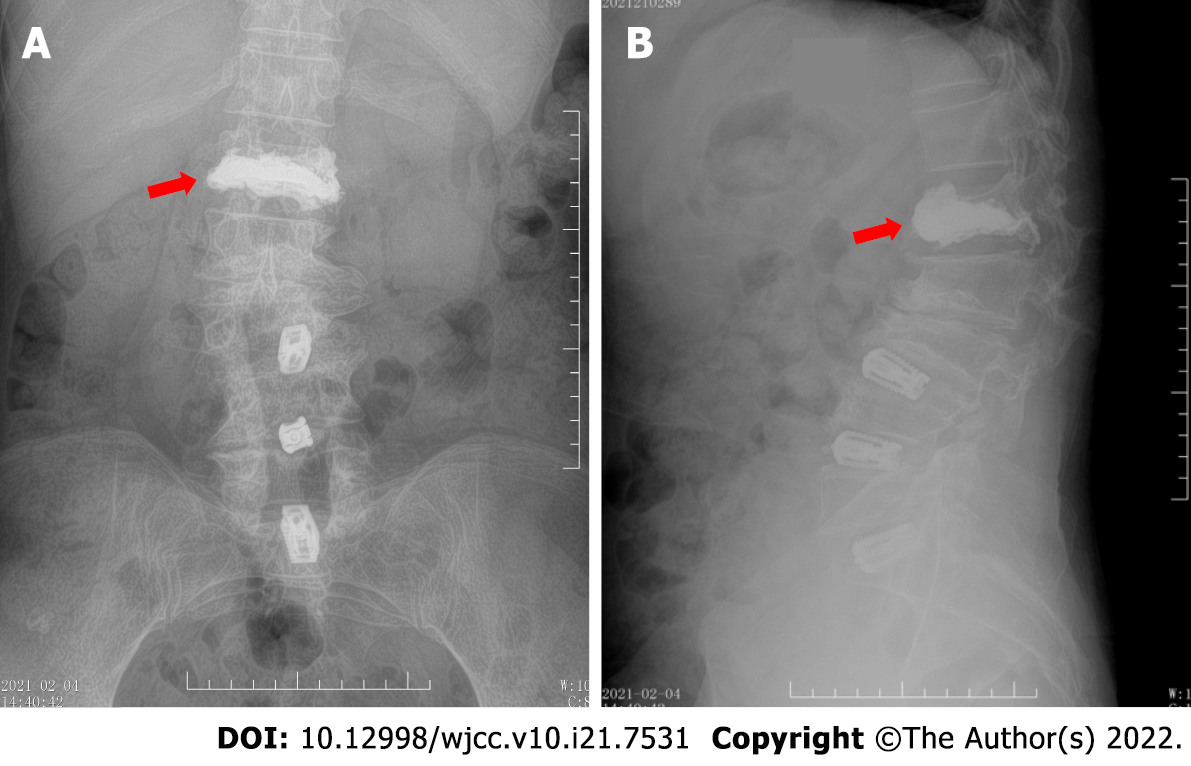
After the surgery, the patient had a pain visual analog score of 2, indicating that the back pain was relieved significantly. The patient also had a Frankel spinal cord scale of E degree with no right lower limb pain symptoms. The patient could walk on her own 2 h after the operation, and was discharged from the hospital within 48 h. Postoperative X-ray depicted that the height of the anterior edge of the compressed first lumbar vertebrae was increased (Figure 5). The patient was delighted with this treatment plan and the outcome; however, she could not be reached for follow-up appointments.
Kummell’s disease is a rare type of nonunion OVCF, also known as delayed vertebral collapse after trauma, post-traumatic osteonecrosis of the vertebral body, vertebral prosthesis, and vacuum fissure in the vertebral body. The etiology of Kummell’s disease is still unclear. It is generally believed that, after OVCF, avascular necrosis can lead to the collapse of the vertebral body, as well as the formation of false joints. Type III Kummell's disease is characterized by rupture and destruction of the vertebral body’s posterior wall, causing the fractured bone block to compress the dural sac. However, this compression is often formed slowly, with or without the symptom of spinal cord injury. Most patients with type III Kummell's disease receive open surgeries to alleviate the compression of the spinal cord. Surgical treatment with PVP is not generally recommended because of the challenge relieving spinal cord compression caused by vertebral bone block while restoring the height of the compressed vertebrae.
In this study, a type III Kummell's disease patient with spinal cord compression by bone block was reported. She was accompanied by a series of medical ailments which caused poor physical fitness for withstanding open surgery. She also refused the open surgery and insisted on having PVP surgery. After careful consideration, PVP was chosen despite the considerable challenges to the process, such as being prone to serious bone cement leakage, poor distribution, risk of paralysis, and the dilemma of relieving spinal cord compression while restoring the height of the compressed vertebral body.
Initially, we attempted to find answers from the literature database. However, we could not find any reports on PVP in treating type III Kummell's disease with spinal cord compression by bone block. Instead, we came up with the idea of applying TCMMR method. The use of TCMMR in the treatment of spinal thoracolumbar compression fractures has a long history dating back to the ancient Chinese Yuan Dynasty[8]. The most important reason for our choice of TCMMR combined with PVP was that we had successfully treated many patients with OVCF using this combined method, achieving satisfactory results for resetting the compression vertebral height[9,10]. The TCMMR uses the spinous process of the fractured vertebral body as a fulcrum to reduce the force of continuous elastic pressing to the ventral side. During the process, the shortened anterior longitudinal ligament is gradually stretched and the upper and lower intervertebral discs adjacent to the fractured vertebral body are jointly distracted by the fractured vertebral body to restore its height gradually.
However, in this case, there were two major differences. One was that the fractured vertebral body had formed a false joint - the posterior edge of the vertebral body was the movable joint point, and the front vertebral body could be opened or closed up and down along the endplate. The other difference was the presence of a fractured bone block behind the connected fractured vertebral body, which compressed the spinal cord and caused painful symptoms in the right lower limb. This meant that when this joint was opened, the bone block at the back would also move forward. In other words, the bone block behind the vertebral body compressing the spinal cord was prone to gradually move forward during the reduction process, which had the effect of reducing spinal cord compression. Because of these differences, we decided to treat this patient with TCMMR combined with PVP. Our new method relieved the symptom caused by the disease and met the patient’s requirement of minimally invasive surgery. Meanwhile, it also achieved the purpose of strengthening the fractured vertebral body and preventing further collapse.
The advantages of this combination therapy are as follows. (1) TCMMR restored the height of the compressed vertebral body to reshape the body and reduce kyphosis. The partial correction of the kyphosis reduced the tension at spinal cord stenosis, restored the spinal canal space at partial stenosis, and allowed the spinal cord to escape; (2) The bone block behind the vertebral body was moved forward, which reduced the compression of the bone block on the spinal cord; (3) After TCMMR, the horizontal direction had a narrow and long reduction cavity, which allowed the smooth entry of the puncture needle into the vertebral body and the diffusion distribution of the bone cement. The cavity not only increased the contact area of the bone cement, bone tissue, and the dispersion volume of the bone cement, but also reduced the risk of severe bone cement leakage depending on the injection pressure for dispersion[11]; (4) Unilateral PVP was used to achieve a reasonable bilateral distribution of bone cement and avoid serious leakage by adjusting the injection site, direction, angle, and flow direction of the bone cement, which also saved the patient’s possible cost of a bilateral PVP; (5) PVP increased the stability of the fractured vertebral body while reducing the stimulation of the spinal cord from the bone in the spinal canal; and (6) In particular, it was important to emphasize that TCMMR did not increase the treatment cost, and was safe and feasible since it was implemented before the PVP operation and only took about 5 min, which would not significantly affect the total operation time.
We believe that this combined method has some aspects that need attention for future operations: (1) The patient's imaging examination data should be carefully studied and the condition of the fractured vertebral body at preoperative should be evaluated to estimate the possible therapeutic effect; (2) TCMMR should be completed under X-ray fluoroscopy. The process should be gentle, and the strength should be moderate enough to resist the muscles. TCMMR that is too powerful may cause new damage or fracture[12]; (3) Communication with the patient should be maintained during the TCMMR process, and the patient's feelings should be known in time to avoid body position changes in response to pain; (4) The primary purpose of TCMMR was to restore the height of the fractured vertebra and correct the kyphosis. It could be used repeatedly, but should not forcefully restore the height to prevent overcorrection[9]; (5) TCMMR could only maintain a short-term effect on the fractured vertebra, and the vertebral body was still affected by the surrounding ligaments and muscle contraction. Therefore, the patient should remain in the reset position until the cement is fully solidified; and (6) The bone cement injection process was prone to leakage, so timely fluoroscopy monitoring is needed. Toothpaste-like bone cement should be selected for injection in small doses. If the bone cement is too thin, it will leak easily, while cement that is too thick is difficult to disperse. Once bone cement leakage occurs, the injection position and direction are required to be adjusted to prevent further leakage. If it still leaks after adjustment, the injection of bone cement should be stopped.
In this case report, the combined method of TCMMR and PVP was introduced. The results provide a reference for the treatment of type III Kummell’s disease patients with spinal cord compression by bone block symptoms who are not suitable for open surgery.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cheng TH, Taiwan; Yap RVC, Philippines S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Pappou IP, Papadopoulos EC, Swanson AN, Cammisa FP Jr, Girardi FP. Osteoporotic vertebral fractures and collapse with intravertebral vacuum sign (Kümmel's disease). Orthopedics. 2008;31:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Kummell H. Die rarefizierende ostitis der wirbelkorpe. Deutsche Med. 1895;21:180-181. |
| 3. | Zhao M, Wang J, Chen Y, Zhong Y, Feng H, Zhao D. Progress of Diagnosis and Treatment of Kummell's Disease. Med Recapitul. 2020;26:1989-1993. [DOI] [Full Text] |
| 4. | He D, Yu W, Chen Z, Li L, Zhu K, Fan S. Pathogenesis of the intravertebral vacuum of Kümmell's disease. Exp Ther Med. 2016;12:879-882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Li KC, Wong TU, Kung FC, Li A, Hsieh CH. Staging of Kümmell's disease. J Musculoskelet Res. 2004;8:43-55. [RCA] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Huang YS, Ge CY, Feng H, Zhang HP, Niu XB, Shi SY, Zhu ZQ, Hao DJ. Bone Cement-Augmented Short-Segment Pedicle Screw Fixation for Kümmell Disease with Spinal Canal Stenosis. Med Sci Monit. 2018;24:928-935. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Zhang XB, Hua Z, Yin J, Wang JW. Treatment on Kummell's disease. Chin J Osteoporos Bone Miner Res. 2020;13:73-78. [DOI] [Full Text] |
| 8. | Song R, Zheng H, Zhou Y, Zhao G. Analysis of Clinical Efficacy of Pingle Boning Manual Reduction Combined with Pereutaneous Vertebroplasty with High Viscosity of Bone Cement on Osteoporotic Vertebral Compressive Fracture in the Old Patients. J Emerg Tradit Chin Med. 2018;27:1348-1351. [DOI] [Full Text] |
| 9. | Guo A, Hao S, Meng S, Wei X, Li H, Liu S, Wang P, An X. Comparison of the effects of manipulative reduction combined with percutaneous vertebroplasty and simple percutaneous kyphoplasty in the treatment of thoracolumbar osteoporotic vertebral compression fractures. Chin J Bone Joint Injury. 2020;35:44-46. [DOI] [Full Text] |
| 10. | Li H, Hao S, Dong S, Liu S, Chen H, Zhang Z, Wang P, Yang X, Guo A. A clinical study of manipulative reduction combined with percutaneous vertebroplasty for treatment of osteoporotic vertebral compression fractures. J Trad Chin Orthop Trauma. 2020;32:6-11. |
| 11. | Liu J, Zhu X, Shi C. Manipulative reduction combined with percutaneous kyphoplasty for the treatment of thoracolumbar compression fractures. J Trad Chin Orthop Trauma. 2016;28:28-30. |
| 12. | Qiu J, Ji B, Wang M, Liu C. Vertebroplasty following fracture manipulation under traction for the treatment of osteoporotic thoracolumbar vertebral compression fractures. Int J Orthop. 2017;38:389-392. [DOI] [Full Text] |