Published online Jul 26, 2022. doi: 10.12998/wjcc.v10.i21.7523
Peer-review started: January 24, 2022
First decision: March 23, 2022
Revised: April 1, 2022
Accepted: June 3, 2022
Article in press: June 3, 2022
Published online: July 26, 2022
Processing time: 168 Days and 4.3 Hours
Neuralgia is frequently noted in patients with Kummell’s disease, and its mechanism is complex, rendering it challenging to treat. Percutaneous kyphop
In our patient, three vertebrae were involved. The collapse of T11 was particularly severe. After managing T8 and T9 using PKP, these two segments were effectively strengthened; consequently, back pain was significantly relieved. However, the structure and strength of T11 could not be effectively restored using a minimally invasive surgical method because there was little room for cement injection. This caused obvious neuralgia according to the postoperative status of the PKP. Thus, we performed selective nerve blocks for the treatment of neuralgia, which resulted in satisfactory outcomes.
Selective nerve block may be a possible therapeutic strategy for neuralgia due to severely collapsed vertebrae in Kummell’s disease.
Core Tip: Percutaneous kyphoplasty is not optimal for managing severely collapsed vertebrae, as cement injection may not be feasible. In our patient, the structure and strength of T11 could not be effectively restored by using a minimally invasive surgical method. However, it caused obvious neuralgia. Thus, a selective nerve block was used to treat the neuralgia, which led to satisfactory outcomes. These results indicate that selective nerve block may be an optional therapeutic measure for neuralgia due to severely collapsed vertebrae in patients with Kummell’s disease who are not candidates for conventional surgery.
- Citation: Zhang X, Li ZX, Yin LJ, Chen H. Selective nerve block for the treatment of neuralgia in Kummell’s disease: A case report. World J Clin Cases 2022; 10(21): 7523-7530
- URL: https://www.wjgnet.com/2307-8960/full/v10/i21/7523.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i21.7523
Kummell’s disease is characterized by delayed osteoporotic vertebral compression fractures (OVCFs) following minor or no trauma. It was first reported by Kummell in 1895[1]. Osteoporosis, avascular necrosis of the vertebra, and delayed union are the main pathological features[2-4]. The course of the disease is long, and the extent of vertebral compression is often severe. Neuralgia frequently occurs in such patients; however, because of its complex mechanism, treatment is challenging[5,6]. Percutaneous kyphoplasty (PKP) has been widely used for the treatment of OVCFs, showing satisfactory pain relief and markedly improved clinical outcomes. However, PVP/PKP is not optimal for managing severely collapsed vertebrae, as bone cement injection may not be feasible. We recently performed a selective nerve block for the treatment of neuralgia caused by severely collapsed vertebrae in a patient with Kummell’s disease, with satisfactory outcomes.
An 82-year-old woman presented with progressive pain in the upper back, costal area, and lateral region of the lower abdomen.
The pain developed approximately 2 mo ago. No traumatic causes were identified. Initially, the patient was able to walk with an aid. However, a few days later, the patient was unable to stand upright. As the symptoms worsened, she experienced constant pain, with no relief despite posture switching. Administration of tramadol did not ease the pain.
The patient was in good physical condition. She had been diagnosed with hypertension for many years; however, hypotensive drugs had not been prescribed for a long time. She had no history of diabetes, heart disease, tumors, or surgery.
The patient had no relevant family history, particularly of osteoporotic vertebral compressed fractures.
Physical examination revealed extensive pain in the chest and back region, with limited spinal movement. Sharp tenderness and pain on percussion were detected in the spinous processes at T8 and T9. Hyperalgesia was noted in the bilateral costal and lateral lower abdominal regions. The Visual Analog Scale (VAS) score was 9 for each region. No radiating pain was observed in the lower limbs. Moreover, the sensation and muscle force were normal. The Oswestry Disability Index (ODI) was 82.5% on admission[7].
Preoperative laboratory examinations such as routine blood tests, liver function, kidney function, and coagulation function did not indicate significant contraindications.
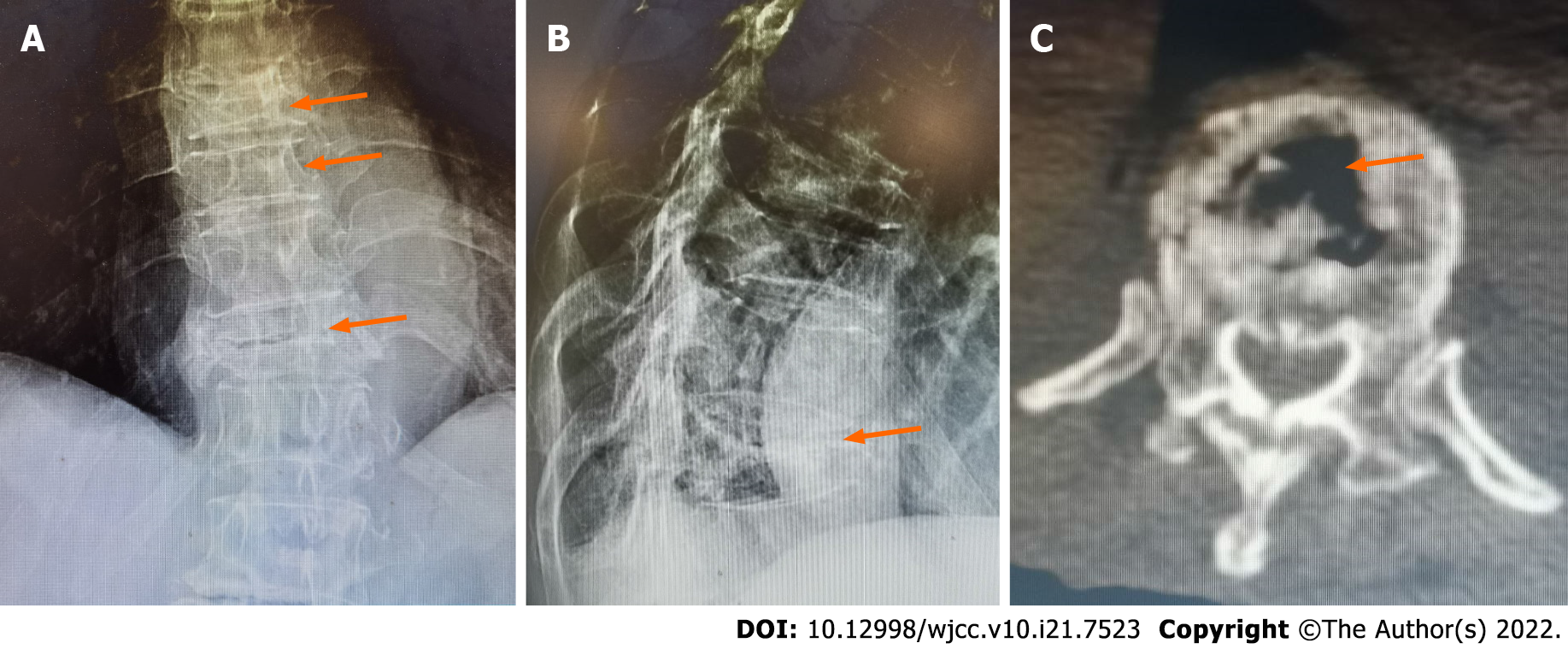
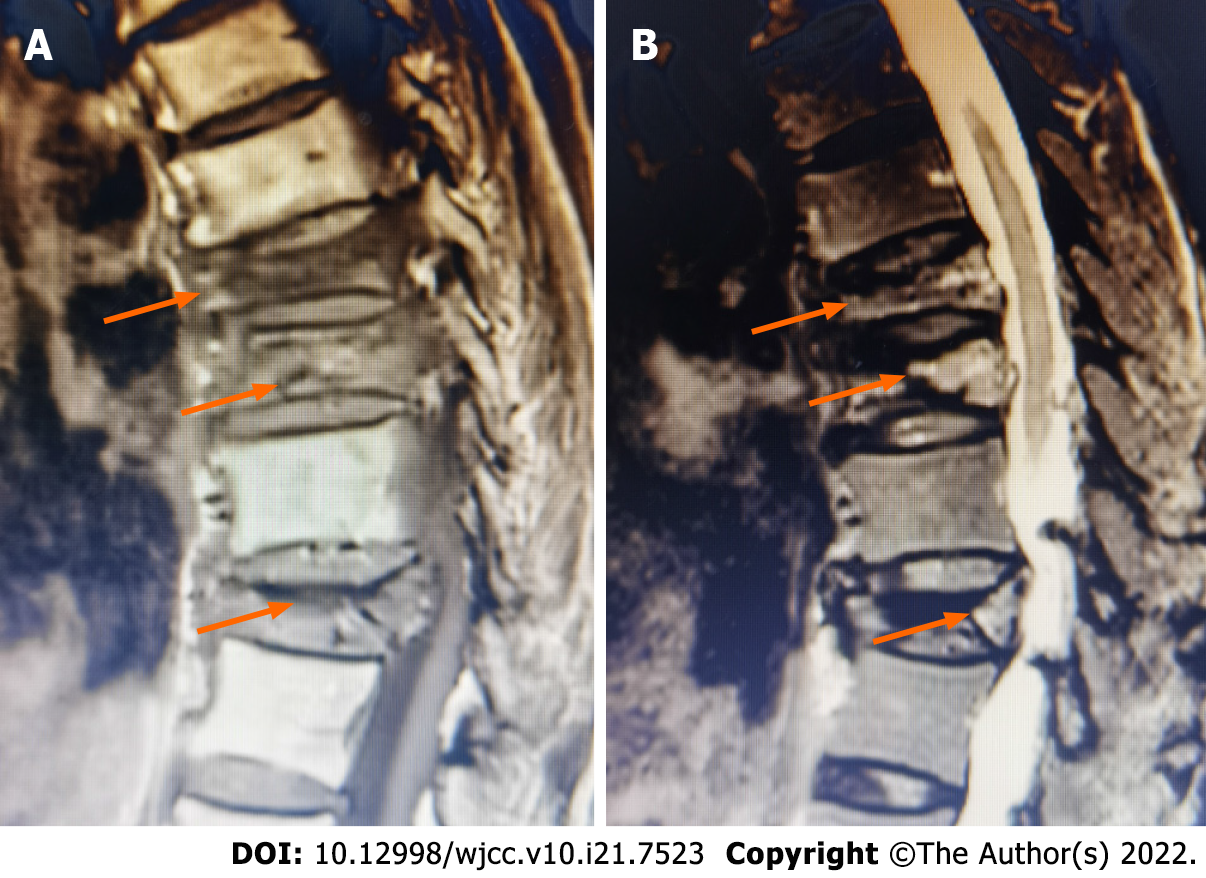
Radiographs revealed that the T8, T9, and T11 vertebrae were dramatically flattened (Figure 1A and B). The vertebral compression rate was > 90% at T11. Computed tomography revealed the “vacuum cleft sign” on horizontal sections of the vertebrae (Figure 1C)[8,9]. Sagittal T1-weighted magnetic resonance (MR) images revealed bone marrow replacement with asymmetrical low signal intensities (Figure 2A). Sagittal T2-weighted MR images showed mixed signal intensity within the vertebral body and a linear area of hyperintensity surrounded by hypointensities (double-line sign) (Figure 2B)[10,11]. Bone mineral density assessment revealed a T-value of -3.0 in L3.
The final diagnoses were as follows: (1) osteoporotic vertebral compression fractures and (2) Kummell’s disease.
To preoperative assessment, the main challenges were as follows: The first was age, as the patient was an older woman (82 years old). Thus, traditional surgery for open reduction and internal fusion fixation was highly risky. Additionally, this technique is not optimal for osteoporotic vertebral fractures. Second, three vertebrae had compressed fractures; despite PKP being performed for T8 and T9, the collapse of T11 was particularly severe, precluding bone cement injection. Moreover, the patient’s symptoms revealed significant neuralgia in the costal and lateral lower abdominal regions. However, it could not be determined whether this neuralgia was closely related to the 11th thoracic nerve and intercostal nerve. Therefore, the questions were whether the neuralgia persisted after PKP of T8 and T9 and how it should be further treated.
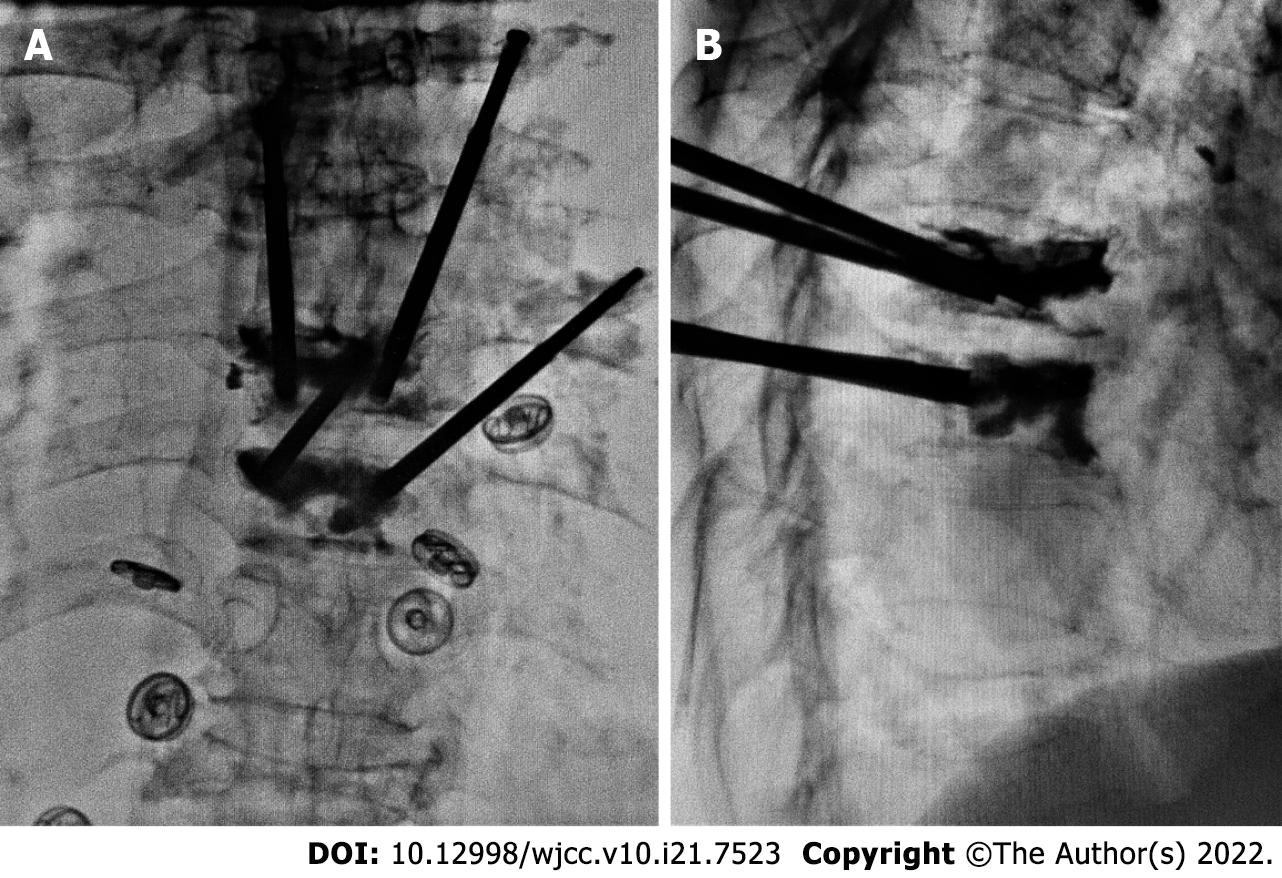
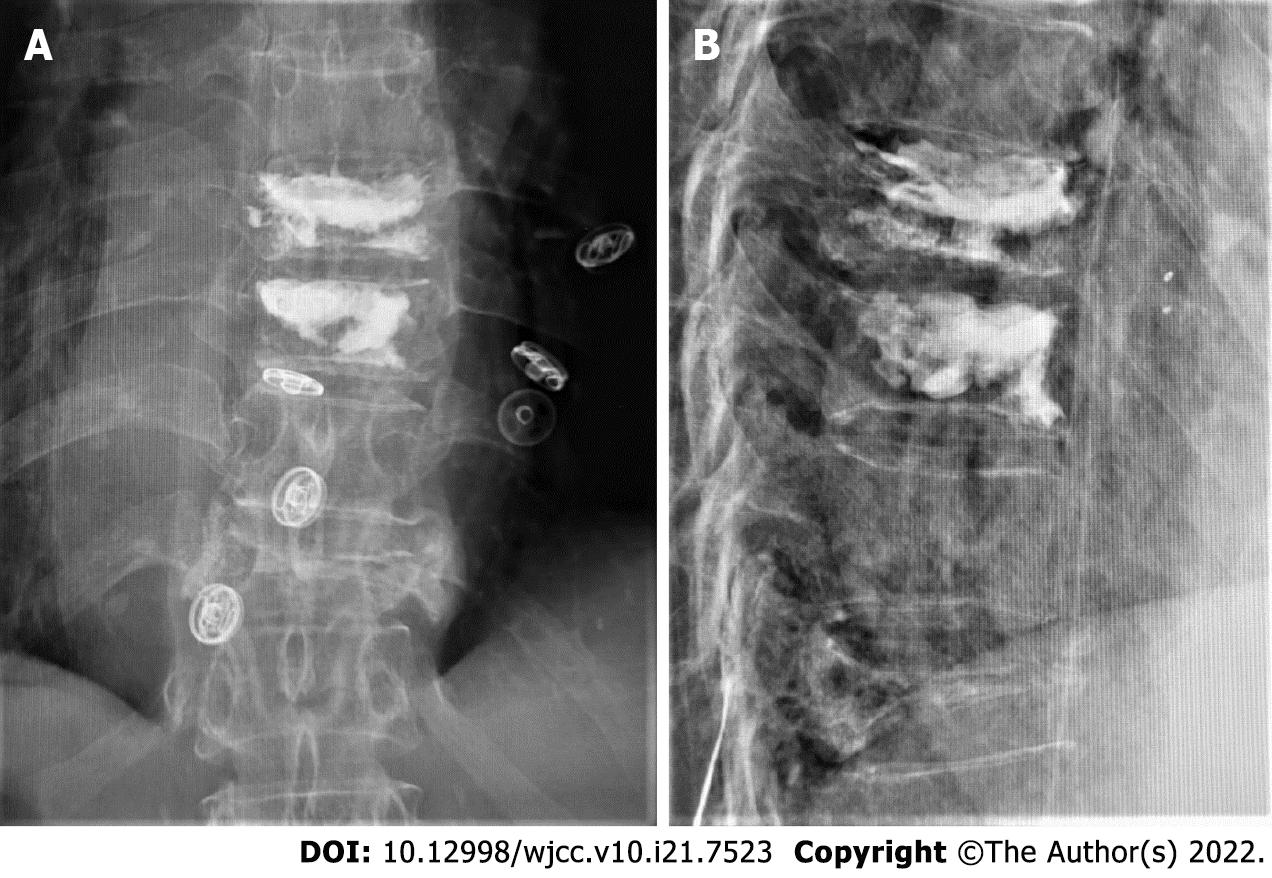
PKP was performed at T8 and T9 with the patient in the prone position. The procedure was performed under local anesthesia with 1% lidocaine, 2 d after admission. The injection volume was 3 mL for each vertebra. Both vertebrae received bone cement injections via the bilateral channels (Figure 3). The procedure was successfully completed, and postoperative radiography revealed that the bone cement was well distributed without marked leakage in the canalis spinalis (Figure 4).
The patient’s chest and back pain were significantly relieved postoperatively. The VAS scores of these regions decreased to 2 points 24 h after surgery. However, pain in the costal and lateral regions of the lower abdomen persisted, with a postoperative VAS score of 6 points. The distribution of pain was mostly in the region innervated by the dorsal ramus of the 11th thoracic spinal nerve and 11th intercostal nerve. These results suggested that severe collapse of the 11th thoracic vertebra remained a major source of pain. The characteristics of the pain were consistent with neuralgia caused by nerve compression resulting from a severe deformity of the vertebral column.
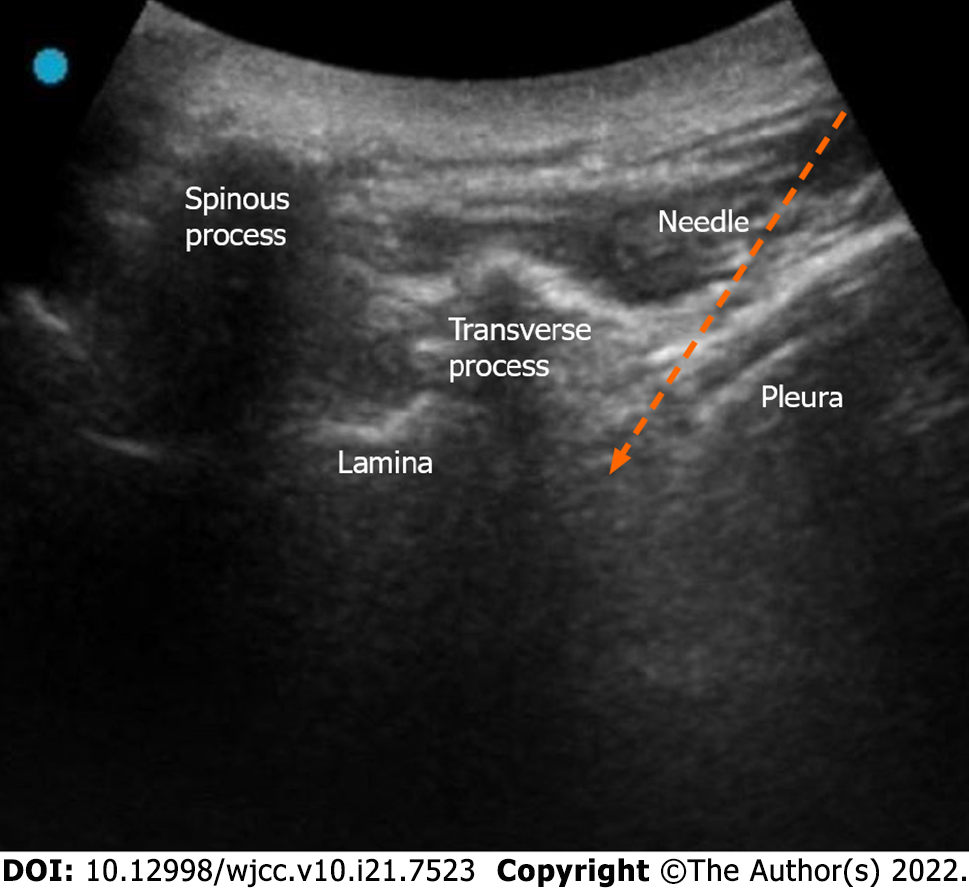
To treat the remnant neuralgia, ultrasound-guided selective nerve block was performed on the dorsal ramus of the 11th thoracic spinal nerve and the 11th intercostal nerve, which was performed once per day for 3 d starting from day 2 after PKP.
The specific procedure of the selective nerve block was as follows: the patient was placed in the prone position. The spinous process at T12 was first determined by palpation of the 12th rib. The spinous process of T11 could then be located adjacent to the proximal region. After the local skin was disinfected, a disposable sterile towel was used. An ultrasound instrument (FUJIFILM SonoSite Inc. Bothell, WA, United States) was set to the musculoskeletal mode. A low-frequency ultrasonic probe covered with a disposable sterilized lens cover was placed on the surface of the spinous process of T11 along the short axis. As the probe slid laterally, the echoes of the spinous process, lamina, and transverse process were constantly observed. On the lateral deep surface of the transverse process, the pleura could fluctuate with respiration. The gap between the pleura and lateral deep surface of the transverse process was the target region for the puncture (Figure 5). Local infiltration anesthesia was performed with 1% lidocaine, approximately 1 cm from the lateral side of the probe. The in-plane technique was adopted. The needle was initially inserted at an angle of approximately 40 degrees to the horizontal plane. After reaching the surface of the transverse process, the needle was slightly pulled back, and the puncture angle was increased to approximately 60 degrees. The needle was then inserted again following the new path toward the target region. No gas or blood was drawn from the suction syringe, confirming that the needle did not penetrate the pleura or blood vessels. An initial volume of 1% lidocaine (0.5 mL) was injected to confirm diffusion toward the foramina. Subsequently, 2 mL 1% lidocaine was injected into the region. The injection in this region diffused to the 11th thoracic nerve root. The needle then receded slightly near the upper edge of the pleura. A volume of 2 mL 1% lidocaine was injected into this region in the same manner. The injection in this region would likely spread following the direction in which the nerve root exited the foramina and would therefore affect the intercostal nerve.
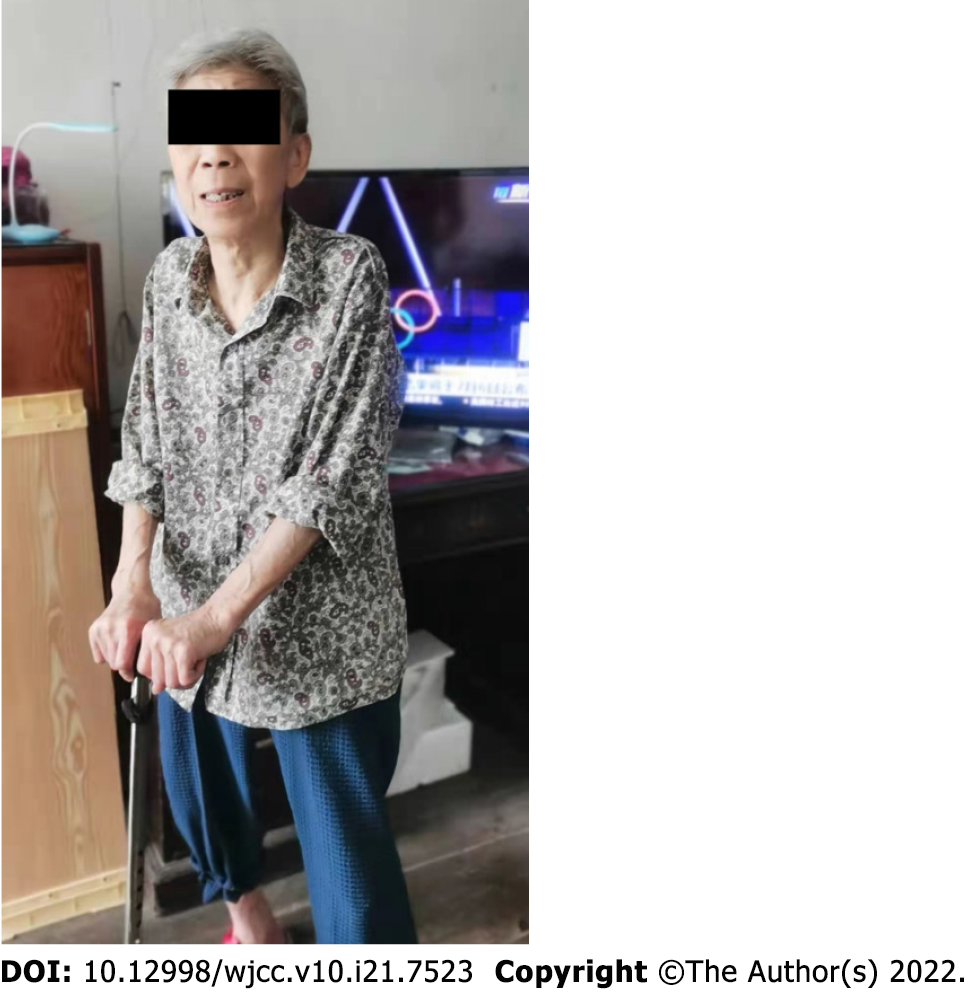
After three selective nerve block treatments, the patient reported significant pain relief in the costal and lateral regions of the lower abdomen. The VAS scores of these regions dropped to 3 points. Meanwhile, the VAS score of her chest and back remained at 2 points, with no fluctuation. The treatment was then continued once per week from day 7 after surgery for a total of three times. This caused the final VAS score of each region to decrease to 1. At the 3-mo follow-up visit, the VAS score of each region was maintained at 1 point, and the ODI decreased to 40% (Figure 6).
The typical clinical features of Kummell’s disease include progressive back pain, delayed vertebral collapse, and kyphosis. Patients may also have no clear history of trauma. Radiological findings provide important evidence for diagnosis, such as the typical intravertebral vacuum cleft sign[8,9]. MR imaging findings vary among individuals. Asymmetrical hypointensities in T1-weighted images and a linear area of hyperintensity surrounded by hypointensities (double-line sign) are representative changes[10,11]. These manifestations were clearly observed in this patient.
The features of Kummell’s disease are different compared to those of common OVCFs. Patients are often very elderly (aged over 80 years). Furthermore, the severity of vertebral compression and complexity of symptoms increase with duration. All these features impact the management strategy, outcome efficacy, functional outcomes, and complications.
Pain associated with Kummell’s disease is complex. However, the specific mechanisms responsible are unknown, and the following confounding factors might influence the choice of management: abnormal biomechanics and an excessive load on facet joints after fracture, irritation of nerve roots caused by the reduction in vertebral height, articular process, distortion and edema of foraminal ligaments, stimulation of the superior thalamus, and excitation of sympathetic pathways and adjacent short neural circuits as a result of the accumulation of mediators[12-16]. Data from real-world clinical practice have revealed that the manifestation of pain tends to be much more diverse.
Recent studies have shown that patients often also have intractable neuralgia, which is the key determinant of remnant pain following PKP[12,17,18]. The incidence of intercostal neuralgia in patients with lower thoracic compression fractures has been reported to be 28.6%[17]. Neuralgia mainly manifests as diffuse radiating pain along the area innervated by the intercostal nerve and lower abdomen. The patient in this report demonstrated these typical symptoms, and three corresponding vertebrae were involved, with the T11 collapse being particularly severe. Following the management of T8 and T9 with PKP, these two segments were effectively strengthened, which significantly relieved back pain. However, the structure and strength of T11 could not be effectively restored using a minimally invasive surgical method because there was little room for cement injection. Moreover, this is an obvious cause of neuralgia and a critical dilemma in treatment. Recent studies have proposed short-segment fusion combined with PKP as a therapeutic strategy for patients with Kummell’s disease with severely compressed vertebrae; however, this has not been extensively used in very old people[5,19,20].
Ultrasound-guided selective nerve block presented advantages in the treatment of our patient because of its ability to precisely block the innervating nerve in the area of neuralgia. It has been reported that selective blocking of the dorsal ramus can effectively relieve the pain of patients with OVCFs[12,18]. This procedure is minimally invasive and has a reduced risk of complications. Steroids were not administered to our patient. We believe that the probable mechanism underlying the effectiveness of selective nerve block is the breakdown of the vicious cycle of neuromuscular pain responses. Various components of the cycle, including biomechanical instability, neurosensitization, and myofascial overload, are effectively controlled through neural regulation.
The successful clinical outcomes reported herein indicate that selective nerve block may be an optional therapeutic measure for neuralgia due to severely collapsed vertebrae in patients with Kummell’s disease who are not candidates for conventional surgery.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chao A, Taiwan; Tsuchiya M, Japan A-Editor: Zhu JQ, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Kummell H. Die rarefizierende ostitis der wirbelkorper. Deutsche Med. 1895;21:180-181. [RCA] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Ito Y, Hasegawa Y, Toda K, Nakahara S. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J. 2002;2:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 97] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 3. | Kim KT, Suk KS, Kim JM, Lee SH. Delayed vertebral collapse with neurological deficits secondary to osteoporosis. Int Orthop. 2003;27:65-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 65] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Kim HS, Adsul N, Bang JS, Singh R, Park CH, Jang IT. Refracture of Kummell Disease Combined with Huge Epidural Hematoma After Minor Trauma. World Neurosurg. 2018;120:500-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Li KC, Li AF, Hsieh CH, Liao TH, Chen CH. Another option to treat Kümmell's disease with cord compression. Eur Spine J. 2007;16:1479-1487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 62] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Lee SH, Cho DC, Sung JK. Catastrophic intramedullary hematoma following Kümmell's disease with large intravertebral cleft. Spine J. 2008;8:1007-1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25:2940-52; discussion 2952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3162] [Cited by in RCA: 3753] [Article Influence: 150.1] [Reference Citation Analysis (0)] |
| 8. | Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology. 1978;129:23-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 186] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Mirovsky Y, Anekstein Y, Shalmon E, Peer A. Vacuum clefts of the vertebral bodies. AJNR Am J Neuroradiol. 2005;26:1634-1640. [PubMed] |
| 10. | Yu CW, Hsu CY, Shih TT, Chen BB, Fu CJ. Vertebral osteonecrosis: MR imaging findings and related changes on adjacent levels. AJNR Am J Neuroradiol. 2007;28:42-47. [PubMed] |
| 11. | van der Schaaf I, Fransen H. Percutaneous vertebroplasty as treatment for Kummell's disease. JBR-BTR. 2009;92:83-85. [PubMed] |
| 12. | Wilson DJ, Owen S, Corkill RA. Facet joint injections as a means of reducing the need for vertebroplasty in insufficiency fractures of the spine. Eur Radiol. 2011;21:1772-1778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Jinkins JR, Whittemore AR, Bradley WG. The anatomic basis of vertebrogenic pain and the autonomic syndrome associated with lumbar disk extrusion. AJR Am J Roentgenol. 1989;152:1277-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Kuniya H, Aota Y, Kawai T, Kaneko K, Konno T, Saito T. Prospective study of superior cluneal nerve disorder as a potential cause of low back pain and leg symptoms. J Orthop Surg Res. 2014;9:139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 15. | Maigne JY, Lazareth JP, Guérin Surville H, Maigne R. The lateral cutaneous branches of the dorsal rami of the thoraco-lumbar junction. An anatomical study on 37 dissections. Surg Radiol Anat. 1989;11:289-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 60] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Kraan GA, Hoogland PV, Wuisman PI. Extraforaminal ligament attachments of the thoracic spinal nerves in humans. Eur Spine J. 2009;18:490-498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Choi HJ, Yang HJ, Lee SH, Park SB. The effect of vertebroplasty on costal pain related to osteoporotic thoracic compression fractures in elderly patients. Korean J Spine. 2012;9:98-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Lin LJ. Clinical observation of radiofrequency thermocoagulation of thoracic spinal nerve for intercostal neuralgia after compression fracture of thoracic vertebrae. Zhongwai Yixue Yanjiu. 2019;17:37-39. [DOI] [Full Text] |
| 19. | Lu W, Wang L, Xie C, Teng Z, Han G, Shi R, Liang J, Lu S. Analysis of percutaneous kyphoplasty or short-segmental fixation combined with vertebroplasty in the treatment of Kummell disease. J Orthop Surg Res. 2019;14:311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Park SJ, Kim HS, Lee SK, Kim SW. Bone Cement-Augmented Percutaneous Short Segment Fixation: An Effective Treatment for Kummell's Disease? J Korean Neurosurg Soc. 2015;58:54-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |