Published online Jul 26, 2022. doi: 10.12998/wjcc.v10.i21.7467
Peer-review started: November 24, 2021
First decision: April 13, 2022
Revised: April 28, 2022
Accepted: June 3, 2022
Article in press: June 3, 2022
Published online: July 26, 2022
Processing time: 229 Days and 4.5 Hours
Although tumors of the lacrimal sac are rare, they represent a potentially life-threatening situation that can easily be overlooked since patients present with features consistent with chronic dacryocystitis. Lacrimal sac squamous cell carcinoma is the most common lacrimal sac malignancy, but no definitive treatment is currently available.
We describe a 34-year-old unmarried male who presented with a red and swollen right lower eyelid, which gradually developed into a mass of the lower eyelid that obstructed vision in his right eye. He was treated with transcatheter arterial infusion chemotherapy and interventional embolization based on the tumor characteristics, and we also administered intensity-modulated radiotherapy and targeted therapy after tumor shrinkage. The tumor treatment demonstrated good efficacy, and the patient’s condition was stable after 10 mo of follow-up.
To our knowledge, this is the first report of lacrimal sac squamous cell carcinoma treated with transcatheter arterial infusion chemotherapy and interventional embolization, which might expand clinical treatment options for lacrimal sac carcinoma.
Core Tip: Tumors of the lacrimal sac are extremely rare but are potentially devastating lesions that lack an effective remedy. We present a case of lacrimal sac squamous cell carcinoma that was treated with transcatheter arterial infusion chemotherapy and interventional embolization to provide a reference for the treatment of primary lacrimal sac tumors.
- Citation: Sun MH, Yi WD, Shen L, Zhou L, Lu JX. Transcatheter arterial infusion chemotherapy and embolization for primary lacrimal sac squamous cell carcinoma: A case report. World J Clin Cases 2022; 10(21): 7467-7473
- URL: https://www.wjgnet.com/2307-8960/full/v10/i21/7467.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i21.7467
Lacrimal sac tumors are classified as either primary and secondary tumors, and most secondary maxillary tumors originate from adjacent structures, such as the paranasal sinuses, or they metastasize from distant organs such as the brain[1]. Primary lacrimal sac tumors are rare, but their malignancy rate is 55%-100%[2]. Primary lacrimal sac malignancies are represented by squamous cell carcinoma, metastatic epithelial carcinoma, or neoplastic adenocarcinoma according to their cell morphology, and no definitive treatment is currently available.
Digital subtraction angiography–guided arterial infusion chemotherapy and embolization of tumor-supplying arteries have provided a new treatment method for neoplastic lesions[3,4]. Here, we present a case of primary lacrimal sac squamous cell carcinoma treated with transcatheter arterial infusion chemotherapy and interventional embolization, which showed good efficacy, thus providing a reference for the treatment of primary lacrimal sac tumors.
The patient was a 34-year-old unmarried male who worked in farming and was admitted to the hospital on August 5, 2019, due to a chief complaint of a right orbital mass with right nasal obstruction for more than 2 mo.
In June 2019, the patient noticed redness and swelling of the lower right eyelid; this swelling gradually developed into a mass on the lower eyelid that obstructed his vision. He visited another hospital for treatment and received intermittent anti-infective therapy with antibiotics based on a diagnosis of right nasolacrimal abscess with sphenoid sinusitis. Treatment slightly alleviated the redness and swelling. Over the next month, his symptoms recurred, and the right orbital mass gradually grew and ulcerated. Moreover, the patient developed visual impairment in his right eye, right nasal obstruction, and an odor caused by local infection. No photophobia or lacrimation was observed during the disease course. He experienced no pain, itching, epileptic seizure, headache, dizziness, cold intolerance, fever, nausea, or vomiting.
Clavicular fracture was treated with internal fixation 10 years before this incident.
He had no family history of similar diseases and denied previous special drug use.
The physical examination performed at admission showed an Eastern Cooperative Oncology Group performance status of 1. Examinations of his heart, lung, and abdomen revealed no special findings. Palpation of the neck revealed no enlargement of the superficial lymph nodes. Specialized examination: His visual acuity was 1.2 in the left eye, and he had light sensation in the right eye. Intraocular pressure: The intraocular pressure in the right eye could not be measured, and that in the left eye was 20 mmHg. The infraorbital mass in the right lacrimal sac was as large as a duck egg, and a small, ulcerated area was evident on the surface. The mass pushed the eyeball upward and outward, which damaged the medial and inferior rectus muscles and complicated eyelid opening. The mass exhibited moderate rigidity and demonstrated adhesion to the maxillary tissue and was thus unmovable. The submandibular gland was also enlarged. The preauricular and cervical lymph nodes were enlarged with little mobility but were without redness or tenderness. No enlargement of the axillary lymph nodes was observed. No abnormality was found in the left eye on fundus examination. Lacrimal passage irrigation indicated no obstruction in the left eye and showed reflux from the lower lacrimal punctum to the upper lacrimal punctum without purulent exudate in the right eye. Otolaryngology revealed hyperemia and edema in the right nasal mucosa, obvious inward shifting of the lateral wall of the right nasal cavity, and hyperemia and ulceration in the mucosa of the middle and lower nasal passages (easy bleeding). No obvious secretion or mass was found in either nasal passage (Figure 1A and B).
No obvious abnormality was found in tests for infectious diseases, such as human immunodeficiency virus, syphilis, and hepatitis C.
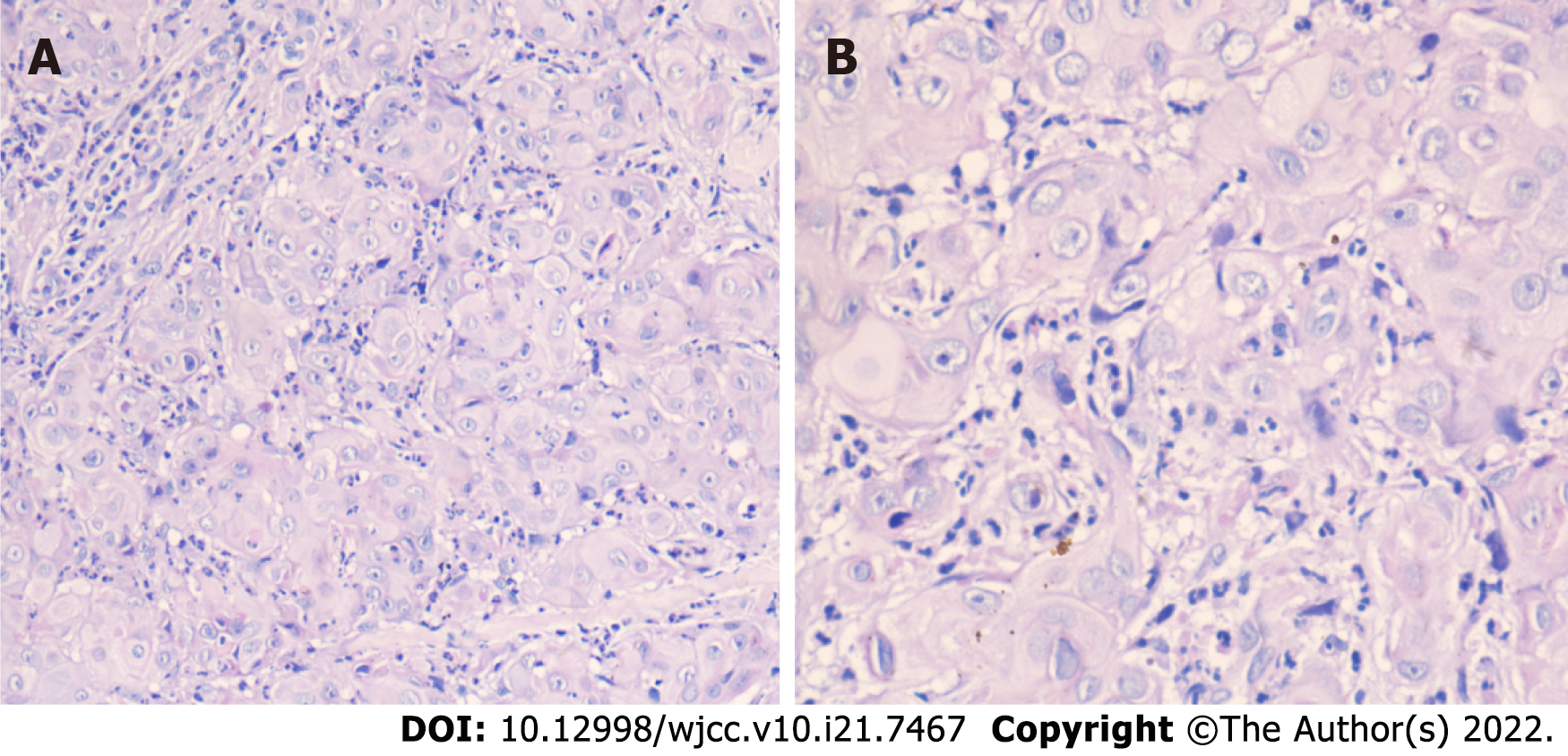
Pathological examination: On August 8, 2019, right lacrimal sac tumor biopsy was performed under local anesthesia. Pathological examination indicated moderately differentiated squamous cell carcinoma. Immunohistochemistry showed that the tumor was CK19 (+), CK20 (-), GCDFP-15 (-10), P40 (+), p53 (+), p63 (+), and CK5/6 (+). Hematoxylin–eosin (HE) staining: The primary lacrimal sac squamous cell carcinoma exhibited a nest-like arrangement of many tumor cells of different sizes and their stromal infiltration by microscopy at 200 × magnification. Under 400 × magnification, tumor cells were clearly atypical and large in size with pink cytoplasm, a high nucleus-to-cytoplasm ratio, and both visible and pathological mitosis. The pathological manifestations seen by HE staining are shown in Figure 2A and B.
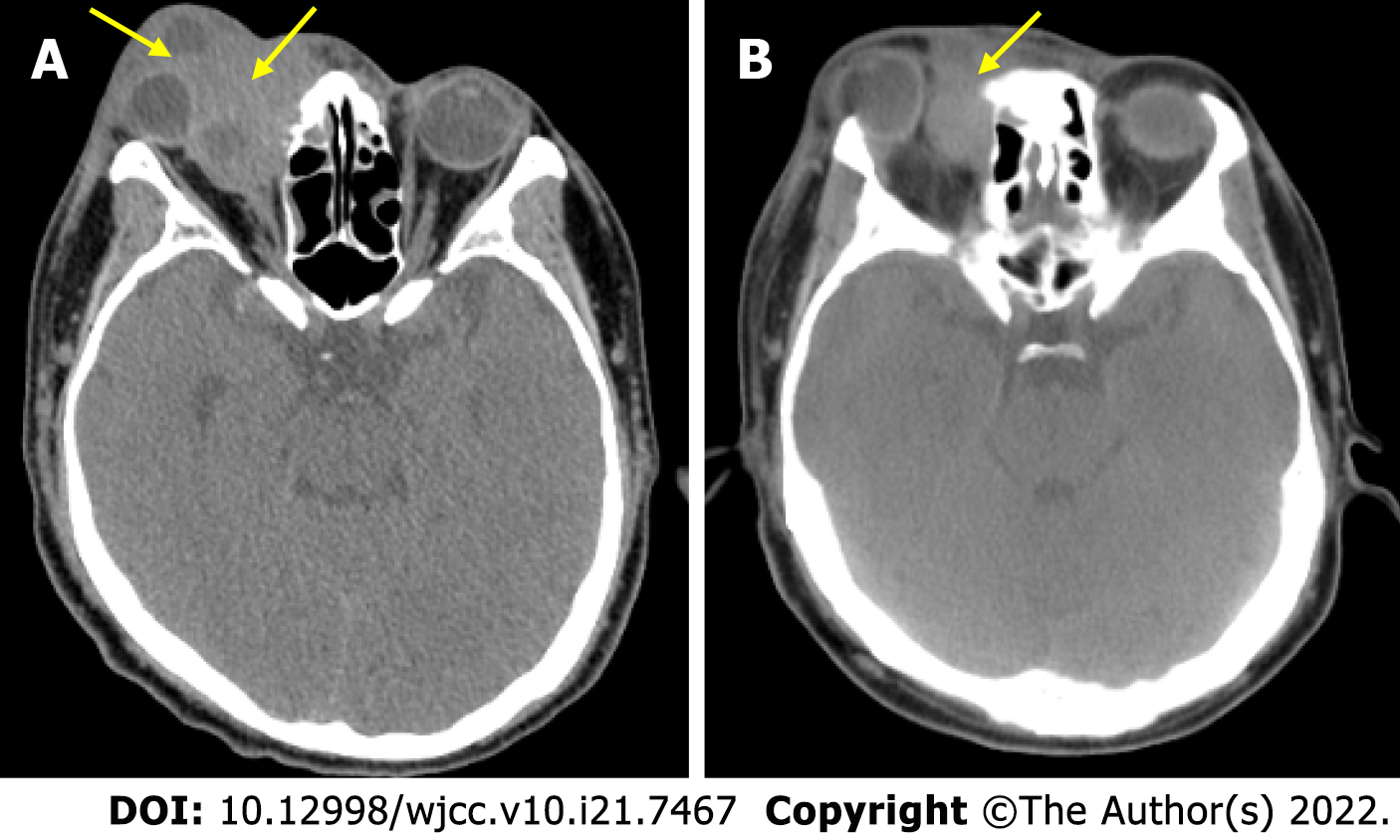
Eye computed tomography (CT) + reconstruction performed on August 5, 2019 showed the following: (1) The nature of the soft tissue mass (52 mm × 60 mm × 65 mm) in the right orbit was uncertain. The bones in the inner wall, top wall, and orbital plate of the right maxillary sinus had been destroyed and absorbed. Hypoattenuating areas were observed in the right maxillary sinus, nasolacrimal duct, and orbital medial wall, and the right eyeball was displaced; and (2) Multiple nodular lymph nodes in the right parotid region were enlarged (Figure 3A).
The patient was diagnosed with lacrimal sac squamous cell carcinoma according to medical history, clinical features, and auxiliary examinations.
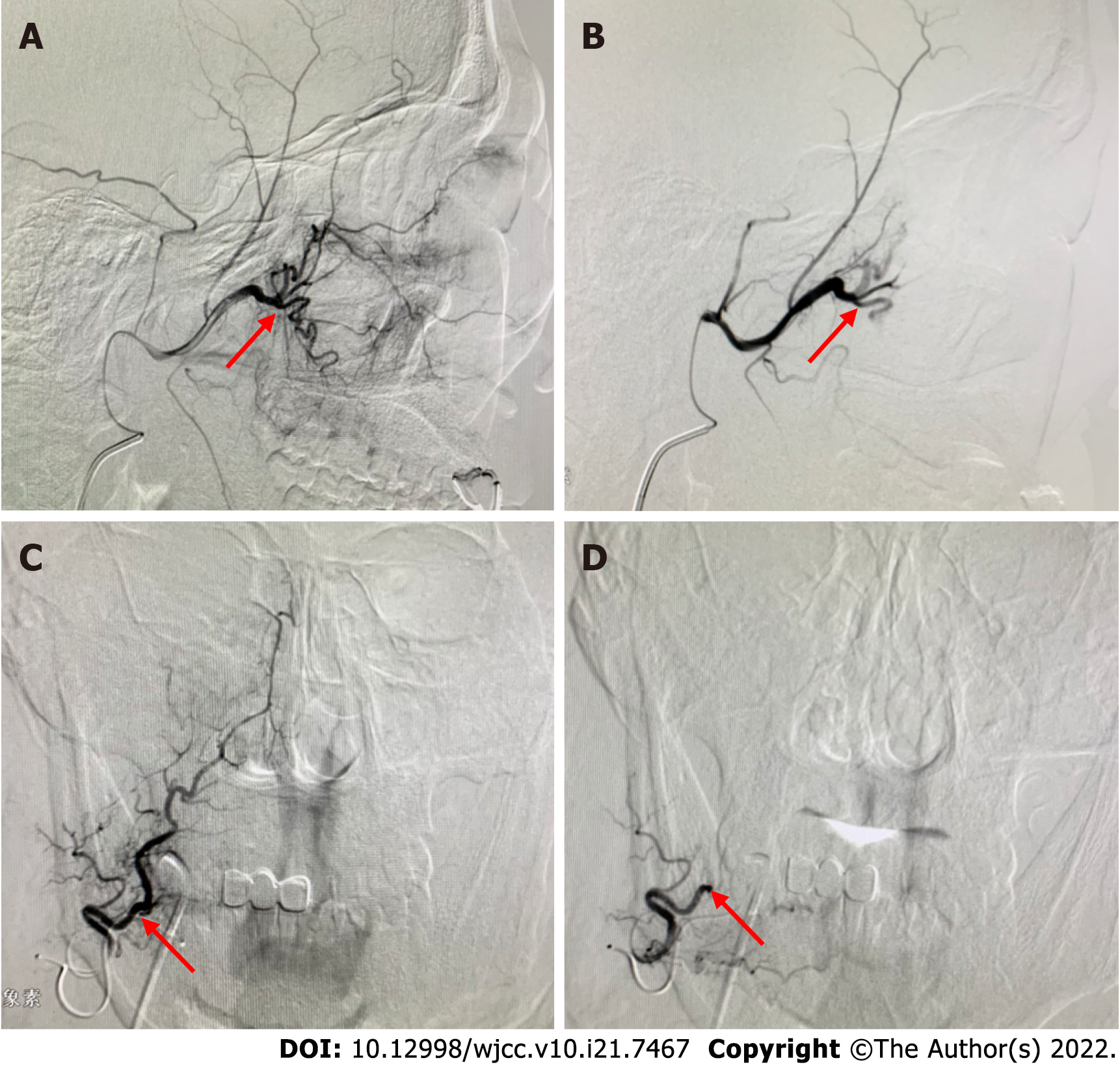
According to the patient’s tumor characteristics, after communicating with the patient and his family and obtaining signed informed consent, we initiated arterial infusion chemotherapy in the intervention room for the right lacrimal sac carcinoma on August 20, 2019. Procedure: The right common carotid artery was catheterized via a 5F single-curved catheter (Terumo, Japan) using the right femoral artery approach. Angiography revealed a lesion with a rich blood supply, tumor staining, and unclear margins (approximately 4 cm) in the right maxillary sinus and orbital region; this lesion was supplied by the right maxillary artery branch and zygomatico-orbital artery branch. No arteriovenous fistula was identified (Figure 4A). A microcatheter (single-curved, 2.6F, Terumo) was successively inserted into the blood-supplying arteries of the tumor. A complete dose of 80 mg lobaplatin in 250 mL of 0.9% NaCl (0.32 mg/mL) and 120 mg docetaxel in 250 mL of 0.9% NaCl (0.48 mg/mL) was initially given for infusion chemotherapy, after which polyethylene microspheres (300-500 μm) were added for embolization. After embolization, angiography revealed no obvious tumor staining. The surgery was performed without complications (Figure 4B).
On September 24, 2019, the second interventional therapy was given. Angiography showed a lesion in the maxillary sinus and orbital areas that was richly supplied by the maxillary artery branch and facial artery branch (Figure 4C). A microcatheter (single-curved, 2.6F, Terumo) was inserted into the target vessels in succession, and 80 mg lobaplatin and 120 mg docetaxel were infused. Then, polyethylene microspheres (300-500 mm) loaded with 50 mg pirarubicin were added as drug-eluting beads for embolization until tumor staining disappeared (Figure 4D).
On October 1, 2019, the patient’s tumor had significantly shrunk, and he was able to open his right eye with greater ease; consequently, the visual impairment in his right eye and the right nasal obstruction were alleviated (Figure 1C and D). Head CT (noncontrast scan) performed on the same day showed the following: (1) The malignant space-occupying lesion (46 mm × 35 mm × 31 mm) in the right orbital lacrimal sac area was smaller compared with its size on August 23, 2019, while destruction of the adjacent bone was roughly the same; (2) The enlarged lymph nodes in the right parotid region were smaller compared with their size in 2019, and metastasis was considered; (3) Maxillary sinusitis, ethmoidal sinusitis, and sphenoidal sinusitis showed no obvious changes on either the right or left side; and (4) The right lateral ventricle was wider than the contralateral ventricle, and the midline had moved slightly to the left. No obvious intracranial space-occupying lesion was noted (Figure 3B).
From October 10 to November 20, 2019, intensity-modulated radiotherapy was administered in seven fields: 6 Mv-X DT PGTVnx (6 Mv X-ray, right eye tumor on imaging) 7037 cGy/31 f/6 W+ (a total of 7037 cGy, 31 times, more than 6 wk), PGTVnd-R (positive lymph nodes in the right parotid gland and neck), 6417 cGy/31 f/6 W+ (a total of 6417 cGy, 31 times, more than 6 wk), PTV1 (high-risk region) 6417 cGy/31 f/6 W+ (a total of 6417 cGy, 31 times, more than 6 wk), and PTV2 (low-risk lymph node drainage region) 5425 cGy/31 f/6 W+ (a total of 5425 cGy, 31 times, more than 6 wk) at 97% isodose to generally cover the targeted region. On October 10, November 1, and November 23, concurrent chemotherapy (lobaplatin 50 mg) was given. On November 25, bone marrow suppression was observed and treated with a white blood cell–boosting substance (recombinant human granulocyte colony-stimulating factor injection, 300 µg/d × 7 d). On December 20, 120 mg docetaxel and 50 mg lobaplatin were administered intravenously, which occurred without complications. The patient was unwilling to continue chemotherapy and instead received anlotinib (12 mg d1-14 per 3 wk). Follow-up until April 2020 showed that the patient’s lesion was stable. In May 2020, he discontinued treatment due to the financial burden.
Primary lacrimal sac tumors are rare, but more than 55% of these tumors are malignant[2]. Most lacrimal sac malignancies originate from the epithelium, and the majority are squamous cell carcinomas[5]. The most common clinical manifestations of lacrimal sac carcinoma are epiphora, local masses, and inflammation, which often cause obstruction of the lacrimal passage due to slow tumor growth[6]. Some patients are misdiagnosed with chronic dacryocystitis due to infection secondary to obstruction of the lacrimal passage by the tumor, but anti-infective therapy is usually ineffective. When the disease course is long and bloody secretions are observed, we should be highly suspicious of lacrimal sac carcinoma. The patient described in this study was misdiagnosed with dacryocystitis at the beginning of the disease course and did not respond to multiple anti-infective treatments; thus, we missed the optimal treatment window.
Due to the low incidence of primary lacrimal sac carcinoma, no high-value evidence-based medical treatment experiences have been reported. According to the available research and case reports, oncologists believe that radical surgical resection, radiotherapy, and chemotherapy are most beneficial in preventing and treating recurrence and metastasis of lacrimal sac tumors[7]. Surgical resection is the first choice for the treatment of early head and neck tumors and mid-stage or advanced local head and neck tumors. In our case, the tumor could not be completely removed by surgery because it had invaded nearby muscles and bones and had metastasized to the lymph nodes in the parotid region. Facial injuries sustained during surgery may also cause psychological harm[8]. Radiotherapy is a commonly used treatment for primary head and neck tumors, but we did not adopt this method as the first choice for two reasons. First, radiotherapy is a means of local treatment, during which the tumor may metastasize. Once the tumor metastasizes, radiotherapy can no longer control the lesion. Even if local radiotherapy shrinks the tumor, it cannot reverse or stop metastasis. Second, this tumor was large, and radiotherapy would have caused considerable damage to the surrounding normal tissues and might have led to serious complications, including blindness in the right eye. Although systemic chemotherapy may shrink the tumor, the systemic reaction is strong, and the drug concentration reaching the tumor tissue is limited.
Due to improvements in interventional technology and medical equipment, several studies have demonstrated the feasibility and safety of transcatheter arterial chemotherapy and embolization. Digital subtraction angiography–guided arterial infusion chemotherapy plus embolization of tumor supply arteries serves as a new treatment method for neoplastic lesions and can effectively inhibit tumor growth, potentially allow systematic drug treatment and prognosis improvement, and achieve good clinical treatment outcomes. Through arterial infusion chemotherapy, chemotherapy drugs can reach tumor cells at a higher concentration than that which reaches normal cells surrounding the tumor, which reduces both damage to normal cells and systemic reactions and kills tumor cells. In addition, after the drug is metabolized, the first-pass elimination effect weakens the systemic adverse reactions to chemotherapy[9]. Arterial infusion chemotherapy has advantages over other modalities including less trauma, simple execution, and a high success rate. Chemotherapy drugs can be injected in a targeted manner to reduce tumor volume, improve local structural changes, promote local functional recovery, and provide doctors with the opportunity to comprehensively evaluate the patient’s condition, formulate an individualized treatment plan, and reduce the incidence of complications and death[10].
In this case, arterial infusion chemotherapy and embolization achieved good results, reduced the tumor size, and provided favorable conditions for later radiotherapy and chemotherapy as the patient expected, but the treatment failed to improve the patient’s quality of life. The members of our research group considered that the tumor might have developed drug resistance, which may have led to the unsatisfactory efficacy of chemotherapy.
Primary lacrimal sac carcinoma is very rare, and no definitive treatment is currently available. In this patient, arterial infusion chemotherapy and embolization followed by chemotherapy and radiotherapy achieved some therapeutic effects but culminated in an unsatisfactory therapeutic response. We hope that our case report provides a good reference for the diagnosis and treatment of primary lacrimal sac squamous cell carcinoma.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Posa A, Italy A-Editor: Liu X, China S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
| 1. | Wladis EJ, Frempong T, Gausas R. Nasolacrimal metastasis from heptocellular carcinoma masquerading as dacryocystitis. Ophthalmic Plast Reconstr Surg. 2007;23:333-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Krishna Y, Coupland SE. Lacrimal Sac Tumors--A Review. Asia Pac J Ophthalmol (Phila). 2017;6:173-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Inchingolo R, Spiliopoulos S, Posa A, Tibana TK, Nunes TF, Memeo R. New frontiers in endovascular therapies for locally advanced hepatocellular carcinoma. Radiol Bras. 2021;54:130-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Pereira PL, Iezzi R, Manfredi R, Carchesio F, Bánsághi Z, Brountzos E, Spiliopoulos S, Echevarria-Uraga JJ, Gonçalves B, Inchingolo R, Nardella M, Pellerin O, Sousa M, Arnold D, de Baère T, Gomez F, Helmberger T, Maleux G, Prenen H, Sangro B, Zeka B, Kaufmann N, Taieb J. The CIREL Cohort: A Prospective Controlled Registry Studying the Real-Life Use of Irinotecan-Loaded Chemoembolisation in Colorectal Cancer Liver Metastases: Interim Analysis. Cardiovasc Intervent Radiol. 2021;44:50-62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Hodgson N, Whipple K, Lin JH, Brumund KT, Kikkawa DO, Korn BS. Bilateral squamous cell carcinoma of the lacrimal sac. Ophthalmic Plast Reconstr Surg. 2013;29:e149-e151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Lee LN, Scott AR, Chan AW, Frankenthaler RA. Management of transitional cell carcinoma of the lacrimal sac: a multidisciplinary approach to orbit sparing treatment. Laryngoscope. 2010;120 Suppl 4:S161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Goto T, Bandoh N, Nagato T, Takahara M, Harabuchi Y, Tokusashi Y, Miyokawa N. Primary small cell carcinoma of lacrimal sac: case report and literature review. J Laryngol Otol. 2010;124:1223-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Ramos A, Pozo CD, Chinchurreta A, García F, Lorenzo M, Gismero S. Adenoid cystic carcinoma of the lacrimal sac: case report. Arq Bras Oftalmol. 2016;79:333-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Kallini JR, Gabr A, Abouchaleh N, Ali R, Riaz A, Lewandowski RJ, Salem R. New Developments in Interventional Oncology: Liver Metastases From Colorectal Cancer. Cancer J. 2016;22:373-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Carne PW, Frye JN, Robertson GM, Frizelle FA. Stents or open operation for palliation of colorectal cancer: a retrospective, cohort study of perioperative outcome and long-term survival. Dis Colon Rectum. 2004;47:1455-1461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 109] [Article Influence: 5.2] [Reference Citation Analysis (0)] |