Published online Jul 26, 2022. doi: 10.12998/wjcc.v10.i21.7409
Peer-review started: November 7, 2021
First decision: January 11, 2022
Revised: January 22, 2022
Accepted: June 3, 2022
Article in press: June 3, 2022
Published online: July 26, 2022
Processing time: 246 Days and 5 Hours
Solitary necrotic nodule of the liver (SNNL) is a rare benign lesion with a complete necrotic core and a clear fibrous capsule containing elastic fibers. We present the case of a patient with a radiographic computed tomography (CT) finding of "ring"-like annular calcification within the lesion and postoperative pathologic diagnosis of necrotic nodules wrapped by dense fibers in liver tissue, as well as the patient's subsequent management and outcome.
A 38-year-old Chinese woman with a history of systemic lupus erythematosus treated with prednisone and hydroxychloroquine, without any symptoms, was found to have hepatic space-occupying lesions by imaging examination at a health examination. A subsequent CT scan suggested a space-occupying lesion of the liver with annular calcification, which was not defined to be benign or malignant. After that, a laparoscopic hepatic space-occupying resection was performed. The postoperative pathological diagnosis was necrotic nodules wrapped by dense fibers in the liver tissue, and the final diagnosis was SNNL. The patient had an uneventful postoperative recovery.
There is a "ring"-like calcification in SNNL. This patient had a history of systemic lupus erythematosus, without a history of parasite infection, trauma, or tumor. Therefore, whether the etiology and pathological changes of SNNL are related to rheumatic immune diseases remains to be investigated.
Core Tip: A 38-year-old woman with a history of systemic lupus erythematosus responded well to corticosteroids (prednisone) and hydroxychloroquine. A liver mass was found on examination, and subsequent computed tomography examination confirmed the liver mass with "ring"-like calcification, and thus malignancy was not ruled out. The patient received surgical treatment, and postoperative pathology showed necrotic nodules surrounded by dense fibers in the liver tissue. There were many lymphocytes and tissue cells around the nodules, which were consistent with isolated necrotic nodules in the liver. The patient is currently being followed.
- Citation: Bao JP, Tian H, Wang HC, Wang CC, Li B. Solitary necrotic nodules of the liver with "ring"-like calcification: A case report. World J Clin Cases 2022; 10(21): 7409-7414
- URL: https://www.wjgnet.com/2307-8960/full/v10/i21/7409.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i21.7409
Solitary necrotic nodule of the liver (SNNL) is a rare disease that is generally considered nonmalignant. It was first reported in 1983 by Shepard and Lee, who described four lesions with a completely necrotic core and a transparent fibrotic capsule containing elastic fibers. The pathogenesis of SNNL remains unknown. In their initial study, Shepard and Lee favored a traumatic or infectious etiology[1]. Sundaresan et al[2] found the presence of nourishing vessels within nodules, suggesting a hemangioma origin. They also described the central reticular fibers within the nodules, suggesting a sclerosing hemangioma origin. It has also been reported that SNNL may also demonstrate calcification[3]. Wang et al[4] studied 29 cases of SNNL and found that histopathological calcification was more likely to be used to confirm the diagnosis of SNNL. However, due to its non-specific features, SNNL is often mistaken for malignant lesions according to imaging[1,5]. A recent article questioned the traditional assumption that SNNLs are always benign, citing evidence of metastatic gastrointestinal carcinomas found in a small number of cases[6]. We report a patient with a previously indescribable imaging feature-annular calcification.
A 38-year-old Chinese woman was admitted to our Outpatient Department of Hepatobiliary Surgery for a space-occupying liver lesion.
No symptoms related to the hepatic mass were found, and no related treatment or management had been performed.
The patient had a history of systemic lupus erythematosus treated with prednisone and hydroxychloroquine. She had a history of cesarean section. She denied a history of other diseases, trauma or surgery. She had no abdominal tenderness or rebound pain and no palpable abdominal mass.
This patient had no special personal or family history.
The physical examination of the patient's abdomen revealed no abnormalities. The patient had a flat abdomen with no pigmentation of the abdominal skin. The patient had no abdominal tenderness or rebound pain, and no palpable abdominal mass.
No elevated tumor markers such as carcinoembryonic antigen, alpha-fetoprotein, and CA-199 were found. Eosinophil counts were normal. Alanine aminotransferase and aspartate aminotransferase were normal before operation. Increased alanine aminotransferase and aspartate aminotransferase were found after the operation. The indexes of other assay items were normal.
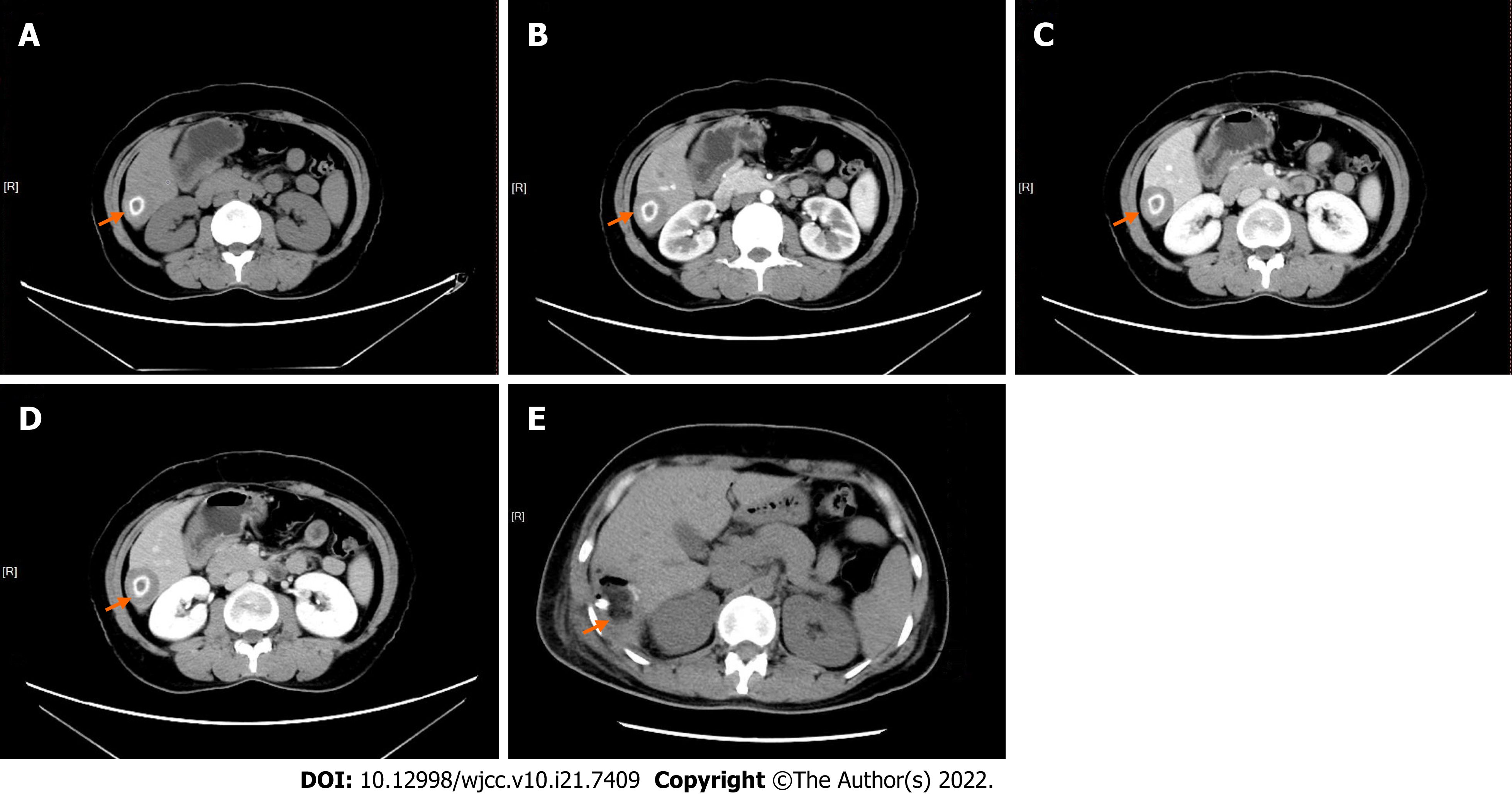
Abdominal computed tomography (plain + enhanced scans) revealed an isolated, low-density, round lesion (3.4 cm × 2.7 cm in size) in the sixth segment of the liver with a "ring" calcification of 1.5 cm in diameter. There was no enhancement in the arterial phase, portal vein phase, or delayed phase (Figure 1). No radiographic evidence of other abnormalities was observed. No magnetic resonance imaging (MRI) examination was performed.
Considering the patient’s history, laboratory examinations, and imaging examinations, she was diagnosed with a benign lesion of the liver, with the possibility of malignancy not being excluded.
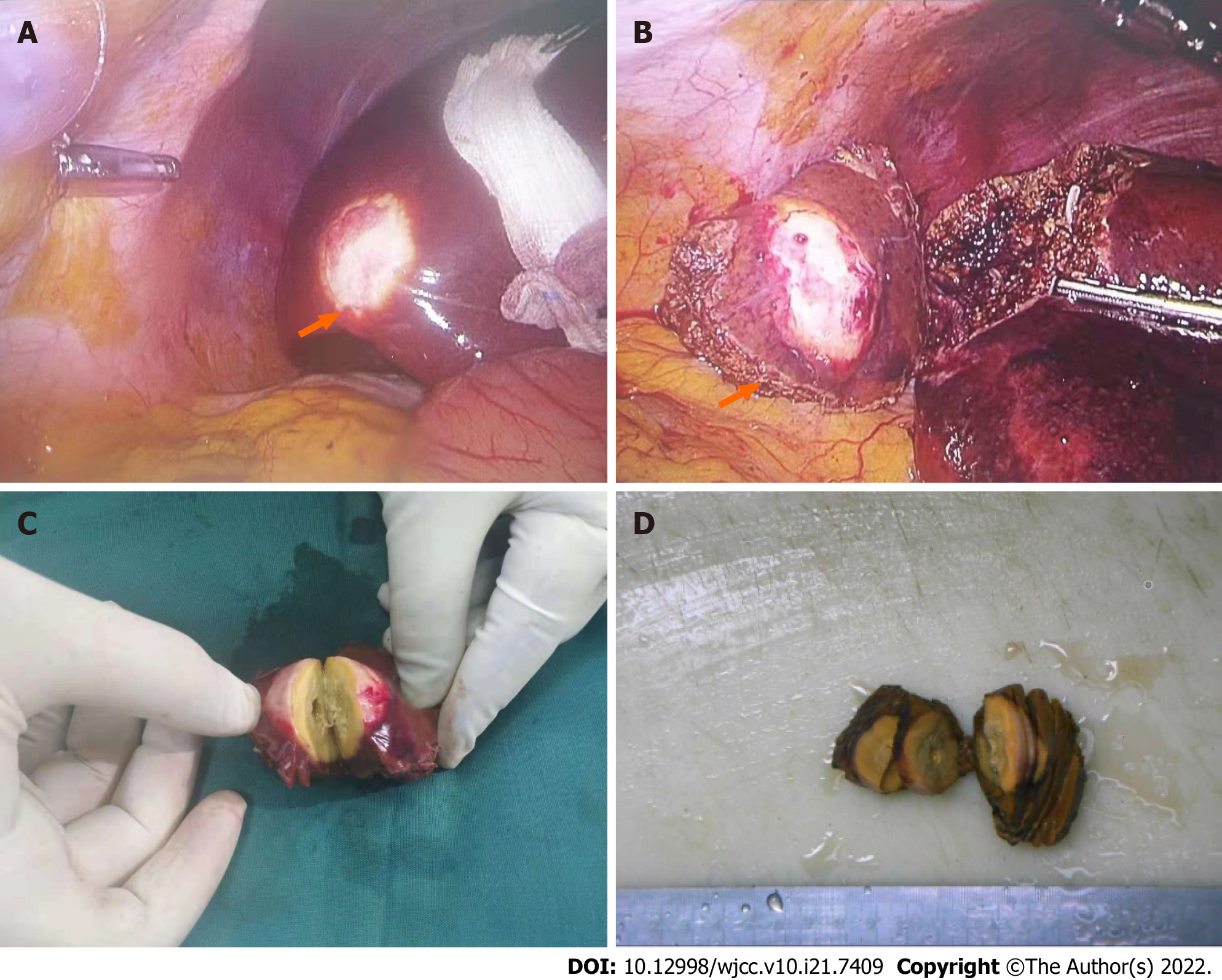
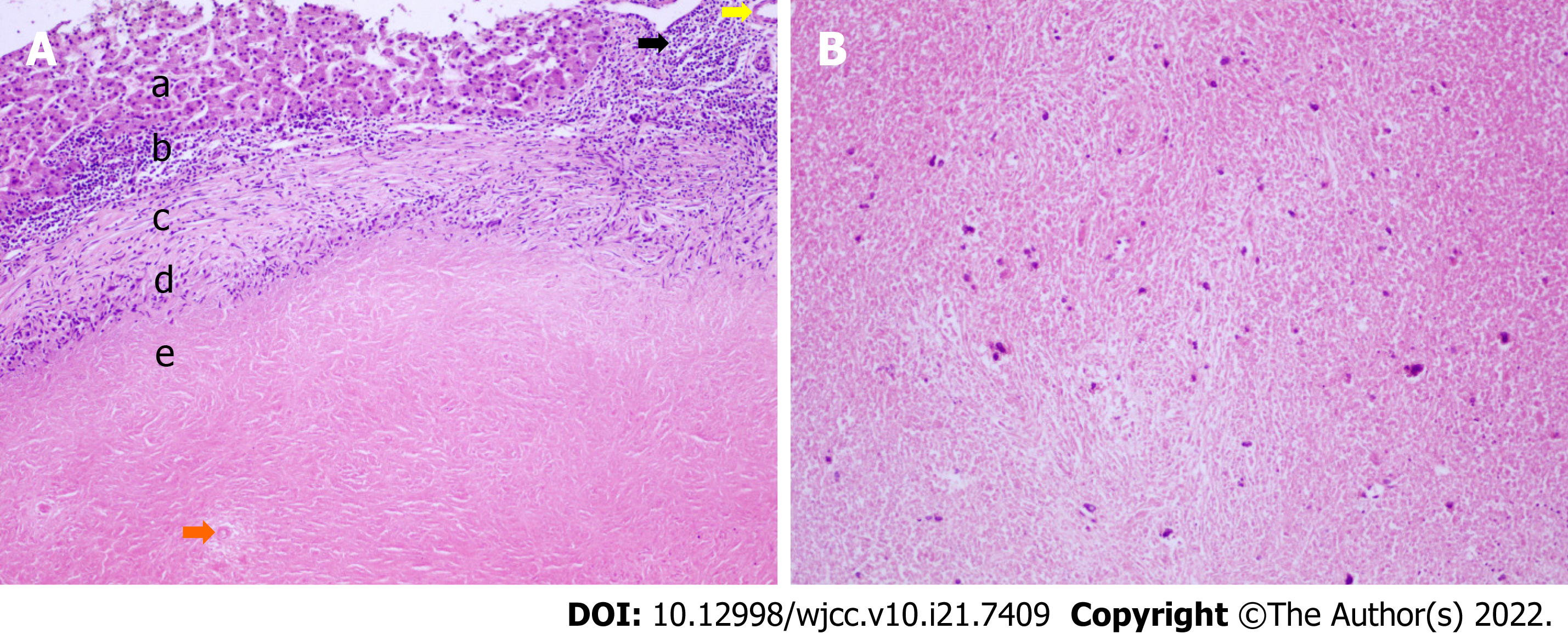
After undergoing laparoscopic hepatic space-occupying resection (Figure 2A and B), the patient recovered smoothly. Pathological examination after surgery revealed an irregular liver. A grayish yellow tough nodule measuring 4.2 cm × 3 cm × 2.9 cm was seen inside the lesion after incision (Figure 2C and D). It had a clear boundary with surrounding tissues. It invaded the liver capsule and was 0.4 cm near the resection surface. The remaining liver tissue was yellowish-brown and tough. Microscopically, there were necrotic nodules surrounded by dense fibers in the liver tissue. Many lymphocytes and histiocytes were surrounding the nodules. Immunohistochemical staining showed CD68 [tissue cell (+)], CK [liver tissue (+)], Hepatocyte [Hepatocyte (+)], CK19 [bile duct (+)], fungal immunofluorescence (-), and acid-fast mycobacterium fluorescence staining (-) (Figure 3). No granulomas, parasites, fungi, or atypical cells were found. The final diagnosis was SNNL.
The patient had a smooth postoperative recovery and no adverse events occurred. The postoperative computed tomography (CT) scan showed no abnormal manifestations on the 4th day after liver lesion resection (Figure 1E). The patient is currently healthy and is being followed (lasting for 27 mo).
SNNL, a rare entity, was first described by Shepherd and Lee[1] as a rare benign lesion[5,7-10]. The origin of solitary hepatic necrotic nodules remains controversial. The type of cells in or around the nodules can be explained by the following hypotheses: The presence of eosinophilic multinucleated cells will lead to the origin of parasites, while the presence of epithelioid cells may lead to the origin of tuberculosis; however, these hypotheses have never been confirmed[11]. At present, there are two main theories about the pathogenesis of SNNL. One is that the lesion is a result of trauma or previous parasite infection. The other one is related to the sclerosis evolution of hemangioma[2]. The persistence of necrotic material in the center of the nodule may be ascribed to the formation of a dense fibrotic wall, in which blood vessels are destroyed, thereby preventing their reabsorption[7]. Patients with SNNL are often asymptomatic.
Preoperative examination to identify liver diseases such as SNNL, liver metastases, hepatic tuberculosis, inflammatory pseudotumor, etc. has an important influence on the treatment option. Hypoechoic nodules normally appear on abdominal ultrasound of SNNL[12], hepatic parenchymal tuberculosis[13], and liver metastatic tumors. Ultrasound has certain limitations in the differential diagnosis of solitary liver nodules. Some literature shows that simple coagulation necrosis type SNNL is manifested by low-density or iso-density nodules with clear borders during plain and enhanced CT scans. There tends to be no enhancement in the SNNL lesion, but thin edge enhancement could be seen in this case, which may result from calcification[3-4]. Liver metastases appear as low-density foci on the plain CT scan, slightly lower density at the outer edge of the lesion during the enhancement phase and low density at the center of the lesion during the arterial phase. Liver inflammatory pseudotumor and liver parenchymal tuberculosis demonstrated low-density foci on CT, and there was calcification in the center of liver parenchymal tuberculosis. CT also has certain limitations in the differential diagnosis of solitary liver nodules. If SNNL is highly suspected, surgical resection should be avoided[8]. Because the appearance of SNNL overlaps with that of liver metastases, malignancy cannot be completely ruled out[4,14]. Therefore, liver biopsy cannot be performed on this lesion, and the pathological characteristics of the lesion should be determined after surgical resection. Some literature suggests that frequent calcification in the lesion is vital for the differential diagnosis of isolated necrotic nodules in the liver[15]. In this case, obvious "ring" circular calcification was found. Geng et al[16] reported that SNNL show a low signal or iso-signal with different degrees of necrosis changes on MRI, and T2WI can show variable signals. On enhanced MRI, there was no enhancement at all stages of SNNL. This patient did not undergo MRI examination.
The patient underwent laparoscopic hepatic space-occupying resection with wide margins. The histological feature of SNNL is the central necrotic core surrounded by a transparent fibrotic envelope. They are usually well-bounded from the surrounding liver and have a yellowish-white soft malleable solid center with hard white edge. Despite being often isolated, multiple necrotic nodules have been reported in the same patient. This case is consistent with related studies. The main pathological manifestation of SNNL is coagulative necrosis, with thin borders of surrounding collagen fibers, sparse monocytes, lymphocytes, plasma cells, inflammatory cells, and elastic fibers, and the central area is rough and patchy with cellular debris[5,9,14]. The pathological manifestation of this case was mainly transparent surrounding fibrotic sacs, lymphocytes, plasma cells, eosinophils, and a small amount of leukocyte infiltration. The calcification in the lesion plays an important role in the diagnosis of SNNL. SNNL is difficult to diagnose before surgery, especially in the case of tumors. Ultrasound-guided liver biopsy may be used to confirm the diagnosis, but it is less accurate than postoperative pathological diagnosis. Therefore, intraoperative and postoperative pathological examinations are the gold standards for the diagnosis of SNNL[10]. In the present case, the lesion was surgically resected and pathology revealed SNNL.
In conclusion, we report a case of SNNL with "ring"-like calcification. As SNNL is a rare lesion, there has been no previous similar literature or case reports. Since the manifestations of SNNL overlap with those of liver metastases, malignancy cannot be completely excluded[4,14], so the nature of the lesions needs to be determined through surgical treatment. The cause of SNNL remains unclear[1,2,11]. The patient described here has no history of parasitic infection, trauma, or tumor, yet has a history of systemic lupus erythematosus. Therefore, whether SNNL is related to rheumatic immune disease or pathological changes awaits further investigation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Haddadi S, Algeria; Yap RVC, Philippines A-Editor: Yao QG, China S-Editor: Xing YX L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Shepherd NA, Lee G. Solitary necrotic nodules of the liver simulating hepatic metastases. J Clin Pathol. 1983;36:1181-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 53] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Sundaresan M, Lyons B, Akosa AB. 'Solitary' necrotic nodules of the liver: an aetiology reaffirmed. Gut. 1991;32:1378-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Hwang JY, Lee JE, Jung MJ. A Challenging Case of Solitary Necrotic Nodules of the Liver Mimicking Hepatic Metastases: CT, MRI, and PET-CT Findings. J Belg Soc Radiol. 2020;104:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Wang LX, Liu K, Lin GW, Zhai RY. Solitary Necrotic Nodules of the Liver: Histology and Diagnosis with CT and MRI. Hepat Mon. 2012;12:e6212. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Zhou YM, Li B, Xu F, Wang B, Li DQ, Liu P, Yang JM. Clinical features of solitary necrotic nodule of the liver. Hepatobiliary Pancreat Dis Int. 2008;7:485-489. [PubMed] |
| 6. | Deniz K, Coban G. Solitary necrotic nodule of the liver: always benign? J Gastrointest Surg. 2010;14:536-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Tsui WM, Yuen RW, Chow LT, Tse CC. Solitary necrotic nodule of the liver: parasitic origin? J Clin Pathol. 1992;45:975-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Choi CS, Cho EY, Jeong JS, Im CJ, Yang BJ, Kim HC. Spontaneous regression of a solitary necrotic nodule of the liver. Hepatol Int. 2010;4:649-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Patti R, Cabibi D, Sparacello M, Di Vita G, Montalto G. Solitary necrotic nodule of the liver: different pathological findings express a different histogenesis. Case Rep Gastroenterol. 2008;2:149-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Imura S, Miyake K, Ikemoto T, Morine Y, Fujii M, Sano N, Shimada M. Rapid-growing solitary necrotic nodule of the liver. J Med Invest. 2006;53:325-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Goel G, Rao S, Khurana N, Sarda AK. Solitary Necrotic Nodule of Liver (SNNL): A Report of Two Cases. J Clin Diagn Res. 2014;8:115-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Francica G, Meloni MF, Riccardi L, de Sio I, Caturelli E, Terracciano F, Giangregorio F, Chiang J, Danzi R, Marra A, Niosi M, Ranalli TV, Pompili M. Contrast-Enhanced Ultrasound Findings in Patients with Rare Solitary Necrotic Nodule of the Liver - a Multicenter Report. Ultraschall Med. 2021;Aug 25.. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Ch'ng LS, Amzar H, Ghazali KC, Siam F. Imaging appearances of hepatic tuberculosis: experience with 12 patients. Clin Radiol. 2018;73:321.e11-321.e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Colagrande S, Paolucci ML, Messerini L, Schima W, Stadler A, Bartolotta TV, Vanzulli A, Brancatelli G. Solitary necrotic nodules of the liver: cross-sectional imaging findings and follow-up in nine patients. AJR Am J Roentgenol. 2008;191:1122-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Kondi-Pafiti AI, Grapsa DS, Kairi-Vasilatou ED, Voros DK, Smyrniotis VE. "Solitary" necrotic nodule of the liver: an enigmatic entity mimicking malignancy. Int J Gastrointest Cancer. 2006;37:74-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Geng L, Lin C, Huang B, Long XA, Dai BH, Cong WM, Yang JM. Solitary necrotic nodule of the liver: MR findings in 33 pathologically proved lesions. Eur J Radiol. 2012;81:623-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |